Abstract
Introduction
Impulse control disorders (ICDs) frequently occur in Parkinson’s disease (PD), and an early identification is essential to prevent severe psychosocial consequences. The Questionnaire for Impulsive-Compulsive Disorders in Parkinson’s Disease–Rating Scale (QUIP-RS) has been developed to evaluate the severity of ICDs along with a range of impulsive-compulsive behaviors (ICBs) in PD; however, its Italian version has not yet been validated.
Methods
One hundred consecutive outpatients with PD were administered an Italian version of the QUIP-RS and a brief neuropsychological assessment to evaluate global cognitive status and scales to measure depression, apathy and impulsive disorders. We evaluated the internal consistency, convergent and divergent validity, and factorial structure of QUIP-RS. We also explored the possible association between QUIP-RS scores and clinical factors and dopaminergic medication.
Results
Subsyndromal ICDs manifestations were observed in 54% of the patients, and one in four (22%) reported two or more ICDs or related behaviors. The QUIP-RS demonstrated good internal consistency (Cronbach’s alpha = 0.806) and construct validity, and its factorial structure reflected different ICDs and ICBs domains. No association emerged between QUIP-RS scores and the clinical aspects of PD and dopaminergic medication.
Conclusion
We provided, for the first time, an Italian translation of the QUIP-RS and demonstrated its feasibility in clinical and research settings. Severity of ICDs was independent of clinical factors and dopaminergic medication, underlining the need to adopt a broader perspective on their etiopathology in PD.
Similar content being viewed by others
Introduction
Impulse control disorders (ICDs) encompass a class of psychiatric disorders described as a failure to resist an impulse or temptation to perform a behavior harmful to either the self or others [1]. ICDs are characterized by a growing sense of tension or activation before committing the act and a sense of pleasure or “release” during and immediately after the act [2].
ICDs occur frequently in Parkinson’s disease (PD), with prevalence rates widely ranging from 3.5 to 42.8% [3,4,5], which likely reflect methodological differences in study designs, assessment methods (i.e., informant-based or patient-outcome, use of diagnostic interviews or screening questionnaires), and socio-cultural factors that influence the phenomenology of ICDs worldwide [6]. Different subtypes of ICDs have been reported in PD, including compulsive buying, pathological gambling, binge eating, and hypersexuality, along with a range of impulsive-compulsive behaviors (ICBs) such as punding, walkabout, hobbyism, and compulsive dopaminergic medication overuse, the latter also known as dopamine dysregulation syndrome (DDS) [7]. Although ICDs in PD are often explained as side effects of dopamine replacement therapies, especially dopamine agonists (DA) [8], their occurrence in PD (PD-ICD) has also been reported in the early stages of the disease in drug-naive patients [9]. Altered functioning of the mesocorticolimbic network seems to be responsible for ICDs [10, 11], with increased activity in the ventral striatum and orbitofrontal cortex (OFC) and decreased activity in the anterior cingulate cortex (ACC) strongly related to PD-ICD manifestations [12]. Moreover, ICDs are associated with more severe cognitive manifestations, particularly executive dysfunctions [13, 14], supporting the pivotal role of the prefrontal cortex in behavioral regulation in PD patients.
The clinical relevance and psychosocial consequences associated with ICDs strengthen the need for an efficient early detection of these disorders in PD. To fill this gap, Weintraub and colleagues [7] first developed a global screening instrument titled the Questionnaire for Impulsive-Compulsive Disorders in Parkinson’s Disease (QUIP) [15] for the diagnosis and screening of PD-ICD, and subsequently, the Questionnaire for Impulsive-Compulsive Disorders in Parkinson’s Disease - Rating Scale (QUIP-RS) [16], which allows quantification of the severity and evolution of both ICDs and ICBs.
The QUIP-RS has been tested and validated in numerous languages [17,18,19,20,21]; however, no study has provided and validated an Italian version. To this end, the present study aimed to provide and validate an Italian version of the QUIP-RS, providing its psychometric properties and exploring the possible associations between impulsive-compulsive disorders and clinical variables in an Italian PD population.
Materials and methods
Participants
One hundred consecutive PD outpatients were recruited from the Movement Disorders Unit of the IDC-Hermitage Capodimonte in Naples. Patients were included in the study if they met the following inclusion criteria: (i) diagnosis of idiopathic PD based on clinical diagnostic criteria [22], (ii) absence of other neurological and psychiatric conditions, and (iii) absence of cognitive impairment as measured by the Montreal Cognitive Assessment (indicated by a score above 15.5) [23].
