Abstract
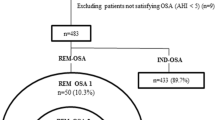
Previous studies aimed to determine if Pittsburgh sleep quality index (PSQI) is a valid screening instrument for obstructive sleep apnea, indicating its disadvantages. However, the rationale of PSQI use in sleep clinics is not the screening, but the assessment of sleep quality itself. Therefore, the aims of this study were to investigate the sleep quality in obstructive sleep apnea patients and to identify the cutoff point for differentiation of “good” and “poor” sleepers among them. We constructed the Croatian version of PSQI and assessed its psychometric properties. The protocol of the study included the assessment of sleep quality in 130 obstructive sleep apnea patients and 75 healthy control subjects. All subjects completed the Croatian version of the PSQI, and the patients underwent overnight polysomnography screening. Obstructive sleep apnea patients had higher values of the global PSQI component score, indicating lower sleep quality, compared to a healthy control group (p < 0.001). The psychometric properties of PSQI scores in the prediction of normal sleep efficiency indicate that the cutoff score of 9.5 differentiates patients in total sleep time (p < 0.001), REM duration (p = 0.014), sleep efficiency (p = 0.001), time spent awake during sleep (p = 0.006), after sleep (p = 0.024), and after sleep onset (p = 0.001). In OSA patients, a PSQI cutoff score of 9.5 differentiated good and poor sleepers significantly in total sleep time, REM duration, time spent awake during sleep, and WASO time. Current findings enhance the interpretability of PSQI results in a population of OSA patients.

Similar content being viewed by others
References
Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, Colantonio A (2016) The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis. Sleep Med Rev 25:52–73
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Beaudreau SA, Spira AP, Stewart A, Kezirian EJ, Lui LY, Ensrud K et al (2012) Validation of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older black and white women. Sleep Med 13(1):36–42
Brekke FB, Amro A, Hortemo Osthus TB, Dammen T, Waldum B, Os I (2013) Sleep complaints, depression and quality of life in Norwegian dialysis patients. Clin Clin Nephrol 80(2):88–97
Buysse DJ, Hall ML, Strollo PJ, Kamarck TW, Owens J, Lee L et al (2008) Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med 4(6):563–571
Grandner MA, Kripke DF, Yoon IY, Youngstedt SD (2006) Criterion validity of the Pittsburgh Sleep Quality Index: investigation in a non-clinical sample. Sleep Biol Rhythms 4(2):129–133
Kotronoulas GC, Papadopoulou CN, Papapetrou A, Patiraki E (2011) Psychometric evaluation and feasibility of the Greek Pittsburgh Sleep Quality Index (GR-PSQI) in patients with cancer receiving chemotherapy. Support Care Cancer 19(11):1831–1840
Mondal P, Gjevre JA, Taylor-Gjevre RM, Lim HJ Relationship between the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in a sleep laboratory referral population. Nat Sci Sleep 5:15–21
Nishiyama T, Mizuno T, Kojima M, Suzuki S, Kitajima T, Ando KB et al (2013) Criterion validity of the Pittsburgh Sleep Quality Index and Epworth Sleepiness Scale for the diagnosis of sleep disorders. Sleep Med 15(4):422–429
Spira AP, Beaudreau SA, Stone KL, Kezirian EJ, Lui LY, Redline S et al (2012) Reliability and validity of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older men. J Gerontol Ser A-Biol Sci Med Sci 67(4):433–439
Scarlata S, Pedone C, Curcio G, Cortese L, Chiurco D, Fontana D et al (2013) Pre-polysomnographic assessment using the Pittsburgh Sleep Quality Index questionnaire is not useful in identifying people at higher risk for obstructive sleep apnea. J Med Screen 20(4):220–226
Shochat T, Tzischinsky O, Oksenberg A, Peled R (2007) Validation of the Pittsburgh Sleep Quality Index Hebrew translation (PSQI-H) in a sleep clinic sample. Isr Med Assoc J 9(12):853–856
Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F (2002) Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res 53(3):737–740
Curcio G, Tempesta D, Scarlata S, Marzano C, Moroni F, Rossini PM et al (2013) Validity of the Italian version of the Pittsburgh Sleep Quality Index (PSQI). Neurol Sci 34(4):511–519
