Abstract
Purpose
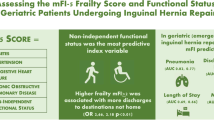
Frailty has shown promise in predicting postoperative morbidity and mortality following hernia surgery. This study aims to evaluate the predictive capacity of the 11-item modified frailty index (mFI) in estimating postoperative outcomes following elective hernia surgery using the National Inpatient Sample (NIS) database.
Methods
A retrospective analysis of the NIS from 2015 to 2019 was performed including adult patients who underwent elective hernia repair. The mFI was used to stratify patients as either frail (mFI ≥ 0.27) or robust (mFI < 0.27). The primary outcomes were in-hospital postoperative morbidity and mortality. The secondary outcomes were system-specific morbidity, length of stay (LOS), total in-hospital healthcare cost, and discharge disposition. Univariable and multivariable regressions were utilized.
Results
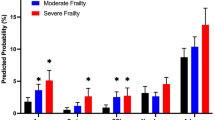
In total, 14,125 robust patients and 1704 frail patients were included. Frailty was associated with an increased age (mean age 66.4 years vs. 52.6 years, p < 0.001) and prevalence of ventral hernias (51.9% vs. 44.4%, p < 0.001). Adjusted analyses demonstrated that frail patients had increased in-hospital mortality (adjusted odds ratio (aOR) 3.89, 95% CI 1.50, 10.11, p = 0.005), postoperative overall morbidity (aOR 1.98, 95% CI 1.72, 2.29, p < 0.001), postoperative LOS (adjusted mean difference (aMD) 0.78 days, 95% CI 0.51, 1.06, p < 0.001), total in-hospital healthcare costs (aMD $7562 95% CI 3292, 11,832, p = 0.001), and were less likely to be discharged home (aOR 0.61, 95% CI 0.53, 0.69, p < 0.001).
Conclusion
The mFI may be a reliable predictor of postoperative morbidity and mortality in elective hernia surgery. Utilizing this tool can aid in patient education and identifying high-risk patients who may benefit from tailored prehabilitation.
Similar content being viewed by others
Data and code availability
All data generated or analyzed during this study are included in this published article and its supplementary information files. Files can be provided by the corresponding author upon request.
References
Rutkow IM, Robbins AW (1993) Demographic, classificatory, and socioeconomic aspects of hernia repair in the United States. Surg Clin North Am 73(3):413–426. https://doi.org/10.1016/s0039-6109(16)46027-5
Howard R, Thompson M, Fan Z, Englesbe M, Dimick JB, Telem DA (2019) Costs associated with modifiable risk factors in ventral and incisional hernia repair. JAMA Netw Open 2(11):e1916330. https://doi.org/10.1001/jamanetworkopen.2019.16330
Moran J, Guinan E, McCormick P, Larkin J, Mockler D, Hussey J, Moriarty J, Wilson F (2016) The ability of prehabilitation to influence postoperative outcome after intra-abdominal operation: a systematic review and meta-analysis. Surgery 160(5):1189–1201. https://doi.org/10.1016/j.surg.2016.05.014
Jensen KK, East B, Jisova B, Cano ML, Cavallaro G, Jørgensen LN, Rodrigues V, Stabilini C, Wouters D, Berrevoet F (2022) The European hernia society prehabilitation project: a systematic review of patient prehabilitation prior to ventral hernia surgery. Hernia 26(3):715–726. https://doi.org/10.1007/s10029-022-02573-2
Lindmark M, Strigård K, Löwenmark T, Dahlstrand U, Gunnarsson U (2018) Risk factors for surgical complications in ventral hernia repair. World J Surg 42(11):3528–3536. https://doi.org/10.1007/s00268-018-4642-6
