Abstract
Background
Mesh repair in incarcerated or strangulated groin hernia is controversial, especially when bowel resection is required. We aimed to perform a meta-analysis comparing mesh and non-mesh repair in patients undergoing emergency groin hernia repair.
Methods
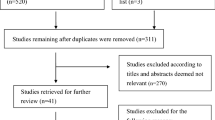
We performed a literature search of databases to identify studies comparing mesh and primary suture repair of patients with incarcerated or strangulated inguinal or femoral hernias who underwent emergency surgery. Postoperative outcomes were assessed by pooled analysis and meta-analysis. Statistical analysis was performed using RevMan 5.4. Heterogeneity was assessed with I2 statistics.
Results
1095 studies were screened and 101 were thoroughly reviewed. Twenty observational studies and four randomized controlled trials comprising 12,402 patients were included. We found that mesh-based repair had reduced recurrence (OR 0.36; 95% CI 0.19, 0.67; P = 0.001; I2 = 35%), length of hospital stay (OR − 1.02; 95% CI − 1.87, − 0.17; P = 0.02; I2 = 94%) and operative time (OR − 9.21; 95% CI − 16.82, − 1.61; P = 0.02; I2 = 95%) without increasing surgical site infection, mortality or postoperative complications such as seroma, chronic, ileus or urinary retention. In the subgroup analysis of patients that underwent bowel resection, we found that mesh repair was associated with an increased risk of surgical site infection (OR 1.74; 95% CI 1.04, 2.91; P = 0.04; I2 = 9%).
Conclusions
Mesh repair for incarcerated and strangulated groin hernias reduces recurrence without an increase in postoperative complications and should be considered in clean cases. However, in the setting of bowel resection, mesh repair might increase the incidence of surgical site infection.








Similar content being viewed by others
References
Kumar D, Wu D, Tan B et al (2022) Emergency groin hernia: outcome after mesh and non‐mesh repair. ANZ J Surg ans.18212. https://doi.org/10.1111/ans.18212
The HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165. https://doi.org/10.1007/s10029-017-1668-x
Samuel JC, Tyson AF, Mabedi C et al (2014) Development of a ratio of emergent to total hernia repairs as a surgical capacity metric. Int J Surg 12:906–911. https://doi.org/10.1016/j.ijsu.2014.07.019
Alvarez JA, Baldonedo RF, Bear IG et al (2004) Incarcerated groin hernias in adults: presentation and outcome. Hernia 8:121–126. https://doi.org/10.1007/s10029-003-0186-1
Simon KL, Frelich MJ, Gould JC et al (2015) Inpatient outcomes after elective versus nonelective ventral hernia repair. J Surg Res 198:305–310. https://doi.org/10.1016/j.jss.2015.03.073
Köckerling F, Simons MP (2018) Current concepts of inguinal hernia repair. Visc Med 34:145–150. https://doi.org/10.1159/000487278
Venara A, Hubner M, Le Naoures P et al (2014) Surgery for incarcerated hernia: short-term outcome with or without mesh. Langenbecks Arch Surg 399:571–577. https://doi.org/10.1007/s00423-014-1202-x
Elsebae MMA, Nasr M, Said M (2008) Tension-free repair versus Bassini technique for strangulated inguinal hernia: a controlled randomized study. Int J Surg Lond Engl 6:302–305. https://doi.org/10.1016/j.ijsu.2008.04.006
Hentati H, Dougaz W, Dziri C (2014) Mesh repair versus non-mesh repair for strangulated inguinal hernia: systematic review with meta-analysis. World J Surg 38:2784–2790. https://doi.org/10.1007/s00268-014-2710-0
Sæter AH, Fonnes S, Rosenberg J, Andresen K (2022) High complication and mortality rates after emergency groin hernia repair: a nationwide register-based cohort study. Hernia J Hernias Abdom Wall Surg 26:1131–1141. https://doi.org/10.1007/s10029-022-02597-8
Sakamoto T, Fujiogi M, Ishimaru M et al (2022) Comparison of postoperative infection after emergency inguinal hernia surgery with enterectomy between mesh repair and non-mesh repair: a national database analysis. Hernia J Hernias Abdom Wall Surg 26:217–223. https://doi.org/10.1007/s10029-021-02439-z
Duan S-J, Qiu S-B, Ding N-Y et al (2018) Prosthetic mesh repair in the emergency management of acutely strangulated groin hernias with grade I bowel necrosis: a rational choice. Am Surg 84:215–219