Demographic variables such as age, sex, and education (i.e., years of formal education), as well as clinical data such as disease duration, stage of disease, and level of functional disability, assessed using the Hoehn and Yahr staging system (H&Y), and severity of motor symptoms assessed by part III of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS-III) were registered. As for dopaminergic medication, we calculated the total levodopa equivalent daily dose (LEDD) and the use of levodopa, DA, catechol-O-methyl transferase (COMT), and monoamine oxidase-B (MAO-B) alone.
The present study was approved by the Local Ethics Committee and performed according to the ethical standards of the Declaration of Helsinki and its later amendments. Participants provided informed consent, and the data were treated according to the current regulations.
Patients and methods
Patients were administered a brief behavioral assessment comprising the QUIP-RS, Beck Depression Inventory-II (BDI-II), Dimensional Apathy Scale (DAS), and a modified version of the Minnesota Impulsive Disorders Interview (MIDI).
The Italian version of QUIP-RS
The QUIP-RS is a self-completed or rater-administered rating scale developed to measure the frequency and severity of symptoms of four ICDs (pathological gambling, hypersexuality, compulsive buying, and compulsive eating) and three related disorders (hobbyism, punding, and DDS) over the preceding 4 weeks. For each disorder, the scale uses 4 questions rated on a 5-point Likert scale (from “Never” = 0 to “Very often” = 4) to evaluate commonly reported thoughts, urges and desires, difficulty in controlling behaviors, and deceptive behaviors associated with ICDs (e.g., lying, mounting debts, engaging in illegal acts) [16]. Scores for each ICD and related disorder range from 0 to 16 (higher scores indicate greater severity/frequency of symptoms), with a total QUIP-RS score ranging from 0 to 112.
All items comprising the original version of the QUIP-RS [16] were independently translated into Italian by two researchers (G.M. and C.V.), the different versions were compared, and a third arbitrator (G.S.) solved discrepancies to reach an agreement. The draft of the Italian version of the QUIP-RS was back-translated into English by a native English speaker with expertise in linguistics and psychology to test the linguistic and psychological equivalence of the two versions following the guidelines of Beaton et al. [24]. Subsequently, linguistic comprehensibility and readability were assessed and judged as adequate and equivalent to the original version by a preliminary group of 25 individuals (aged 18–65 years), and the translated version was proofread and approved by the developer of the original questionnaire (D.W.). The The Italian version of the QUIP-RS is presented in Supplementary Material 1.
Assessment
Patients were administered a modified version of the MIDI, a 36-item semi-structured clinical interview designed to assess the presence of impulsive disorders [25, 26]. Different screening modules are present for each ICD (compulsive buying, pathological gambling, excessive sexual behavior, compulsive eating, and punding behavior), evaluated using a general screening question and subsequent questions to evaluate the presence of ICD according to the DSM-IV-TR criteria [25].
The BDI-II is a 21-item self-report questionnaire developed to measure depressive symptomatology [27]. Participants were required to select the most appropriate statement to describe their mood during the previous 2 weeks. Statements are organized according to the severity of their content on a 4-point scale from a minimum of 0 points to a maximum of 3, with higher scores indicating greater severity of depressive symptoms.
The DAS is a 24-item scale used to measure the multidimensional nature of apathy [28]. It consists of different subscales to assess executive, emotional, and behavioral initiation apathy, with each item rated on a 4-point Likert scale. The DAS total score ranges from 0 to 72, with higher scores indicating more severe apathy.
All questionnaires and QUIP-RS were rater-administered.
Statistics
Acceptability of the QUIP-RS was defined as appropriate in the absence of missing values, following previous studies on the standardization of behavioral scales [27, 29,30,31]. Floor and ceiling effects were also analyzed. Non-parametric statistics were used because of the non-normality of QUIP-RS total score, i.e., skewness and kurtosis values exceeding |2|.
Internal consistency was tested via Cronbach’s α coefficient. Principal component analysis (PCA) with direct OBLIMIN rotation was used to evaluate the factorial structure of the scale. We employed the Mineigen criterion (eigenvalues > 1), together with inspection of the scree plot, to determine the number of factors to be extracted.
