Abstract
Purpose
High success rates and minimal complications have consolidated arthroscopy as the therapeutic alternative of choice for minimally invasive treatment of internal disorders (ID) of the temporomandibular joint (TMJ). However, there is no certainty regarding the demographic and clinical factors associated with the technique’s success or failure. This study was performed to analyze the effectiveness of arthroscopy regarding pain and the mandibular dynamics and also to determine whether variables such as age, sex, and preoperative Wilkes stage influence the results.
Methods
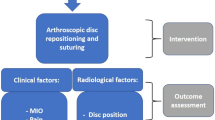
A retrospective study was conducted involving 92 patients with ID of the TMJ between September 2017 and February 2020. In all cases, a first stage of intra-articular lysis and lavage was executed. As needed, a phase of operative arthroscopy or arthroscopic discopexy was implemented.
Results
A total of 152 arthroscopies were performed. Both the variation in pain and mouth opening in patients with ID of the TMJ treated were statistically significant for the follow-up periods studied. Better results were observed for patients with lower Wilkes stages. No association with age was found.
Conclusion
Based on the results, we recommend early intervention as soon as an ID in the TMJ is detected.




Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author F.S The data are not publicly available due to them containing information that could compromise research participant privacy/consent.
References
Israel HA (2016) Internal derangement of the temporomandibular joint: new perspectives on an old problem. Oral Maxillofac Surg Clin North Am 28(3):313–333. https://doi.org/10.1016/j.coms.2016.03.009
Haeffs TH, D’Amato LN, Khawaja SN, Keith DA, Scrivani SJ (2018) What variables are associated with the outcome of arthroscopic lysis and lavage surgery for internal derangement of the temporomandibular joint? J Oral Maxillofac Surg 76(10):2081–2088. https://doi.org/10.1016/j.joms.2018.04.018
Wilkes C (1989) Internal derangements of the temporomandibular joint. Arch Otolaryngol Head Neck Surg 115:470–477
Bronstein SL, Merril R (1992) Clinical staging for TMJ internal derangement application to arthroscopy. J Craniomandib Disord 6(1):7–16
Sanders B (1986) Arthroscopic surgery of the temporomandibular joint: treatment of internal derangement with persistent closed lock. Oral Surgery Oral Med Oral Pathol 62(4):361–372. https://doi.org/10.1016/0030-4220(86)90282-3
Al-Moraissi EA (2015) Open versus arthroscopic surgery for the management of internal derangement of the temporomandibular joint: a meta-analysis of the literature. Int J Oral Maxillofac Surg 44(6):763–770. https://doi.org/10.1016/j.ijom.2015.01.024
da Silva PA, de Fatima Fernandes Lopes MT, Freire FS (2015) A prospective study of 138 arthroscopies of the temporomandibular joint. Braz J Otorhinolaryngol 81(4):352–357. https://doi.org/10.1016/j.bjorl.2014.08.021
McCain JP, Sanders B, Koslin MG, Quinn JD, Peters PB, Indresano AT (1992) Temporomandibular joint arthroscopy: a 6-year multicenter retrospective study of 4,831 joints. J Oral Maxillofac Surg 50(9):926–930. https://doi.org/10.1016/0278-2391(92)90047-4
González-García R, Rodríguez-Campo FJ, Monje F, Sastre-Pérez J, Gil-Díez Usandizaga JL (2008) Operative versus simple arthroscopic surgery for chronic closed lock of the temporomandibular joint: a clinical study of 344 arthroscopic procedures. Int J Oral Maxillofac Surg 37(9):790–796. https://doi.org/10.1016/j.ijom.2008.04.022
González-García R, Rodríguez-Campo FJ (2011) Arthroscopic lysis and lavage versus operative arthroscopy in the outcome of temporomandibular joint internal derangement: a comparative study based on Wilkes stages. J Oral Maxillofac Surg 69(10):2513–2524. https://doi.org/10.1016/j.joms.2011.05.027
Al-Moraissi EA, Wolford LM, Ellis E, Neff A (2020) The hierarchy of different treatments for arthrogenous temporomandibular disorders: a network meta-analysis of randomized clinical trials. J Cranio-Maxillofacial Surg 48(1). https://doi.org/10.1016/j.jcms.2019.10.004
