Abstract
Purpose
An aging population has led to an increased number of patients with cardiovascular comorbidities requiring antithrombotic therapy. Perioperatively, surgeons should consider the increased risk of bleeding and thrombotic events in patients continuing or discontinuing these medications. We aimed to analyze the safety of continued antithrombotic therapy during open inguinal hernia repair.
Methods
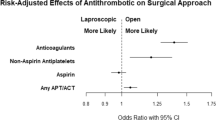
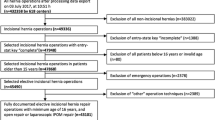
In this single-center, retrospective study, 4870 adult patients who underwent open inguinal hernia repair surgery by the same surgeon from 2008 January to 2019 March were included. Patients who underwent surgery while continuing antithrombotic therapy were included in the antithrombin group (n = 523) while those who were not under any antithrombotic therapy during the surgery were included in the control group (n = 4333). Using propensity score-matching, we then selected patients from each group with similar backgrounds. Surgery time, anesthesia time, postoperative bleeding, reoperation, and thrombotic event data were compared between the groups. Subgroup analysis based on the type of medications used was performed within the antithrombin group.
Results
Ten patients in the antithrombin group and seven patients in the control group experienced postoperative bleeding (p < 0.001). The rate of postoperative bleeding was the highest in patients taking multiple medications. However, most were managed conservatively. Three patients from the antithrombin group experienced thrombotic events postoperatively (p = 0.001).
Conclusions
Patients receiving continued antithrombotic therapy had an increased risk of minor postoperative bleeding; however, they are a high-risk group for thrombotic events.

Similar content being viewed by others
References
Yeung LYY, Sarani B, Weinberg JA, McBeth PB, May AK (2016) Surgeon's guide to anticoagulant and antiplatelet medications part two: antiplatelet agents and perioperative management of long-term anticoagulation. Trauma Surg Acute Care Open 1(1):e000022. https://doi.org/10.1136/tsaco-2016-000022
Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, Dunn AS, Kunz R (2012) Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e326S–e350S. https://doi.org/10.1378/chest.11-2298
van Veen JJ, Makris M (2015) Management of peri-operative anti-thrombotic therapy. Anaesthesia 70(Suppl 1):58–67. https://doi.org/10.1111/anae.12900e21-53
Capodanno D, Musumeci G, Lettieri C, Limbruno U, Senni M, Guagliumi G, Valsecchi O, Angiolillo DJ, Rossini R (2015) Impact of bridging with perioperative low-molecular-weight heparin on cardiac and bleeding outcomes of stented patients undergoing non-cardiac surgery. Thromb Haemostasis 114(2):423–431. https://doi.org/10.1160/th14-12-1057
Igarashi K, Takizawa K, Kakushima N, Tanaka M, Kawata N, Yoshida M, Ito S, Imai K, Hotta K, Ishiwatari H, Matsubayashi H, Ono H (2017) Should antithrombotic therapy be stopped in patients undergoing gastric endoscopic submucosal dissection? Surg Endosc 31(4):1746–1753. https://doi.org/10.1007/s00464-016-5167-4
Palamaras I, Semkova K (2015) Perioperative management of and recommendations for antithrombotic medications in dermatological surgery. Br J Dermatol 172(3):597–605. https://doi.org/10.1111/bjd.13362
Chen G, Barkmeier AJ (2014) Perioperative management of antithrombotic medications in vitreoretinal surgery. Int Ophthalmol Clin 54(2):199–213. https://doi.org/10.1097/iio.0000000000000024
Dezsi CA, Dezsi BB, Dezsi AD (2017) Management of dental patients receiving antiplatelet therapy or chronic oral anticoagulation: a review of the latest evidence. Eur J Gen Pract 23(1):196–201. https://doi.org/10.1080/13814788.2017.1350645
Kockerling F, Roessing C, Adolf D, Schug-Pass C, Jacob D (2016) Has endoscopic (TEP, TAPP) or open inguinal hernia repair a higher risk of bleeding in patients with coagulopathy or antithrombotic therapy? Data from the Herniamed Registry. Surg Endosc 30(5):2073–2081. https://doi.org/10.1007/s00464-015-4456-7
