Abstract
Objectives
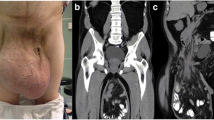
The laparoscopic trans-abdominal preperitoneal (TAPP) approach to inguinal hernia repair is well documented as an excellent choice in numerous studies, especially when conducted by an experienced surgeon. Its full list of specific indications is still under debate. Generally, the repair of scrotal hernias demands a higher level of experience on the part of the surgeon, irrespective of the applied surgical technique. In this report, we evaluate our preliminary experience of TAPP laparoscopic repair for inguinoscrotal hernias in young patients in a Community Hospital setting, focusing on the feasibility of the technique and the incidence of complications.
Materials and methods
Between January 2008 and January 2009 a total of ten consecutive young patients at the “Civil Hospital” in Vittorio Veneto (TV), underwent TAPP laparoscopic repair of bilateral inguinoscrotal hernias.
Results
The overall mean operative time was 65 (±15) min. All procedures were performed on a day surgery basis. There were no conversions to open repair, no mortality/morbidity or relapsing hernias. The mean follow-up was 14 (±2) months. No patients reported severe pain at 10 days, There were no reports of night pain at 30 days. All patients had a return to physical-work capacity within 14 days. All patients were completely satisfied at the 3-month follow up.
Conclusions
Analysis of the short-term post-operative outcomes of our experience enabled us to conclude that, in the proper setting, TAPP can be performed for inguinoscrotal hernia repair with an efficiency comparable to that of normal inguinal hernia repair.
Similar content being viewed by others
References
Fingerhut A, Millat B, Veyrie N, Chouillard E, Dziri C (2006) Inguinal hernia repair—update 2006. In: Sauerland S, Fingerhut A, Millat B, Buess E (eds) EAES guidelines for endoscopic surgery—neugebauer EAM. Springer, Berlin
Heikkinen T, Bringman S, Ohtonen P, Kunelius P, Haukipuro K, Hulkko A (2004) Five-year outcome of laparoscopic and Lichtenstein hernioplasties. Surg Endosc 18(3):518–522
Bencini L, Lulli R, Mazzetti MP (2007) Experience of laparoscopic hernia repair in a laparoscopically oriented unit of a large community hospital. J Laparoendosc Adv Surg Rech 17(2):200–204
Agresta F, Mazzarolo G, Bedin N (2009) Inguinal hernia repair in a community hospital setting: have attitudes changed because of laparoscopy? A review of a general surgeon’s experience over the last 5 years. Surg Laparosc Endosc Percutan Techn 19:267–271
Bittner R, Schmedt CG, Scwarz J, Kraft K, Leibl BJ (2002) Laparoscopic transperitoneal procedures for routine repair of groin hernia. Br J Surg 89(8):1062–1066
Mahon D, Decadt B, Rhodes M (2003) Prospective randomized trial of laparoscopic (transabdominal preperitoneal) vs open (mesh) repair for bilateral and recurrent inguinal hernia. Surg Endosc 17(9):1386–1390
McCornack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, Vale L, Grant A (2005) Laparoscopic surgery for inguinal repair: systematic review of effectiveness and economic evaluation. Health Technol Assess 9(14):1–203, iii–iv
Miserez M (2004) Inguinal hernia repair in general surgical practice 2004: more than laparoscopy training is the keyword. Acta Chir Belg 104(4):422–424
Butters M, Redecke J, Koninger J (2007) Long-term results of a randomized clinical trial of Shouldice, Lichtenstein and transabdominal preperitoneal hernia repairs. Br J Surg 94(5):562–565
Miserez M, Alexandre JH, Campanelli G, Corcione F, Cuccurullo D, Pascual MH, Hoeferlin A, Kingsnorth AN, Mandala V, Palot JP, Schumpelick V, Simmermacher RK, Stoppa R, Flament JB (2007) The European hernia society groin hernia classification: simple and easy to remember. Hernia 11(2):113–116
Libl BJ, Scmedt KK, Ulrich M, Bittner R (2000) Scrotal hernias: a contraindication for an endoscopic procedure? Results of a single institution experience in transabdominal repair. Surg Endosc 14:289–292
Ferzli GS, Kiel T (1997) The role of the endoscopic extraperitoneal apporach in large inguinal scrotal hernias. Surg Endosc 11:299–302
Wake BL, McCormack K, Fraser C, Vale L, Perez J, Grant AM (2005) Transabdominal pre-peritoneal (TAPP) vs totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair. Cochrane Database Syst Rev 25(1):CD004703
O’Dwyer PJ, Kingsnorth AN, Molloy RG, Small PK, Lammers B, Horeyseck G (2004) Randomized clinical trial assessing impact of a lightweight or heavyweight mesh on chronic pain after inguinal hernia repair. Br J Surg 92(2):166–170
Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L, Faillace G, Longoni M (2007) Use of human fibrin sealant (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty. Ann Surg 245(2):222–232
Topart P, Vandenbroucke F, Lozac’h P (2005) Tisseel vs tack staples as mesh fixation in totally extraperitoneal laparoscopic repair of groin hernias. A retrospective analysis. Surg Endosc 19:724–727
Anadol ZA, Ersoy E, Taneri F, Tekin E (2004) Outcome and cost comparison of laparoscopic transabdominal preperitoneal hernia repair versus open liechtenstein technique. J Laparoendosc Adv Surg Tech 14(3):159–163
Singhal T, Balakrishnan S, Grandy-Smith S, El-Hasani S (2007) Consolidated five-year experience with laparoscopic inguinal hernia repair. Surgeon 5(3):137–140
Olmi S, Scaini A, Erba L, Guaglio M, Croce E (2007) Quantification of pain in laparoscopic transabdominal preperitoneal (TAPP) inguinal hernioplasty identifies marked differences between prosthesis fixation systems. Surgery 142(1):40–46
Bozuk M, Schuster R, Stewart D, Hicks K, Greaney G, Waxman K (2003) Disability and chronic pain after open mesh and laparoscopic inguinal hernia repair. Am Surg 69(10):839–841
Bueno J, Serralta A, Planells M, Rodero D (2004) Inguinodynia after two inguinal herniorrhaphy methods. Surg Laparosc Endosc Percutan Tech 14(4):210–214
Gholghesaei M, Langeveld HR, Veldkamp R, Bojer HJ (2005) Costs and quality of life after endoscopic repair of inguinal hernia vs open tension-free repair. Surg Endosc 19:816–821
Acknowledgment
The authors want to thank J.A. Mawer from the UK for linguistic review of the manuscript.
Conflict of interest statement
All authors declare that they have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Agresta, F., Mazzarolo, G., Balbi, P. et al. Inguinal-scrotal hernias in young patients: is laparoscopic repair a possible answer? Preliminary results of a single-institution experience with a transabdominal preperitoneal approach. Hernia 14, 471–475 (2010). https://doi.org/10.1007/s10029-010-0677-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-010-0677-9