McCain JP, Hossameldin RH (2011) Advanced arthroscopy of the temporomandibular joint. Atlas Oral Maxillofac Surg Clin North Am 19(2):145–167. https://doi.org/10.1016/j.cxom.2011.06.001
Mccain P, Podrasky ANNE, Zabiegalski NA (1992) Arthroscopic disc repositioning and suturing: a preliminary report. J Oral Maxillofac Surg 50:568–579
Murakami KI (2013) Rationale of arthroscopic surgery of the temporomandibular joint. J Oral Biol Craniofacial Res 3(3):126–134. https://doi.org/10.1016/j.jobcr.2013.07.002
Breik O, Devrukhkar V, Dimitroulis G (2016) Temporomandibular joint (TMJ) arthroscopic lysis and lavage: outcomes and rate of progression to open surgery. J Cranio-Maxillofacial Surg 44(12):1988–1995. https://doi.org/10.1016/j.jcms.2016.09.017
Abboud W, Nadel S, Yarom N, Yahalom R (2016) Arthroscopy of the temporomandibular joint for the treatment of chronic closed lock. Isr Med Assoc J 18(7):397–400
Muñoz-Guerra MF, Rodríguez-Campo FJ, Escorial-Hernández V, Brabyn PJ, Fernández-Domínguez M, Naval-Gías L (2021) Is there a relationship between age, personal factors or surgical findings, and outcome after temporomandibular joint arthroscopy? J Oral Maxillofac Surg 79(5):1000–1008. https://doi.org/10.1016/j.joms.2020.12.016
Abboud W, Yahalom R, Givol N (2015) Treatment of intermittent locking of the jaw in Wilkes Stage II Derangement by Arthroscopic Lysis and Lavage. J Oral Maxillofac Surg 73(8):1466–1472. https://doi.org/10.1016/j.joms.2015.02.027
Werkman DF, Carver KZ, Harper DE, Troost JP, Aronovich S (2022) Are outcomes of temporomandibular joint arthroscopy influenced by central sensitization?. J Oral Maxillofac Surg 80(6):980–988. https://doi.org/10.1016/j.joms.2022.02.009
Cho J, Israel H (2017) Does the age of a patient affect the outcome of temporomandibular joint arthroscopic surgery?. J Oral Maxillofac Surg 75(6):1144–1150. https://doi.org/10.1016/j.joms.2016.10.038
Askar H, Aronovich S, Christensen BJ, McCain J, Hakim M (2021) Is arthroscopic disk repositioning equally efficacious to open disk repositioning? A systematic review. J Oral Maxillofac Surg 79(10):2030–2041.e2. https://doi.org/10.1016/j.joms.2021.02.007
Muñoz-Guerra MF, Rodríguez-Campo FJ, Escorial-Hernández V, Sanz-García A, Brabyn PJ, Fernández-Domínguez M (2022) Temporomandibular joint arthroscopy in advanced stages of internal derangement: a retrospective cohort study on the influence of age. Int J Oral Maxillofac Surg. https://doi.org/10.1016/j.ijom.2021.12.009
Sharawy M, Ali AM, Choi WS, Larke V (2000) Ultrastructural characterization of the rabbit mandibular condyle following experimental induction of anterior disk displacement. Cells Tissues Organs 167(1):38–48. https://doi.org/10.1159/000016765
Cai XY, Jin JM, Yang C (2011) Changes in disc position, disc length, and condylar height in the temporomandibular joint with anterior disc displacement: a longitudinal retrospective magnetic resonance imaging study. J Oral Maxillofac Surg 69(11):e340–e346. https://doi.org/10.1016/j.joms.2011.02.038
Acknowledgements
The authors thank Prof. Dr. Benjamín Martinez for assistance with the statistical analysis.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Carlos Gaete, Christian Droguett, Felipe Sáez and Paula Astorga. The first draft of the manuscript was written by Felipe Sáez and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the hospital ethics board, which complies with the Declaration of Helsinki. The patients accepted for this study approved and signed an informed consent form allowing clinical photographs to be published.
Consent for publication
Patients signed informed consent regarding publishing their data and photographs
Competing interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: one of the authors (C.G) received a speaking fee from Johnson & Johnson. However Johnson & Johnson played no role in data analysis or preparation of the manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gaete, C., Droguett, C., Sáez, F. et al. Clinical and demographic factors associated with the effectiveness of temporomandibular joint arthroscopy. Oral Maxillofac Surg 28, 405–411 (2024). https://doi.org/10.1007/s10006-023-01158-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-023-01158-2