Abstract
Purpose
The aim of this study was to evaluate the influence of cyclobenzaprine and dexamethasone on the electrical activity of the masticatory muscles in patients who had undergone lower third molar surgery.
Methods
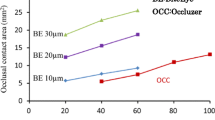
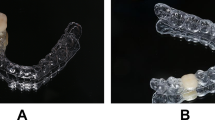
Thirty bilateral impacted lower third molars with indication of extraction were randomised into three groups: the control group, the dexamethasone, and the cyclobenzaprine group. To obtain muscular electrical activity and mouth opening, an electromyographic device was used at mandibular rest and maximum voluntary contraction and compared pre- and post-operatively.
Results
During muscle contraction, no significant difference was observed in the electromyographic records on the non-operated side. On the operated side, there was a reduction in electrical activity for both drugs pre-operatively and immediately post-operatively compared to the control group. All pharmacological agents promoted a higher mouth opening compared to control group.
Conclusion
The results suggest that dexamethasone and cyclobenzaprine may be useful as an adjuvant in the prevention of motor dysfunctions in third molar surgery.






Similar content being viewed by others
References
Raldi FV, Moraes MB, Nascimento RD, Santamaria MP, Amorim JBO, Paula FA (2011) The role of electromyography in dentistry. Braz Dent Sci 14:60–65
Rossi-Junior WC, Esteves A, Bérzin F, Couto Filho CEG, Nogueira DA, Villela GA Jr (2011) Masseter and extraction of third molars: electromyographic evaluation. Rev Cir Traumatol Buco-Maxilo-Fac 11:101–108
Flores JA, Machado E, Machado P, Flores FW, Mezomo MB (2007) Avaliação da prevalência de trismo em pacientes submetidos a exodontia de terceiros molares. RGO 55:17–22
Souza JA, Consone DP (1992) Método para medida do edema facial. RGO 40:137–139
Boer PJ, Raghoebar GM, Stegenga B, Schoen PJ, Boering G (1995) Complications after mandibular third molar extraction. Quintessence Int 26:779–784
Weber CR, Griffin JM (1994) Evaluation of dexamethasone for reducing postoperative edema and inflammatory response after orthognathic surgery. J Oral Maxillofac Surg 52:35–39
Raldi FV, Sá-Lima JR, Zanotti GG, Moraes MB (2006) Avaliação da eficácia da dexametasona no pós-operatório de terceiros molares. Revista Internacional de Cirurgia e Traumatologia Bucomaxilofacial 4:251–257
Delegado JHO, Fernandes JMT, Salinas BB (1997) Estudio comparativo entre ibuprofeno, dexametasona y betametasona em el control del edema postoperatorio em cirurgia de terceros molares retenidos. Revista ADM 2:88–91
Ensen E, Tasar F, Akhan O (1999) Determination of the anti-inflammatory effects of methylprednisolone on the sequelae of third molar surgery. J Oral Maxillofac Surg 57:1201–1206
Lima CA, Favarini V, Torres AM, Silva RA, Sato FRL (2017) Oral dexamethasone decreases postoperative pain, swelling, and trismus more than diclofenac following third molar removal: a randomized controlled clinical trial. Oral Maxillofac Surg 21:321–326
Yuasa H, Sugiura M (2004) Clinical postoperative findings after removal of impacted mandibular third molars: prediction of postoperative facial swelling and pain based on preoperative variables. Br J Oral Maxillofac Surg 42:209–214
Benediktsdóttir IS, Wenzel A, Petersen JK (2004) Mandibular third molar removal: risk indicators for extended operation time, postoperative pain, and complications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 97:438–446
Korokolvas A (2015) Dicionário Terapêutico Guanabara. Guanabara-Koogan, Rio de Janeiro
Linden CH, Mitchiner JC, Lindzon RD (1983) Cyclobenzaprine overdosage. J Toxicol Clin Toxicol 20:281–288