Chu EW, Chernoguz A, Divino CM (2016) The evaluation of clopidogrel use in perioperative general surgery patients: a prospective randomized controlled trial. Am J Surg 211(6):1019–1025. https://doi.org/10.1016/j.amjsurg.2015.05.036
Antolovic D, Rakow A, Contin P, Ulrich A, Rahbari NN, Buchler MW, Weitz J, Koch M (2012) A randomised controlled pilot trial to evaluate and optimize the use of anti-platelet agents in the perioperative management in patients undergoing general and abdominal surgery—the APAP trial (ISRCTN45810007). Langenbeck's Arch Surg 397(2):297–306. https://doi.org/10.1007/s00423-011-0867-7
Zeb MH, Pandian TK, El Khatib MM, Naik ND, Chandra A, Morris DS, Smoot RL, Farley DR (2016) Risk factors for postoperative hematoma after inguinal hernia repair: an update. J Surg Res 205(1):33–37. https://doi.org/10.1016/j.jss.2016.06.002
Sanders DL, Shahid MK, Ahlijah B, Raitt JE, Kingsnorth AN (2008) Inguinal hernia repair in the anticoagulated patient: a retrospective analysis. Hernia 12(6):589–592. https://doi.org/10.1007/s10029-008-0405-xdiscussion 667-588
Ho CH, Wu CC, Wu CC, Tsai YC (2018) Laparoscopic total extraperitoneal inguinal hernia repair is safe and feasible in patients with continuation of antithrombotics. J Minim Access Surg. https://doi.org/10.4103/jmas.JMAS_128_18
Ong W, Shen T, Tan WB, Lomanto D (2016) Is preoperative withdrawal of aspirin necessary in patients undergoing elective inguinal hernia repair? Surg Endosc 30(12):5542–5549. https://doi.org/10.1007/s00464-016-4926-6
McLemore EC, Harold KL, Cha SS, Johnson DJ, Fowl RJ (2006) The safety of open inguinal herniorraphy in patients on chronic warfarin therapy. Am J Surg 192(6):860–864. https://doi.org/10.1016/j.amjsurg.2006.08.058
Sundstrom J, Hedberg J, Thuresson M, Aarskog P, Johannesen KM, Oldgren J (2017) Low-dose aspirin discontinuation and risk of cardiovascular events: a Swedish Nationwide, population-based cohort study. Circulation 136(13):1183–1192. https://doi.org/10.1161/circulationaha.117.028321
Vene N, Mavri A, Gubensek M, Tratar G, Vizintin Cuderman T, Pohar Perme M, Blinc A (2016) Risk of thromboembolic events in patients with non-valvular atrial fibrillation after dabigatran or rivaroxaban discontinuation—data from the ljubljana registry. PLoS ONE 11(6):e0156943. https://doi.org/10.1371/journal.pone.0156943
Garcia DA, Regan S, Henault LE, Upadhyay A, Baker J, Othman M, Hylek EM (2008) Risk of thromboembolism with short-term interruption of warfarin therapy. Arch Intern Med 168(1):63–69. https://doi.org/10.1001/archinternmed.2007.23
Eisenberg MJ, Richard PR, Libersan D, Filion KB (2009) Safety of short-term discontinuation of antiplatelet therapy in patients with drug-eluting stents. Circulation 119(12):1634–1642. https://doi.org/10.1161/circulationaha.108.813667
Mashour GA, Shanks AM, Kheterpal S (2011) Perioperative stroke and associated mortality after noncardiac, nonneurologic surgery. Anesthesiology 114(6):1289–1296. https://doi.org/10.1097/ALN.0b013e318216e7f4
Acknowledgements
Dr. Kyosuke Miyazaki is an advisor to BARD.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
This retrospective study was approved by the institutional review board of Hokkaido University (Med 18-037). The notice for this retrospective study was published on the website of the institute and the patients were given the right to opt out.
Human and animal rights
Animals were not used in this study.
Informed consent
Prior to surgery, the risk of both continuation or cessation of antithrombotic medications was explained to all the patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Poudel, S., Miyazaki, K. & Hirano, S. Continuation of antithrombotic therapy increases minor bleeding but does not increase the risk other morbidities in open inguinal hernia repair: A propensity score-matched analysis. Hernia 24, 857–865 (2020). https://doi.org/10.1007/s10029-020-02169-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02169-8