Karaca A, Karaca S, Capar M et al (2016) Is graft use safe in emergency inguinal hernia repair? J Clin Anal Med 7:236–239. https://doi.org/10.4328/JCAM.3862
Panda N, Ghoshal D, Das S, Das R (2012) Lichtenstein’s mesh versus Bassini tissue repair technique for obstructed inguinal hernia: a controlled randomized study. Eur Surg Acta Chir Austriaca 44:314–318. https://doi.org/10.1007/s10353-012-0151-2
Sterne JA, Hernán MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. https://doi.org/10.1136/bmj.i4919
Sterne JAC, Savović J, Page MJ et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. https://doi.org/10.1136/bmj.l4898
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. https://doi.org/10.1136/bmj.n71
Dai W, Chen Z, Zuo J et al (2019) Risk factors of postoperative complications after emergency repair of incarcerated groin hernia for adult patients: a retrospective cohort study. Hernia J Hernias Abdom Wall Surg 23:267–276. https://doi.org/10.1007/s10029-018-1854-5
Tastaldi L, Krpata DM, Prabhu AS et al (2019) Emergent groin hernia repair: a single center 10-year experience. Surgery 165:398–405. https://doi.org/10.1016/j.surg.2018.08.001
Liu J, Chen J, Shen Y (2020) The results of open preperitoneal prosthetic mesh repair for acutely incarcerated or strangulated inguinal hernia: a retrospective study of 146 cases. Surg Endosc 34:47–52. https://doi.org/10.1007/s00464-019-06729-7
Chen F, Liu M, Jin C et al (2020) Tension-free mesh repair for incarcerated groin hernia: a comparative study. Surg Innov 27:352–357. https://doi.org/10.1177/1553350620901392
Tomaoglu K, Okmen H (2021) Prosthetic mesh hernioplasty versus primary repair in incarcerated and strangulated groin and abdominal wall hernias with or without organ resection. Retrospective study. Langenbecks Arch Surg 406:1651–1657. https://doi.org/10.1007/s00423-021-02145-5
Gopal SV, Warrier A (2013) Recurrence after groin hernia repair-revisited. Int J Surg 11:374–377. https://doi.org/10.1016/j.ijsu.2013.03.012
Karakose O, Eken H (2016) Shouldice herniorrhaphy—still an effective technique: a retrospective cohort study. Int J Surg Open 3:11–13. https://doi.org/10.1016/j.ijso.2016.04.006
Amato B, Moja L, Panico S et al (2012) Shouldice technique versus other open techniques for inguinal hernia repair. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD001543.pub4
Wysocki A, Kulawik J, Poźniczek M, Strzałka M (2006) Is the Lichtenstein operation of strangulated groin hernia a safe procedure? World J Surg 30:2065–2070. https://doi.org/10.1007/s00268-005-0416-z
Köckerling F, Heine T, Adolf D et al (2021) Trends in emergent groin hernia repair—an analysis from the herniamed registry. Front Surg 8:655755. https://doi.org/10.3389/fsurg.2021.655755
Kohga A, Kawabe A, Yajima K et al (2020) Emergency surgery versus elective surgery after reduction for patients with incarcerated groin hernias. ANZ J Surg 90:1086–1091. https://doi.org/10.1111/ans.15877
Payiziwula J, Zhao P-J, Aierken A et al (2019) Laparoscopy versus open incarcerated inguinal hernia repair in octogenarians: single-center experience with world review. Surg Laparosc Endosc Percutan Tech 29:138–140. https://doi.org/10.1097/SLE.0000000000000629
Rodrigues-Gonçalves V, Verdaguer M, Bravo-Salva A et al (2022) Open preperitoneal vs. open anterior repair for the treatment of emergency femoral hernia: a bicentric retrospective study. Hernia J Hernias Abdom Wall Surg. https://doi.org/10.1007/s10029-022-02673-z
Tatar C, Tüzün İS, Karşıdağ T et al (2016) Prosthetic mesh repair for incarcerated inguinal hernia. Balk Med J 33:434–440. https://doi.org/10.5152/balkanmedj.2016.150137
Collins MM, Race B, Messer RJ et al (2023) Practical mouse model to investigate therapeutics for Staphylococcus aureus contaminated surgical mesh implants. J Surg Res 283:428–437. https://doi.org/10.1016/j.jss.2022.10.093
Ueda J, Nomura T, Sasaki J et al (2012) Prosthetic repair of an incarcerated groin hernia with small intestinal resection. Surg Today 42:359–362. https://doi.org/10.1007/s00595-011-0019-2
Wysocki A, Strzałka M, Migaczewski M, Budzyński P (2014) Short- and long-term outcomes of incarcerated inguinal hernias repaired by Lichtenstein technique. Videosurg Miniinvas Tech 2:196–200. https://doi.org/10.5114/wiitm.2014.41630
