Abstract
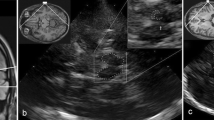
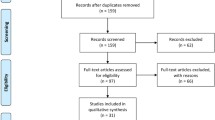
Progressive supranuclear palsy (PSP) is an atypical parkinsonism that presents with different phenotypes. There are still no validated diagnostic biomarkers for early diagnosis of PSP. Transcranial sonography (TCS) is a promising tool in the differential diagnosis of parkinsonian disorders; however, there are no systematic investigations about the application of TCS in PSP patients. Therefore, we performed a systematic review and meta-analysis to discuss the role of TCS in diagnosing PSP by systematically searching PubMed, Cochrane Library, Chinese National Knowledge Infrastructure and Wan Fang databases. Of 66 obtained records, 16 articles, including 366 patients with PSP, were included. Our results showed the estimated random-effects pooled prevalence of substantia nigra hyperechogenicity in patients with PSP was 22% (95% CI 12–32%), lenticular nucleus hyperechogenicity was 70% (95% CI 52–82%), and enlarged third ventricle was 71% (95% CI 55–85%). Additionally, a normal echogenicity substantia nigra in TCS showed 70% sensitivity (95% CI 56–81%) and 86% specificity (95% CI 75–86%) to differentiate PSP from Parkinson’s disease. In conclusion, TCS is an important supplementary biomarker for diagnosing PSP. At the same time, the diagnostic value of TCS in discriminating PSP from other atypical parkinsonism and between different PSP phenotypes needs further exploration.







Similar content being viewed by others
References
Lukic MJ, Respondek G, Kurz C et al (2022) Long-Duration Progressive Supranuclear Palsy: Clinical Course and Pathological Underpinnings. Ann Neurol 92:637–649. https://doi.org/10.1002/ana.26455
Kovacs GG, Lukic MJ, Irwin DJ et al (2020) Distribution patterns of tau pathology in progressive supranuclear palsy. Acta Neuropathol 140:99–119. https://doi.org/10.1007/s00401-020-02158-2
Giagkou N, Hoglinger GU, Stamelou M (2019) Progressive supranuclear palsy. Int Rev Neurobiol 149:49–86. https://doi.org/10.1016/bs.irn.2019.10.013
Respondek G, Stamelou M, Kurz C et al (2014) The phenotypic spectrum of progressive supranuclear palsy: a retrospective multicenter study of 100 definite cases. Mov Disord 29:1758–1766. https://doi.org/10.1002/mds.26054
Höglinger GU, Respondek G, Stamelou M et al (2017) Clinical diagnosis of progressive supranuclear palsy: The movement disorder society criteria. Mov Disord 32:853–864. https://doi.org/10.1002/mds.26987
Ali F, Martin PR, Botha H et al (2019) Sensitivity and Specificity of Diagnostic Criteria for Progressive Supranuclear Palsy. Mov Disord 34:1144–1153. https://doi.org/10.1002/mds.27619
Armstrong MJ (2018) Progressive Supranuclear Palsy: an Update. Curr Neurol Neurosci Rep 18:12. https://doi.org/10.1007/s11910-018-0819-5
Coughlin DG, Litvan I (2020) Progressive supranuclear palsy: Advances in diagnosis and management. Parkinsonism Relat Disord 73:105–116. https://doi.org/10.1016/j.parkreldis.2020.04.014
Alster P, Madetko N, Koziorowski D et al (2020) Progressive Supranuclear Palsy-Parkinsonism Predominant (PSP-P)-A Clinical Challenge at the Boundaries of PSP and Parkinson's Disease (PD). Front Neurol 11:180. https://doi.org/10.3389/fneur.2020.00180
Stamelou M, Giagkou N, Höglinger GU (2019) One decade ago, one decade ahead in progressive supranuclear palsy. Mov Disord 34:1284–1293. https://doi.org/10.1002/mds.27788
Picillo M, Tepedino MF, Abate F et al (2020) Midbrain MRI assessments in progressive supranuclear palsy subtypes. J Neurol Neurosurg Psychiatry 91:98–103. https://doi.org/10.1136/jnnp-2019-321354
Shafieesabet A, Fereshtehnejad SM, Shafieesabet A et al (2017) Hyperechogenicity of substantia nigra for differential diagnosis of Parkinson's disease: A meta-analysis. Parkinsonism Relat Disord 42:1–11. https://doi.org/10.1016/j.parkreldis.2017.06.006