Goodenough CJ, Ko TC, Kao LS, Nguyen MT, Holihan JL, Alawadi Z, Nguyen DH, Flores JR, Arita NT, Roth JS, Liang MK (2015) Development and validation of a risk stratification score for ventral incisional hernia after abdominal surgery: hernia expectation rates in intra-abdominal surgery (the HERNIA Project). J Am Coll Surg 220(4):405–413. https://doi.org/10.1016/j.jamcollsurg.2014.12.027
Howard R, Delaney L, Kilbourne AM, Kidwell KM, Smith S, Englesbe M, Dimick J, Telem D (2021) Development and implementation of preoperative optimization for high-risk patients with abdominal wall hernia. JAMA Netw Open 4(5):e216836. https://doi.org/10.1001/jamanetworkopen.2021.6836
Delaney LD, Howard R, Palazzolo K, Ehlers AP, Smith S, Englesbe M, Dimick JB, Telem DA (2021) Outcomes of a presurgical optimization program for elective hernia repairs among high-risk patients. JAMA Netw Open 4(11):e2130016. https://doi.org/10.1001/jamanetworkopen.2021.30016
Cox TC, Blair LJ, Huntington CR, Colavita PD, Prasad T, Lincourt AE, Heniford BT, Augenstein VA (2016) The cost of preventable comorbidities on wound complications in open ventral hernia repair. J Surg Res 206(1):214–222. https://doi.org/10.1016/j.jss.2016.08.009
Grove TN, Kontovounisios C, Montgomery A, Heniford BT, Windsor ACJ, Warren OJ, Europe Collaborative AWR (2021) Perioperative optimization in complex abdominal wall hernias: Delphi consensus statement. BJS Open 5(5):zrab082. https://doi.org/10.1093/bjsopen/zrab082
Basta MN, Fischer JP, Wink JD, Kovach SJ (2016) Mortality after inpatient open ventral hernia repair: developing a risk stratification tool based on 55,760 operations. Am J Surg 211(6):1047–1057. https://doi.org/10.1016/j.amjsurg.2015.03.009
Berger RL, Li LT, Hicks SC, Davila JA, Kao LS, Liang MK (2013) Development and validation of a risk-stratification score for surgical site occurrence and surgical site infection after open ventral hernia repair. J Am Coll Surg 217(6):974–982. https://doi.org/10.1016/j.jamcollsurg.2013.08.003
Pannucci CJ, Basta MN, Fischer JF, Kovach SJ (2015) Creation and validation of a condition-specific venous thromboembolism risk assessment tool for open ventral hernia repair patients. J Vasc Surg Venous Lymphat Disord 3(1):127–128. https://doi.org/10.1016/j.jvsv.2014.10.031
Fischer JP, Wink JD, Tuggle CT, Nelson JA, Kovach SJ (2015) Wound risk assessment in ventral hernia repair: generation and internal validation of a risk stratification system using the ACS-NSQIP. Hernia 19(1):103–111. https://doi.org/10.1007/s10029-014-1318-5
Fligor JE, Lanier ST, Dumanian GA (2017) Current risk stratification systems are not generalizable across surgical technique in midline ventral hernia repair. Plast Reconstr Surg Glob Open 5(3):e1206. https://doi.org/10.1097/GOX.0000000000001206
Xue QL (2011) The frailty syndrome: definition and natural history. Clin Geriatr Med 27(1):1–15. https://doi.org/10.1016/j.cger.2010.08.009
Joseph WJ, Cuccolo NG, Baron ME, Chow I, Beers EH (2020) Frailty predicts morbidity, complications, and mortality in patients undergoing complex abdominal wall reconstruction. Hernia 24(2):235–243. https://doi.org/10.1007/s10029-019-02047-y
Solano QP, Howard R, Mullens CL, Ehlers AP, Delaney LD, Fry B, Shen M, Englesbe M, Dimick J, Telem D (2023) The impact of frailty on ventral hernia repair outcomes in a statewide database. Surg Endosc 37(7):5603–5611. https://doi.org/10.1007/s00464-022-09626-8
Perez AJ, Campbell S (2022) Inguinal hernia repair in older persons. J Am Med Dir Assoc 23(4):563–567. https://doi.org/10.1016/j.jamda.2022.02.008
Balla FM, Yheulon CG, Stetler JL, Patel AD, Lin E, Davis SS (2019) Ventral hernia repair outcomes predicted by a 5-item modified frailty index using NSQIP variables. Hernia 23(5):891–898. https://doi.org/10.1007/s10029-019-01923-x