Convergent validity was assessed between the QUIP-RS and MIDI total scores, while divergent validity was evaluated by the correlation between the QUIP-RS total score and the BDI-II and DAS total scores. The potential association between demographic (i.e., age and educational level) and clinical factors (i.e., UPDRS-III, disease duration, and medication) and total QUIP-RS score was evaluated using Spearman’s correlation. Sex differences in QUIP-RS scores were assessed using the Mann-Whitney U test.
Statistical analyses were performed using IBM SPSS Statistics version 26.
Results
Our final sample comprised 100 PD patients (62% males), aged 67.45 ± 9.63 years with a mean disease duration of 9.91 ± 4.78 (Table 1).
QUIP-RS scores in PD population
We considered the QUIP-RS total score for the investigation of floor and ceiling effects; the floor effect (score 0) was observed in 46% of the sample, but no ceiling effect was observed.
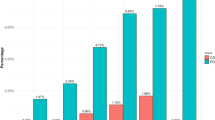
Fifty-four patients were screened as positive (≥ 1, subclinical ICDs and ICD-related disorders) for at least one impulsive-compulsive disorder (54%), and 22% reported two or more ICDs or related behaviors (Fig. 1). Particularly, hobbyism/punding and compulsive eating were the most frequent domains within PD+ICD single domain, whereas DDS was more common within PD+ICD multiple domains (Fig. 1). Considering the whole sample, hobbyism/punding was the most frequently reported symptom (21%), followed by DDS (20%), compulsive eating (16%), hypersexuality (15%), pathological gambling (13%), and compulsive buying (10%). Considering the recommended cut-off scores proposed by Weintraub and colleagues [16], 11 PD patients (11%) were classified as having ICDs, and among these, compulsive eating was observed in 9%, pathological gambling in 6%, hypersexuality in 3%, and compulsive buying in 2%. Regarding ICD-related disorders, 12 patients (12%) reported a score above the cut-off for hobbyism/punding, whereas no cut-off was previously established for the DDS domain.
Pie charts displaying percentages of the prevalence of impulse control disorder and related behavior (ICDs) in Parkinson’s disease (PD+ICD) according to the QUIP-RS. In detail, on the right, the frequencies of specific ICDs and related behaviors within PD+ICD single and multiple domains. Note that percentages of specific ICDs and related behaviors within PD+ICD multiple domains chart exceed 100% due to comorbidity
Internal consistency and exploratory factor analysis
The QUIP-RS demonstrated good internal consistency (Cronbach’s α = 0.806) (Table 2). A seven-factor solution with an explained variance of 80.55% was generated by PCA with direct OBLIMIN rotation using the Mineigen criterion (eigenvalues > 1; Table 3) and was confirmed by inspection of the scree plot. This structure substantially reflected the items’ classification of different impulsive, compulsive, and related disorders: the first factor loaded under items evaluating hobbyism (explained variance = 18.70%), the second factor included items assessing compulsive eating (explained variance = 15.76%), and the third factor comprised items evaluating compulsive buying (explained variance = 13.43%). The fourth, fifth, sixth, and seventh factors included items assessing pathological gambling (explained variance = 10.96%), hypersexuality (explained variance = 9.07%), use of PD medication (explained variance = 7.57%), and punding (explained variance = 5.06%), respectively. The question of deceptive behaviors associated with punding behavior was initially loaded under the hobbyism factor, but it could be placed within the punding factor because of a lower factor based on the suitability of the content.
Validity
Convergent validity was demonstrated by a moderate correlation between the QUIP-RS and MIDI total scores (rs = 0.509, p < 0.001), whereas divergent validity was demonstrated by the absence of an association between the QUIP-RS total score and the BDI-II (rs = 0.129, p = 0.240) and DAS total scores (rs = −0.084, p = 0.445).
Associations with demographic and clinical factors
The QUIP-RS total score was not associated with age (rs = −0.119, p = 0.259), educational level (rs = −0.046, p = 0.669), or sex (U = 1143.000, p = 0.793). As for clinical variables, the QUIP-RS total score was not related to disease duration (rs = −0.071, p = 0.537), H&Y stage (rs = −0.068, p = 0.586), and UPDRS-III (rs = 0.070, p = 0.590). Considering PD medication, no associations emerged between the QUIP-RS total score and the LEDD total score (rs = 0.100, p = 0.388), amount of daily levodopa alone (rs = 0.229, p = 0.102), amount of DA alone (rs = 0.059, p = 0.606), doses of COMT inhibitors alone (rs = 0.126, p = 0.373), and doses of MAO inhibitors alone (rs = −0.053, p = 0.711).