Becker G, Seufert J, Bogdahn U et al (1995) Degeneration of substantia nigra in chronic Parkinson's disease visualized by transcranial color-coded real-time sonography. Neurology 45:182–184. https://doi.org/10.1212/wnl.45.1.182
Mei YL, Yang J, Wu ZR et al (2021) Transcranial Sonography of the Substantia Nigra for the Differential Diagnosis of Parkinson's Disease and Other Movement Disorders: A Meta-Analysis. Parkinsons Dis 2021:8891874. https://doi.org/10.1155/2021/8891874
Richter D, Katsanos AH, Schroeder C et al (2019) Lentiform Nucleus Hyperechogenicity in Parkinsonian Syndromes: A Systematic Review and Meta-Analysis with Consideration of Molecular Pathology. Cells 9. https://doi.org/10.3390/cells9010002
Heim B, Peball M, Hammermeister J et al (2022) Differentiating Parkinson's Disease from Essential Tremor Using Transcranial Sonography: A Systematic Review and Meta-Analysis. J Parkinsons Dis 12:1115–1123. https://doi.org/10.3233/JPD-213012
Bouwmans AEP, Vlaar AMM, Srulijes K et al (2010) Transcranial sonography for the discrimination of idiopathic Parkinson's disease from the atypical parkinsonian syndromes. Int Rev Neurobiol 90:121–146. https://doi.org/10.1016/S0074-7742(10)90009-3
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
Whiting PF, Rutjes AWS, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Hellwig S, Reinhard M, Amtage F et al (2014) Transcranial sonography and [18F]fluorodeoxyglucose positron emission tomography for the differential diagnosis of parkinsonism: a head-to-head comparison. Eur J Neurol 21:860–866. https://doi.org/10.1111/ene.12394
Liboni W, Pignatta P, Salzedo E et al (2011) Ultrasonography and MR Imaging in Progressive Supranuclear Palsy. Neuroradiol J 24:221–225. https://doi.org/10.1177/197140091102400209
Gaenslen A, Unmuth B, Godau J et al (2008) The specificity and sensitivity of transcranial ultrasound in the differential diagnosis of Parkinson's disease: a prospective blinded study. The Lancet Neurology 7:417–424. https://doi.org/10.1016/s1474-4422(08)70067-x
Walter U, Niehaus L, Probst T et al (2003) Brain parenchyma sonography discriminates Parkinson's disease and atypical parkinsonian syndromes. Neurology 60:74–77. https://doi.org/10.1212/wnl.60.1.74
Walter U, Dressler D, Wolters A et al (2004) Sonographic discrimination of corticobasal degeneration vs progressive supranuclear palsy. Neurology 63:504–509. https://doi.org/10.1212/01.wnl.0000133006.17909.32
Walter U, Dressler D, Probst T et al (2007) Transcranial brain sonography findings in discriminating between parkinsonism and idiopathic Parkinson disease. Arch Neurol 64:1635–1640. https://doi.org/10.1001/archneur.64.11.1635
Behnke S, Berg D, Naumann M et al (2005) Differentiation of Parkinson's disease and atypical parkinsonian syndromes by transcranial ultrasound. J Neurol Neurosurg Psychiatry 76:423–425. https://doi.org/10.1136/jnnp.2004.049221
Okawa M, Miwa H, Kajimoto Y et al (2007) Transcranial sonography of the substantia nigra in Japanese patients with Parkinson's disease or atypical parkinsonism: clinical potential and limitations. Intern Med 46:1527–1531. https://doi.org/10.2169/internalmedicine.46.0271
Ebentheuer J, Canelo M, Trautmann E et al (2010) Substantia nigra echogenicity in progressive supranuclear palsy. Mov Disord 25:773–777. https://doi.org/10.1002/mds.22981
Kostić VS, Mijajlović M, Smajlović D et al (2013) Transcranial brain sonography findings in two main variants of progressive supranuclear palsy. Eur J Neurol 20:552–557. https://doi.org/10.1111/ene.12034
Sastre-Bataller I, Vázquez JF, Martínez-Torres I et al (2013) Mesencephalic area measured by transcranial sonography in the differential diagnosis of parkinsonism. Parkinsonism Relat Disord 19:732–736. https://doi.org/10.1016/j.parkreldis.2013.04.010
Bartova P, Kraft O, Bernatek J et al (2014) Transcranial sonography and (123)I-FP-CIT single photon emission computed tomography in movement disorders. Ultrasound Med Biol 40:2365–2371. https://doi.org/10.1016/j.ultrasmedbio.2014.05.014