Farrahi Moghaddam J, Nakhaee N, Sheibani V, Garrusi B, Amirkafi A (2012) Reliability and validity of the Persian version of the Pittsburgh Sleep Quality Index (PSQI-P). Sleep Breath 16(1):79–82
Sohn SI, Kim do H, Lee MY, Cho YW (2012) The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath 16(3):803–812
Tsai PS, Wang MY, Wang SY et al (2005) Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual Life Res 14:1943–1952
Bertolazi AN, Fagondes SC, Hoff LS, Dartora EG, Miozzo IC, de Barba ME et al (2011) Validation of the Brazilian Portuguese version of the Pittsburgh Sleep Quality Index. Sleep Med 12(1):70–75
Jordan AS, McSharry DG, Malhotra A (2014) Adult obstructive sleep apnoea. Lancet 383(9918):736–747
Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S et al (2008) STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 108(5):812–821
Collop NA, Anderson WM, Boehlecke B, Claman D, Goldberg R, Gottlieb DJ et al (2007) Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 3(7):737–747
Santos-Silva R, Sartori DE, Truksinas V, Truksinas E, Alonso FF, Tufik S et al (2009) Validation of a portable monitoring system for the diagnosis of obstructive sleep apnea syndrome. Sleep 32(5):629–636
Thurnheer R (2006) Diagnosis of obstructive sleep apnea: alternatives to polysomnography. Chest 130(5):1625
Bianchi MT, Williams KL, McKinney S, Ellenbogen JM (2013) The subjective-objective mismatch in sleep perception among those with insomnia and sleep apnea. J Sleep Res 22(5):557–568
American Academy of Sleep Medicine (2014) International classification of sleep disorders, 3rd edn. American Academy of Sleep Medicine, Darien
Rudan I, Marušić A, Janković S, Rotim K, Boban M, Lauc G et al (2009) “10 001 Dalmatians:” Croatia launches its National Biobank. Cro Med J 50(1):4–6
Hirshkowitz M (2004) Normal human sleep: an overview. Med Clin North Am 88(3):551–565
Fischer J, Dogas Z, Bassetti CL, Berg S, Grote L, Jennum P et al (2012) Standard procedures for adults in accredited sleep medicine centres in Europe. J Sleep Res 21(4):357–368
Devine EB, Hakim Z, Green J (2005) A systematic review of patient-reported outcome instruments measuring sleep dysfunction in adults. PharmacoEconomics 23(9):889–912
Castronovo V, Galbiati A, Marelli S, Brombin C, Cugnata F, Giarolli L et al (2016) Validation study of the Italian version of the Insomnia Severity Index (ISI). Neurol Sci 37(9):1517–1524
Lucchesi C, Baldacci F, Cafalli M et al (2016) Fatigue, sleep–wake pattern, depressive and anxiety symptoms and body-mass index: analysis in a sample of episodic and chronic migraine patients. Neurol Sci 37:987
Knutson KL, Rathouz PJ, Yan LL, Liu K, Lauderdale DS (2006) Stability of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Questionnaires over 1 year in early middle-aged adults: the CARDIA study. Sleep 29(11):1503–1506
Macey PM, Woo MA, Kumar R, Cross RL, Harper RM (2010) Relationship between obstructive sleep apnea severity and sleep, depression and anxiety symptoms in newly-diagnosed patients. PLoS One 5(4):10211
El Shayeb M, Topfer LA, Stafinski T, Pawluk L, Menon D (2014) Diagnostic accuracy of level 3 portable sleep tests versus level 1 polysomnography for sleep-disordered breathing: a systematic review and meta-analysis. Can Med Assoc J 186(1):25–51
Acknowledgments
The authors wish to thank Mrs. Jelena Baricevic from the Department of Neuroscience, University of Split School of Medicine for her technical assistance, and Natalija Ivković, MS, from the Split Sleep Medicine Center, University of Split School of Medicine and University Hospital Split for her technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The protocol of the study was approved by the Biomedical Ethics Committee of the University of Split School of Medicine, Split, Croatia. Informed consent was obtained from all individual participants included in the study.
Funding
This study was funded by the Croatian Science Foundation grant #IP-11-2013-5935.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Lusic Kalcina, L., Valic, M., Pecotic, R. et al. Good and poor sleepers among OSA patients: sleep quality and overnight polysomnography findings. Neurol Sci 38, 1299–1306 (2017). https://doi.org/10.1007/s10072-017-2978-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-017-2978-6