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A (2005) A global clinical measure of fitness and frailty in elderly people. CMAJ 173(5):489–495. https://doi.org/10.1503/cmaj.050051
Velanovich V, Antoine H, Swartz A, Peters D, Rubinfeld I (2013) Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. J Surg Res 183(1):104–110. https://doi.org/10.1016/j.jss.2013.01.021
Li JL, Henderson MA, Revenig LM, Sweeney JF, Kooby DA, Maithel SK, Master VA, Ogan K (2016) Frailty and one-year mortality in major intra-abdominal operations. J Surg Res 203(2):507-512.e1. https://doi.org/10.1016/j.jss.2016.03.007
Alluri RK, Leland H, Heckmann N (2016) Surgical research using national databases. Ann Transl Med 4(20):393. https://doi.org/10.21037/atm.2016.10.49
Hoffman RD, Danos DM, Lau FH (2021) National health disparities in incisional hernia repair outcomes: an analysis of the healthcare cost and utilization project national inpatient sample (HCUP-NIS) 2012–2014. Surgery 169(6):1393–1399. https://doi.org/10.1016/j.surg.2020.11.028
Schlosser KA, Renshaw SM, Tamer RM, Strassels SA, Poulose BK (2023) Ventral hernia repair: an increasing burden affecting abdominal core health. Hernia 27(2):415–421. https://doi.org/10.1007/s10029-022-02707-6
Colavita PD, Tsirline VB, Walters AL, Lincourt AE, Belyansky I, Heniford BT (2013) Laparoscopic versus open hernia repair: outcomes and sociodemographic utilization results from the nationwide inpatient sample. Surg Endosc 27(1):109–117. https://doi.org/10.1007/s00464-012-2432-z
Wahl TS, Graham LA, Hawn MT, Richman J, Hollis RH, Jones CE, Copeland LA, Burns EA, Itani KM, Morris MS (2017) Association of the modified frailty index with 30-day surgical readmission. JAMA Surg 152(8):749–757. https://doi.org/10.1001/jamasurg.2017.1025
Quan H, Drösler S, Sundararajan V, Wen E, Burnand B, Couris CM, Halfon P, Januel JM, Kelley E, Klazinga N, Luthi JC, Moskal L, Pradat E, Romano PS, Shepheard J, So L, Sundaresan L, Tournay-Lewis L, Trombert-Paviot B, Webster G, Ghali WA (2008) Adaptation of AHRQ patient safety indicators for use in ICD-10 administrative data by an international consortium. In: Henriksen K, Battles JB, Keyes MA, Grady ML (eds) Advances in patient safety: new directions and alternative approaches (Vol. 1: Assessment). Agency for Healthcare Research and Quality, Rockville
Storesund A, Haugen AS, Hjortås M, Nortvedt MW, Flaatten H, Eide GE, Boermeester MA, Sevdalis N, Søfteland E (2019) Accuracy of surgical complication rate estimation using ICD-10 codes. Br J Surg 106(3):236–244. https://doi.org/10.1002/bjs.10985
LaPar DJ, Bhamidipati CM, Mery CM, Stukenborg GJ, Jones DR, Schirmer BD, Kron IL, Ailawadi G (2010) Primary payer status affects mortality for major surgical operations. Ann Surg 252(3):544–550. https://doi.org/10.1097/SLA.0b013e3181e8fd75
Kokotovic D, Bisgaard T, Helgstrand F (2016) Long-term recurrence and complications associated with elective incisional hernia repair. JAMA 316(15):1575–1582. https://doi.org/10.1001/jama.2016.15217
Lu Y, Chen DC, MacQueen IT (2021) General surgery: management of postoperative complications following ventral hernia repair and inguinal hernia repair. Surg Clin North Am 101(5):755–766. https://doi.org/10.1016/j.suc.2021.05.018
Luijendijk RW, Hop WC, van den Tol MP, de Lange DC, Braaksma MM, IJzermans JN, Boelhouwer RU, de Vries BC, Salu MK, Wereldsma JC, Bruijninckx CM, Jeekel J (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 343(6):392–398. https://doi.org/10.1056/NEJM200008103430603