Discussion
The present study provided the first Italian version of the QUIP-RS and demonstrated its validity and reliability for the assessment of ICDs and related disorders in patients with PD. Fifty-four percent of the patients were screened as positive considering the subsyndromal manifestations, with hobbyism/punding (21%) and DDS (20%) emerging as the most frequent symptoms. Only 11% of the patients were classified as having PD-ICD, according to the recommended cut-off scores [16].
Although the percentages of ICDs such as pathological gambling, compulsive eating, hypersexuality, and compulsive buying partially overlapped with those reported in previous studies [17, 18], we found a higher percentage of patients complaining of ICD-related behaviors such as punding and DDS. The nature of the relationship between hobbyism and punding remains unclear because they may represent a unique neurobiological entity. Patients seem to be aware but unable to reduce the time spent on the execution of repetitive, excessive, and non-goal-directed behaviors and become irritable when distracted from them, possibly leading to isolation from or conflict with other people [32, 33]. Punding has been associated with a pattern of compulsive medication overuse defined by Giovannoni [34] as the inability to stop dopaminergic replacement therapy (DRT) intake to alleviate motor impairment, which instead produces intoxication and severe dyskinesias. Although 20% of patients obtained a score ≥ 1 in the DDS domain of the QUIP, most complained of frequent thoughts (18%) and urges and desires (13%) to take medication rather than a pattern of pathological use and overdosing of DRT (reported by 7% of patients), which is essential for the definition of DDS [34]. Therefore, it is possible to hypothesize that the high percentage of patients with DDS does not reflect an actual high prevalence of this comorbidity that, instead, can be due to anxiety-related mechanisms driven by off-period dysphoria [35] and then triggered by patients’ perception that the “ON” phase is fading away.
Furthermore, the Italian version of the QUIP-RS demonstrated good internal consistency, and a seven-factor structure was revealed by factor analysis reflecting seven ICD domains: hobbyism, compulsive eating, compulsive shopping, DDS, pathological gambling, punding, and hypersexuality. The only exception in the partition of items into factors was represented by the item assessing the engagement in activities for maintaining punding behavior that loaded into the hobbyism factor. However, this result further confirms the hypothesis that hobbyism and punding may be combined to form a single diagnosis [16].
Convergent and divergent validity were demonstrated by our correlational results, revealing a strong positive association of the QUIP-RS with the MIDI and the absence of a relationship with scales assessing depression and apathy. Indeed, the MIDI was originally developed for use in adults and represents a valuable interview tool for ICDs in clinical and research settings [26]; however, it neglects some ICD-related manifestations, such as hobbyism and DDS, whose assessment has been included in the QUIP-RS, designed to cover the whole range of ICDs and related behaviors reported in PD [16].
Although some studies have provided evidence of a link between ICDs and neuropsychiatric disorders set on the opposite extreme of the motivated behavior continuum, such as apathy and depression, these disorders may rarely co-occur [36, 37], that may explain the absence of relationships in our study.
Interestingly, the QUIP-RS score was independent of the PD-related processes and DRT. Although some studies have shown that ICDs are more prevalent in young unmarried male subjects and in patients with a longer disease duration [38] as an adverse effect of DA use in PD [39], recent findings have shown that the mere contribution of DA intake and other clinical factors does not fully explain the pathophysiology and prognosis of ICDs in PD [8, 40, 41]. First, it should be noted that the current clinical approach in planning DRT posology promotes the use of extended-release formulations that allow the maintenance of more stable drug concentrations and lower DA dosages to minimize the risk of ICD development and subsequent medical-legal issues [8, 40, 42]. In addition, personality profiles characterized by impulsiveness and novelty seeking, or a family history of substance use disorders, represent risk factors for the development of ICDs [43]. At the same time, biological sex may also influence the development of specific ICDs with male patients being more prone to hypersexuality and eating disorders, whereas compulsive shopping is more common among female patients [38]. Finally, it should be considered that some types of ICDs are also affected by cultural, religious, and socioeconomic factors (e.g., pathological gambling is likely to be less prevalent or underreported in India and China, as public gambling or casino visiting is not a socially accepted habit in these countries) [38]. Taken together, these findings suggest adopting a broader perspective on the etiopathology of ICDs, whose occurrence seems to result from the interaction between personality traits, sex, cultural factors, neuropathological processes, and DRT impact [8, 40, 41].