Derici H, Unalp HR, Nazli O et al (2010) Prosthetic repair of incarcerated inguinal hernias: is it a reliable method? Langenbecks Arch Surg 395:575–579. https://doi.org/10.1007/s00423-008-0326-2
Li J, Qin C, Hu Y (2022) Comparison of mesh repair and suture repair for the treatment of incarcerated femoral hernia: a retrospective, single-center study. Surg Endosc. https://doi.org/10.1007/s00464-022-09488-0
Sharma G, Schouten JA, Itani KMF (2017) Repair of a bowel-containing, scrotal hernia with incarceration contributed by femorofemoral bypass graft. J Surg Case Rep 2017:rjw228. https://doi.org/10.1093/jscr/rjw228
Kurt N, Oncel M, Ozkan Z, Bingul S (2003) Risk and outcome of bowel resection in patients with incarcerated groin hernias: retrospective study. World J Surg 27:741–743. https://doi.org/10.1007/s00268-003-6826-x
Atila K, Guler S, Inal A et al (2010) Prosthetic repair of acutely incarcerated groin hernias: a prospective clinical observational cohort study. Langenbecks Arch Surg 395:563–568. https://doi.org/10.1007/s00423-008-0414-3
Oida T, Kawasaki A, Mimatsu K et al (2012) Mesh vs. non-mesh repair for inguinal hernias in emergency operations. Hepatogastroenterology 59:2112–2114
Sawayama H, Kanemitsu K, Okuma T et al (2014) Safety of polypropylene mesh for incarcerated groin and obturator hernias: a retrospective study of 110 patients. Hernia J Hernias Abdom Wall Surg 18:399–406. https://doi.org/10.1007/s10029-013-1058-y
Priego P, Lobo E, Moreno I et al (2005) Acute appendicitis in an incarcerated crural hernia: analysis of our experience. Rev Espanola Enfermedades Dig Organo Of Soc Espanola Patol Dig 97:707–715. https://doi.org/10.4321/s1130-01082005001000004
Wilson RB, Farooque Y (2022) Risks and prevention of surgical site infection after hernia mesh repair and the predictive utility of ACS-NSQIP. J Gastrointest Surg 26:950–964. https://doi.org/10.1007/s11605-022-05248-6
Montgomery A, Kallinowski F, Köckerling F (2016) Evidence for replacement of an infected synthetic by a biological mesh in abdominal wall hernia repair. Front Surg. https://doi.org/10.3389/fsurg.2015.00067
Bueno Lledó J, Sosa Quesada Y, Gavara GI et al (2009) Infección de la prótesis en la reparación herniaria. Nuestra experiencia en 5 años. Cir Esp 85:158–164. https://doi.org/10.1016/j.ciresp.2008.09.008
Tolino MJ, Tripoloni DE, Ratto R, García MI (2009) Infections associated with prosthetic repairs of abdominal wall hernias: pathology, management and results. Hernia 13:631–637. https://doi.org/10.1007/s10029-009-0541-y
Birolini C, de Miranda JS, Utiyama EM, Rasslan S (2015) A retrospective review and observations over a 16-year clinical experience on the surgical treatment of chronic mesh infection. What about replacing a synthetic mesh on the infected surgical field? Hernia 19:239–246. https://doi.org/10.1007/s10029-014-1225-9
Sartori A, Balla A, Botteri E et al (2022) Laparoscopic approach in emergency for the treatment of acute incarcerated groin hernia: a systematic review and meta-analysis. Hernia. https://doi.org/10.1007/s10029-022-02631-9
Kamtoh G, Pach R, Kibil W et al (2014) Effectiveness of mesh hernioplasty in incarcerated inguinal hernias. Wideochirurgia Inne Tech Maloinwazyjne Videosurgery Miniinvasive Tech 9:415–419. https://doi.org/10.5114/wiitm.2014.43080
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Patrícia Marcolin, Dr. Sergio Mazzola Poli de Figueiredo, Dr. Sérgio Walmir de Araújo, Marcella Mota Constante, Vítor Moura Fé de Melo, Dr. Rui-Min Diana Mao and Dr. Villasante-Tezanos declare that they have no conflict of interest. Dr. Richard Lu received payment/honoraria for lectures and presentations from Intuitive Surgical that are unrelated to this work.
Ethical approval
For this type of study ethical approval is not required.
Human and animal rights
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marcolin, P., Mazzola Poli de Figueiredo, S., Moura Fé de Melo, V. et al. Mesh repair versus non-mesh repair for incarcerated and strangulated groin hernia: an updated systematic review and meta-analysis. Hernia 27, 1397–1413 (2023). https://doi.org/10.1007/s10029-023-02874-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-023-02874-0