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240(4):578–583. https://doi.org/10.1097/01.sla.0000141193.08524.e7
Petro CC, Prabhu AS (2018) Preoperative planning and patient optimization. Surg Clin North Am 98(3):483–497. https://doi.org/10.1016/j.suc.2018.01.005
de Jong DLC, Wegdam JA, Berkvens EBM, Nienhuijs SW, de Vries Reilingh TS (2023) The influence of a multidisciplinary team meeting and prehabilitation on complex abdominal wall hernia repair outcomes. Hernia 27(3):609–616. https://doi.org/10.1007/s10029-023-02755-6
Liang MK, Bernardi K, Holihan JL, Cherla DV, Escamilla R, Lew DF, Berger DH, Ko TC, Kao LS (2018) Modifying risks in ventral hernia patients with prehabilitation: a randomized controlled trial. Ann Surg 268(4):674–680. https://doi.org/10.1097/SLA.0000000000002961
Augenstein VA, Colavita PD, Wormer BA, Walters AL, Bradley JF, Lincourt AE, Horton J, Heniford TB (2015) CeDAR: Carolinas equation for determining associated risks. J Am Coll Surg 221(4):S65–S66. https://doi.org/10.1016/j.jamcollsurg.2015.07.145
Ventral Hernia Working Group, Breuing K, Butler CE, Ferzoco S, Franz M, Hultman CS, Kilbridge JF, Rosen M, Silverman RP, Vargo D (2010) Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery 148(3):544–558. https://doi.org/10.1016/j.surg.2010.01.008
Basta MN, Kozak GM, Broach RB, Messa CA 4th, Rhemtulla I, DeMatteo RP, Serletti JM, Fischer JP (2019) Can we predict incisional hernia?: development of a surgery-specific decision-support interface. Ann Surg 270(3):544–553. https://doi.org/10.1097/SLA.0000000000003472
Pulik Ł, Jaśkiewicz K, Sarzyńska S, Małdyk P, Łęgosz P (2020) Modified frailty index as a predictor of the long-term functional result in patients undergoing primary total hip arthroplasty. Reumatologia 58(4):213–220. https://doi.org/10.5114/reum.2020.98433
Funding
This research was conducted without external or internal sources of funding. No funding or source of support was received for this work.
Author information
Authors and Affiliations
Contributions
Conception and design of the study: All authors. Acquisition of data: TM; Analysis and interpretation of data: TM, JK; Drafting and revision of the manuscript: All authors; Approval of the final version of the manuscript: All authors; Agreement to be accountable for all aspects of the work: All authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial or non-financial competing interests to declare. Mr. Khamar, Dr. McKechnie, Mr. Hatamnejad, Dr. Lee, Dr. Huo, Dr. Passos, Dr. Sne, Dr. Eskicioglu, and Dr. Hong declare that they have no conflicts of interest.
Ethical approval
This is an observational study and ethics approval was not required as patient identifiers were not obtained from the NIS. Confirmed by the Hamilton Integrated Research Ethics Board.
Human and animal rights
This research was based on data derived from medical records and thus included human participants. As such, it complied to all ethical standards.
Informed consent
The data used in this study was taken from the National Inpatient Sample database. As this repository only supplies deindentified data, informed consent could not be obtained.
Consent to participate/consent to publish
Not applicable as the NIS utilizes anonymous, cumulative data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khamar, J., McKechnie, T., Hatamnejad, A. et al. The modified frailty index predicts postoperative morbidity in elective hernia repair patients: analysis of the national inpatient sample 2015–2019. Hernia 28, 517–526 (2024). https://doi.org/10.1007/s10029-023-02944-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-023-02944-3