Abstract
Background
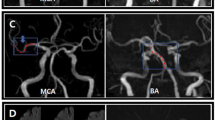
A common-stem origin of lenticulostriate arteries (CS-LSAs) is an anatomical variation that supplies a moderate to large section of the basal ganglia. We hypothesized that CS-LSAs with a patent orifice are located at distal positions of the acute-occluded middle cerebral artery (MCA) and that the blood flow of CS-LSAs is supplied by pail arterial anastomoses and results in hypoperfusion of CS-LSAs, similar to a deep watershed (DWS) infarction.
Objective
Our study evaluated the possibility of CS-LSAs in patients with DWS infarction and MCA occlusion and also assessed the safety of endovascular therapy (ET) in these patients.
Methods
A cohort of consecutive patients with DWS infarction and MCA occlusion and in whom full recanalization via ET was achieved were identified. Patients were divided into two groups based on the presence of CS-LSAs observed during ET. In addition, radiological and clinical data were retrospectively analyzed.
Results
Thirty-three patients were included, and CS-LSAs were observed in 48.5% (16/33) of patients. The possibility (72.2%, 13/18) of CS-LSAs was high in patients with DWS infarction companied with basal ganglia infarction. A good clinical outcome was similar in patients with CS-LSAs and basal ganglia infarction and in patients without CS-LSAs and basal ganglia infarction (69.2% vs. 81.8%, P = 0.649).
Conclusions
The possibility of CS-LSAs was 48.5% in patients with DWS infarction and MCA occlusion, and the revascularization procedure was safe and feasible in these patients despite the moderate-to-large basal ganglia infarction.



Similar content being viewed by others
Abbreviations
- LSAs:
-
Lenticulostriate arteries
- CS-LSAs:
-
Common-stem LSAs
- MCA:
-
Middle cerebral artery
- ICA:
-
Internal carotid artery
- ET:
-
Endovascular therapy
- DWS:
-
Deep watershed
- NIHSS:
-
National Institutes of Health Stroke Scale
- mRS:
-
Modified Rankin Scale
- FVH:
-
Fluid-attenuated inversion recovery vascular hyperintensities
- CWS:
-
Cortical watershed
- mTICI:
-
Modified Thrombolysis in Cerebral Infarction
- ACG:
-
American Society of Interventional and Therapeutic Neuroradiology collateral grading
- TOAST:
-
Trial of Org 10172 in Acute Stroke Treatment
- sICH:
-
Symptomatic intracranial hemorrhage
References
Djulejić V, Marinković S, Maliković A, Jovanović I, Djordjević D, Ćetković M, Todorović V, Milisavljević M (2012) Morphometric analysis, region of supply and microanatomy of the lenticulostriate arteries and their clinical significance. J Clin Neurosci 19:1416–1421. https://doi.org/10.1016/j.jocn.2011.10.025
Decavel P, Vuillier F, Moulin T (2012) Lenticulostriate infarction. Front Neurol Neurosci 30:115–119. https://doi.org/10.1159/000333606
Marinković S, Gibo H, Milisavljević M, Ćetković M (2001) Anatomic and clinical correlations of the lenticulostriate arteries. Clin Anat 14:190–195. https://doi.org/10.1002/ca.1032
Moustafa RR, Momjian-Mayor I, Jones PS, Morbelli S, Day DJ, Aigbirhio FI, Fryer TD, Warburton EA, Baron JC (2011) Microembolism versus hemodynamic impairment in rosary-like deep watershed infarcts: a combined positron emission tomography and transcranial doppler study. Stroke 42:3138–3143. https://doi.org/10.1161/STROKEAHA.111.616334
Alawneh JA, Moustafa RR, Baron J-C (2009) Hemodynamic factors and perfusion abnormalities in early neurological deterioration. Stroke 40:e443–e450. https://doi.org/10.1161/STROKEAHA.108.532465
Chen W-H, Yi T-Y, Wu Y-M, Zhang MF, Lin DL, Lin XH (2018) Safety of endovascular treatment in progressive ischemic stroke and anterior circulation large artery occlusion. World Neurosurg 122:e383–e389. https://doi.org/10.1016/j.wneu.2018.10.059
Wang Z, Soo YO, Mok VC (2015) Cerebral microbleeds is antithrombotic therapy safe to administer? Stroke 45:2811–2817. https://doi.org/10.1161/STROKEAHA.114.004286
Natarajan SK, Snyder KV, Siddiqui AH, Ionita CC, Hopkins LN, Levy EI (2009) Safety and effectiveness of endovascular therapy after 8 hours of acute ischemic stroke onset and wake-up strokes. Stroke 40:3269–3274. https://doi.org/10.1161/STROKEAHA.109.555102
Seok WY, Oh YB, Phil HL, Wen YL (2006) Internal and cortical border-zone infarction: clinical and diffusion-weighted imaging features. Stroke 37:841–846. https://doi.org/10.1161/01.STR.0000202590.75972.39
Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL, Marks MP, Prabhakaran S, Kallmes DF, Fitzsimmons BF, Mocco J, Wardlaw JM, Barnwell SL, Jovin TG, Linfante I, Siddiqui AH, Alexander MJ, Hirsch JA, Wintermark M, Albers G, Woo HH, Heck DV, Lev M, Aviv R, Hacke W, Warach S, Broderick J, Derdeyn CP, Furlan A, Nogueira RG, Yavagal DR, Goyal M, Demchuk AM, Bendszus M, Liebeskind DS, Cerebral Angiographic Revascularization Grading (CARG) Collaborators, STIR Revascularization working group., STIR Thrombolysis in Cerebral Infarction (TICI) Task Force (2013) Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke 44:2650–2663. https://doi.org/10.1161/STROKEAHA.113.001972
Adams H, Adams H, Bendixen B et al (1993) Classification of subtype of acute ischemic stroke. Stroke 23:35–41. https://doi.org/10.1161/01.STR.24.1.35
Campbell BCV, Mitchell PJ, Kleinig TJ et al (2015) Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 372:1009–1018. https://doi.org/10.1056/NEJMoa1414792
Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, Johnston KC, Johnston SC, Khalessi AA, Kidwell CS, Meschia JF, Ovbiagele B, Yavagal DR, American Heart Association Stroke Council (2015) 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American. Stroke 46:3020–3035. https://doi.org/10.1161/STR.0000000000000074
Nogueira RG, Jadhav AP, Haussen DC et al (2017) Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. https://doi.org/10.1056/NEJMoa1706442
Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, McTaggart R, Torbey MT, Kim-Tenser M, Leslie-Mazwi T, Sarraj A, Kasner SE, Ansari SA, Yeatts SD, Hamilton S, Mlynash M, Heit JJ, Zaharchuk G, Kim S, Carrozzella J, Palesch YY, Demchuk AM, Bammer R, Lavori PW, Broderick JP, Lansberg MG, DEFUSE 3 Investigators (2018) Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 378:708–718. https://doi.org/10.1056/NEJMoa1713973
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC, Kidwell CS, Leslie-Mazwi TM, Ovbiagele B, Scott PA, Sheth KN, Southerland AM, Summers DV, Tirschwell DL, American Heart Association Stroke Council (2018) 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 49(3):e46–e110
Derdeyn CP, Khosla A, Videen TO et al (2001) Severe hemodynamic impairment and border zone--region infarction. Radiology 220:195–201. https://doi.org/10.1148/radiology.220.1.r01jl09195
Yamauchi H, Nishii R, Higashi T, Kagawa S, Fukuyama H (2009) Hemodynamic compromise as a cause of internal border-zone infarction and cortical neuronal damage in atherosclerotic middle cerebral artery disease. Stroke 40:3730–3735. https://doi.org/10.1161/STROKEAHA.109.560011
van Heesewijk HPM, Vos JA, Louwerse ES, van den Berg JC, Overtoom TTC, Ernst SMPG, Mauser HW, Moll FL, Ackerstaff RGA (2002) New brain lesions at MR imaging after carotid angioplasty and stent placement. Radiology 224:361–365. https://doi.org/10.1148/radiol.2242011302
Bladin CF, Chambers BR (1993) Clinical features, pathogenesis, and computed tomographic characteristics of internal watershed infarction. Stroke 24:1925–1932
Kang CK, Park CW, Han JY, Kim SH, Park CA, Kim KN, Hong SM, Kim YB, Lee KH, Cho ZH (2009) Imaging and analysis of lenticulostriate arteries using 7.0-tesla magnetic resonance angiography. Magn Reson Med 61:136–144. https://doi.org/10.1002/mrm.21786
Akashi T, Miyasaka T, Takewa M et al (2012) Branching pattern of lenticulostriate arteries observed by MR angiography at 3.0 T. Jpn J Radiol 30:331–335. https://doi.org/10.1007/s11604-012-0058-7
Acknowledgments
We thank teams from American Journal Expert (https://secure.aje.com/cn/researcher/), for editing the English text of a draft of this manuscript.
Funding
This research received grant from Joint Funds for the innovation of science and Technology, Fujian province (Grant number: 2018J01207).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Implication of patient care
1. There is a moderate chance of common-stem LSAs (CS-LSAs) in progressive ischemic stroke patients with deep watershed (DWS) infarction and middle cerebral artery (MCA) occlusion.
2. The mechanism of basal ganglia infarction was hypoperfusion in these types of patients.
3. The recanalization procedure was feasible in these patients.
Rights and permissions
About this article
Cite this article
Chen, W.h., Yi, Ty., Zhan, Al. et al. Clinical significance of common-stem lenticulostriate arteries in patients with internal watershed infarction. Neurol Sci 40, 2303–2309 (2019). https://doi.org/10.1007/s10072-019-03953-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-019-03953-w