However, the present study presents some limitations. First, the QUIP-RS was administered to patients, which can limit our results because patients may be unaware of the clinical significance of their symptoms or may hide or not report undesirable behaviors due to embarrassment or sociocultural factors leading to underdiagnosis and undertreatment [44, 45]. Future studies should also ascertain the presence of ICDs using an informant version of the QUIP-RS to avoid delays in diagnosis and therapeutic interventions [45]. Moreover, further studies are needed to determine the inter-rater and test-retest reliability of the Italian version of the QUIP-RS and to investigate its sensitivity to symptom changes after therapeutic interventions.
In conclusion, this study demonstrated that the Italian version of the QUIP-RS represents the most appropriate alternative for the evaluation of ICDs in parkinsonian syndromes compared to other behavioral assessments previously available within the Italian scenario [46]. Indeed, it has proven to be a comprehensive, reliable, and valid screening instrument for ICDs and related behaviors, and its adoption is recommended in PD population for both research and clinical purposes.
Data availability
Datasets associated with the present study are available upon reasonable request of interested researchers.
References
(2013) Diagnostic and statistical manual of mental disorders, 5th
Latella D, Maggio MG, Maresca G et al (2019) Impulse control disorders in Parkinson’s disease: a systematic review on risk factors and pathophysiology. J Neurol Sci 398. https://doi.org/10.1016/j.jns.2019.01.034
Antonini A, Barone P, Bonuccelli U et al (2017) ICARUS study: prevalence and clinical features of impulse control disorders in Parkinson’s disease. J Neurol Neurosurg Psychiatry 88. https://doi.org/10.1136/jnnp-2016-315277
Callesen MB, Weintraub D, Damholdt MF, Møller A (2014) Impulsive and compulsive behaviors among Danish patients with Parkinson’s disease: prevalence, depression, and personality. Parkinsonism Relat Disord 20. https://doi.org/10.1016/j.parkreldis.2013.09.006
Weintraub D, Koester J, Potenza MN et al (2010) Impulse control disorders in Parkinson disease: a cross-sectional study of 3090 patients. Arch Neurol. https://doi.org/10.1001/archneurol.2010.65
Parra-Díaz P, Chico-García JL, Beltrán-Corbellini Á et al (2021) Does the country make a difference in impulse control disorders? A systematic review. Mov Disord Clin Pract 8. https://doi.org/10.1002/mdc3.13128
Weintraub D, David AS, Evans AH et al (2015) Clinical spectrum of impulse control disorders in Parkinson’s disease. Mov Disord 30. https://doi.org/10.1002/mds.26016
Vitale C, Amboni M, Erro R et al (2019) Parkinson’s disease management and impulse control disorders: current state and future perspectives. Expert Rev Neurother 19. https://doi.org/10.1080/14737175.2019.1620603
Weintraub D, Papay K, Siderowf A (2013) Screening for impulse control symptoms in patients with de novo Parkinson disease: a case control study. Neurology. https://doi.org/10.1212/WNL.0b013e31827b915c
Zhang JF, Wang XX, Feng Y et al (2021) Impulse control disorders in Parkinson’s disease: epidemiology, pathogenesis and therapeutic strategies. Front. Psychiatry 12. https://doi.org/10.3389/fpsyt.2021.635494
Tessitore A, Santangelo G, De Micco R et al (2016) Cortical thickness changes in patients with Parkinson’s disease and impulse control disorders. Parkinsonism Relat Disord. https://doi.org/10.1016/j.parkreldis.2015.10.013
Santangelo G, Raimo S, Cropano M et al (2019) Neural bases of impulse control disorders in Parkinson’s disease: a systematic review and an ALE meta-analysis. Neurosci Biobehav Rev. https://doi.org/10.1016/j.neubiorev.2019.09.041
Santangelo G, Raimo S, Barone P (2017) The relationship between impulse control disorders and cognitive dysfunctions in Parkinson’s disease: a meta-analysis. Neurosci Biobehav Rev 77:129–147
Vitale C, Santangelo G, Trojano L et al (2011) Comparative neuropsychological profile of pathological gambling, hypersexuality, and compulsive eating in Parkinson’s disease. Mov Disord. https://doi.org/10.1002/mds.23567