Sadowski K, Serafin-Król M, Szlachta K et al (2015) Basal ganglia echogenicity in tauopathies. J Neural Transm (Vienna) 122:863–865. https://doi.org/10.1007/s00702-014-1310-3
Sanzaro E, Iemolo F (2016) Transcranial sonography in movement disorders: an interesting tool for diagnostic perspectives. Neurol Sci 37:373–376. https://doi.org/10.1007/s10072-015-2424-6
Fujita H, Suzuki K, Numao A et al (2016) Usefulness of Cardiac MIBG Scintigraphy, Olfactory Testing and Substantia Nigra Hyperechogenicity as Additional Diagnostic Markers for Distinguishing between Parkinson's Disease and Atypical Parkinsonian Syndromes. PLoS One 11:e0165869. https://doi.org/10.1371/journal.pone.0165869
Alonso-Canovas A, Tembl Ferrairó JI, Martínez-Torres I et al (2019) Transcranial sonography in atypical parkinsonism: How reliable is it in real clinical practice? A multicentre comprehensive study. Parkinsonism Relat Disord 68:40–45. https://doi.org/10.1016/j.parkreldis.2019.09.032
Ghourchian S, Mousavi A, Zamani B et al (2019) Midbrain area for differentiating Parkinson's disease from progressive supranuclear palsy. Clin Neurol Neurosurg 183:105383. https://doi.org/10.1016/j.clineuro.2019.105383
Tian J, Liu H, Zhang M, et al. (2020) The value of TCS, SWI and MRI in identifying progressive supranuclear palsy and Parkinson’s disease. J Apoplexy and Nervous Diseases 37, 895-899. https://doi.org/10.19845/j.cnki.zfysjjbzz.2020.0479
Wang LS, Yu TF, Chai B et al (2021) Transcranial sonography in differential diagnosis of Parkinson disease and other movement disorders. Chin Med J (Engl) 134:1726–1731. https://doi.org/10.1097/cm9.0000000000001503
Pilotto A, Yilmaz R, Berg D (2015) Developments in the role of transcranial sonography for the differential diagnosis of parkinsonism. Curr Neurol Neurosci Rep 15:43. https://doi.org/10.1007/s11910-015-0566-9
Whitwell JL, Hoglinger GU, Antonini A et al (2017) Radiological biomarkers for diagnosis in PSP: Where are we and where do we need to be? Mov Disord 32:955–971. https://doi.org/10.1002/mds.27038
He L, Wu DF, Zhang JH et al (2022) Factors affecting transtemporal window quality in transcranial sonography. Brain Behav 12:e2543. https://doi.org/10.1002/brb3.2543
Liang P, Shi L, Chen N et al (2015) Construction of brain atlases based on a multi-center MRI dataset of 2020 Chinese adults. Sci Rep:5. https://doi.org/10.1038/srep18216
Garcia-Malo C, Novo-Ponte S, Castro-Villacanas Farzamnia A et al (2021) Correlation between systemic iron parameters and substantia nigra iron stores in restless legs syndrome. Sleep Med 85:191–195. https://doi.org/10.1016/j.sleep.2021.07.027
Lee S, Martinez-Valbuena I, de Andrea CE et al (2022) Cell-specific dysregulation of iron and oxygen homeostasis as a novel pathophysiology in PSP. Ann Neurol. https://doi.org/10.1002/ana.26540
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81501110) and Hunan Province Natural Science Foundation (2020JJ4457).
Author information
Authors and Affiliations
Contributions
Yafei Wen searched the databases, selected, and assessed the articles, extracted, and analyzed the data, and drafted the manuscript. Hui Zhou, Mengwen Xia, Qianqian Liu and Hongzhi Quan made contributions to article searching, quality assessments and data collection. Liangjuan Fang designed the study and revised the manuscript. Liangjuan Fang and Hongzhi Quan supported the study.
Corresponding author
Ethics declarations
Ethical approval and informed consent
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wen, ., Zhou, H., Xia, M. et al. Differentiating progressive supranuclear palsy from other movement disorders using transcranial sonography: a systematic review and meta-analysis. Neurol Sci 45, 455–465 (2024). https://doi.org/10.1007/s10072-023-07107-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-07107-x