Weintraub D, Hoops S, Shea JA et al (2009) Validation of the Questionnaire for Impulsive-Compulsive Disorders in Parkinson’s Disease. Mov Disord 24. https://doi.org/10.1002/mds.22571
Weintraub D, Mamikonyan E, Papay K et al (2012) Questionnaire For Impulsive-Compulsive Disorders in Parkinson’s Disease-Rating Scale. Mov Disord 27:242–247. https://doi.org/10.1002/mds.24023
Krieger DM, Cardoso SV, Caumo W et al (2017) Parkinson’s disease impulsive-compulsive disorders questionnaire - current short (QUIP-CS) - translation and validation of content of Portuguese version. J Bras Psiquiatr 66. https://doi.org/10.1590/0047-2085000000158
Probst CC, Winter LM, Möller B et al (2014) Validation of the Questionnaire for Impulsive-Compulsive Disorders in Parkinson’s Disease (QUIP) and the QUIP-rating scale in a German speaking sample. J Neurol 261. https://doi.org/10.1007/s00415-014-7299-6
Marques A, Vidal T, Pereira B et al (2019) French validation of the Questionnaire for Impulsive-Compulsive Disorders in Parkinson’s Disease–Rating Scale (QUIP-RS). Parkinsonism Relat Disord 63. https://doi.org/10.1016/j.parkreldis.2019.02.026
Choi JH, Lee JY, Cho JW et al (2020) Validation of the Korean version of the Questionnaire for Impulsive-Compulsive Disorders in Parkinson’s Disease Rating Scale. J Clin Neurol 16. https://doi.org/10.3988/jcn.2020.16.2.245
Xu T, Cao L, Long W, Zhao G (2021) Validation of the Chinese version of the Questionnaire For Impulsive-Compulsive Disorders in Parkinson’s Disease. Front Neurol 12. https://doi.org/10.3389/fneur.2021.731552
Postuma RB, Berg D, Stern M et al (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30:1591–1601
Santangelo G, Siciliano M, Pedone R et al (2015) Normative data for the Montreal Cognitive Assessment in an Italian population sample. Neurol Sci. https://doi.org/10.1007/s10072-014-1995-y
Beaton DE, Bombardier C, Guillemin F, Ferraz MB (2000) Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976) 25. https://doi.org/10.1097/00007632-200012150-00014
Adam P, Richoux C, Lejoyeux M (2008) Screening for impulse control disorders among patients admitted to a French psychiatric emergency service~!2008-09-16~!2008-11-06~!2008-11-28~! Open Psychiatr J 2. https://doi.org/10.2174/1874354400802010030
Chamberlain SR, Grant JE (2018) Minnesota Impulse Disorders Interview (MIDI): validation of a structured diagnostic clinical interview for impulse control disorders in an enriched community sample. Psychiatry Res 265. https://doi.org/10.1016/j.psychres.2018.05.006
Maggi G, D’Iorio A, Aiello EN et al (2023) Psychometrics and diagnostics of the Italian version of the Beck Depression Inventory-II (BDI-II) in Parkinson’s disease. Neurol Sci. https://doi.org/10.1007/s10072-023-06619-w
Santangelo G, D’Iorio A, Piscopo F et al (2017) Assessment of apathy minimising the effect of motor dysfunctions in Parkinson’s disease: a validation study of the dimensional apathy scale. Qual Life Res. https://doi.org/10.1007/s11136-017-1569-6
Maggi G, Altieri M, Ilardi CR, Santangelo G (2022) Validation of a short Italian version of the Barratt Impulsiveness Scale (BIS-15) in non-clinical subjects: psychometric properties and normative data. Neurol Sci. https://doi.org/10.1007/s10072-022-06047-2
Altieri M, Maggi G, Rippa V, Santangelo G (2023) Evaluation of apathy in non-clinical populations: validation, psychometric properties, and normative data of the Italian version of apathy-motivation index (AMI). Neurol Sci. https://doi.org/10.1007/s10072-023-06774-0
Altieri M, Maggi G, Giacobbe C, Santangelo G (2023) Psychometric properties and normative data of the Italian version of the Cognitive Function at Work Questionnaire: a screening tool for detecting subjective cognitive complaints at work. Neurol Sci. https://doi.org/10.1007/s10072-023-07265-y
Evans AH, Katzenschlager R, Paviour D et al (2004) Punding in Parkinson’s disease: Its relation to the dopamine dysregulation syndrome. Mov Disord 19. https://doi.org/10.1002/mds.20045
Rajalingam R, Fasano A (2023) Punding in Parkinson’s disease: an update. Mov Disord Clin Pract. https://doi.org/10.1002/mdc3.13748
Giovannoni G, O’Sullivan JD, Turner K et al (2000) Hedonistic homeostatic dysregulation in patients with Parkinson’s disease on dopamine replacement therapies. J Neurol Neurosurg Psychiatry 68. https://doi.org/10.1136/jnnp.68.4.423
Okai D, Samuel M, Askey-Jones S et al (2011) Impulse control disorders and dopamine dysregulation in Parkinson’s disease: a broader conceptual framework. Eur J Neurol 18. https://doi.org/10.1111/j.1468-1331.2011.03432.x
Sinha N, Manohar S, Husain M (2013) Impulsivity and apathy in Parkinson’s disease. J Neuropsychol. https://doi.org/10.1111/jnp.12013
Maggi G, Loayza F, Vitale C et al (2024) Anatomical correlates of apathy and impulsivity co-occurrence in early Parkinson’s disease. J Neurol (In press)
Bhattacharjee S (2018) Impulse control disorders in Parkinson’s disease: review of pathophysiology, epidemiology, clinical features, management, and future challenges. Neurol India 66. https://doi.org/10.4103/0028-3886.237019
Joutsa J, Martikainen K, Vahlberg T, Kaasinen V (2012) Effects of dopamine agonist dose and gender on the prognosis of impulse control disorders in Parkinson’s disease. Parkinsonism Relat Disord 18. https://doi.org/10.1016/j.parkreldis.2012.06.005
Contin M, Lopane G, Marini L et al (2023) Screening for impulse control disorders in Parkinson’s disease and dopamine agonist use: a study of pharmacokinetic and psychological risk factors. Neurol Sci 44. https://doi.org/10.1007/s10072-022-06485-y
Gunduz A, Çiftçi T, Erbil AC et al (2023) Impulse control disorders in Parkinson’s disease: a retrospective analysis of 1824 patients in a 12-year period. Neurol Sci. https://doi.org/10.1007/s10072-023-07006-1
Rizos A, Sauerbier A, Antonini A et al (2016) A European multicentre survey of impulse control behaviours in Parkinson’s disease patients treated with short- and long-acting dopamine agonists. Eur J Neurol 23. https://doi.org/10.1111/ene.13034
Maréchal E, Denoiseux B, Thys E et al (2015) Impulse control disorders in Parkinson’s disease: an overview from neurobiology to treatment. J Neurol 262. https://doi.org/10.1007/s00415-014-7361-4
Papay K, Mamikonyan E, Siderowf AD et al (2011) Patient versus informant reporting of ICD symptoms in Parkinson’s disease using the QUIP: validity and variability. Parkinsonism Relat Disord 17. https://doi.org/10.1016/j.parkreldis.2010.11.015
Maggi G, Vitale C, Delle Curti A et al (2023) Unawareness of apathy in Parkinson’s disease: the role of executive dysfunction on symptom recognition. Brain Sci 13. https://doi.org/10.3390/brainsci13060964
Aiello EN, D’Iorio A, Montemurro S et al (2022) Psychometrics, diagnostics and usability of Italian tools assessing behavioural and functional outcomes in neurological, geriatric and psychiatric disorders: a systematic review. Neurol Sci 43. https://doi.org/10.1007/s10072-022-06300-8
Acknowledgements
None.
Funding
Open access funding provided by Università degli Studi della Campania Luigi Vanvitelli within the CRUI-CARE Agreement. Research is partially supported by the Italian Ministry of Health.
University of Campania “Luigi Vanvitelli” joined the Italy Transformative Agreement for the funding about article processing charge (APC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Participants provided informed consent. This study was approved by the Local Ethics Committees.
Conflict of interest
The authors declare no competing interests.
Additional information
University of Pennsylvania holds the copyright to the QUIP-RS and QUIP, so a licensing agreement with Penn is required for its use in any language, which is without cost for academic use.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Gianpaolo Maggi and Carmine Vitale share co-first authorship.
Supplementary information
ESM 1
(DOCX 22 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maggi, G., Vitale, C., Giacobbe, C. et al. Validation of the Italian version of the Questionnaire for Impulsive-Compulsive Disorders in Parkinson’s Disease-Rating Scale (QUIP-RS) in an Italian Parkinson’s disease cohort. Neurol Sci (2024). https://doi.org/10.1007/s10072-024-07304-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10072-024-07304-2