Katz WA, Dube J (1988) Cyclobenzaprine in the treatment of acute muscle spasm: review of a decade of clinical experience. Clin Ther 10:216–228
Yagiela JA, Dowd FJ, Johnson BS, Mariotti A, Neidle E (2010) Pharmacology and therapeutics for dentistry. Mosby, Maryland
Merletti R (1999) The standards for reporting Emg data. J Electromyogr Kinesiol 9:3–4
Ahlgren JG, Ingerval BF, Thilander BL (1985) Surface and intramuscular EMG from the temporales muscle. A study of methods. Electromyogr Clin Neurophysiol 25:353–357
Portney LG, Roy SH (2004) Eletromiografia e testes de velocidade de condução nervosa. In: O’Sullivan S, Schmitz JT (eds) Fisioterapia – Avaliação e Tratamento. Manole, São Paulo
Pignataro Neto G, Berzin F, Rontani RMP (2004) Identificação do lado de preferência mastigatória através do exame eletromiográfico comparado ao visual. R Dent Press Ortodon Ortopedi Fac 9:77–85
Jung JW, Song KH, Chee Y (2010) Eletromyographic activity of the masseter muscle after radiofrequency therapy in an animal model. Oral Maxillofac Surg 14:35–41
Borrini CB. (2005) Analise da atividade eletromiografica de musculos mastigatorios em portadores de disfunção temporomandibular durante a mastigação. Piracicaba, 134p. Dissertação (Mestrado em Odontologia) – Faculdade de Odontologia de Piracicaba, Universidade Estadual de Campinas
Pontes RT, Orsini M, Freitas MRG (2008) Alterações Da Fonação E Deglutição Na Esclerose Lateral Amiotrófica: Revisão de Literatura. Revista Neurociência 18:69–73
Seymour RA, Walton JG (1984) Pain control after third molar surgery. J Oral Surg 13:457–485
Ferrario VF, Sforza C, Zanotti G (2004) Maximal bite forces in healthy young adults as predicted by surface electromyography. J Dent 32:451–457
Ahmad M, Hollender L, Anderson Q (2009) Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107:844–860
Hermens HJ (1999) European recommendations for surface electromyography – results of the SENIAM project. Roessingh Research and Development, Netherlands, pp 1–3
Hermens HJ, Freriks B, Disselhorst-Klug C (2000) Development of recommendations for SEMG sensor and sensor placement procedures. J Electromyogr Kinesiol 10:361–374
Castroflorio T, Icardi K, Torsello F (2005) Reproducibility of surface EMG in the human masseter and anterior temporalis muscle areas. Cranio 23:130–137
Hermens HJ, Merletti R, Freriks B. (1999) The state of the art on signal processing methods for surface EletroMyoGraphy, deliverable of the SENIAM project. Roessingh Research and Development, p 17–19
Soderberg GL, Knutson LM (2000) A guide for use and interpretation of kinesiologic electromyographic data. Phys Ther 80:485–498
Albornoz M, Ogalde A, Aguirre M (2009) Estudio radiográfico y electromiográfico de los músculos masetero y temporal anterior em indivíduos com maloclusion tipo II, 1 de angle y controles. Int J Morphol 27:861–866
Ernberg M, Schopka JH, Fougeront N (2007) Changes in jaw muscle EMG activity and pain after third molar surgery. J Rehabil 34:15–26
Bérzin, F. (2001) Estudo eletromiográfico da hipoatividade de músculos da mastigação em pacientes portadores de desordem cranio-mandibular (DCM), com dor miofacial. In: Anais do 5° Simpósio Brasileiro e Encontro Internacional sobre Dor, São Paulo, 292
Amorim MM, Borini CB, Lopes SLPC, Haiter Neto F, Berzin F, Caria PHF (2008) Relationship between the inclination of the coronoid process of the mandible and the electromyographic activity of the mandible and the electromyographic activity of the temporal muscle in skeletal class I and II individuals. J Oral Sci 50:293–299
Kroll CD. (2009) Avaliação da Ansiedade e da atividade eletromiografica dos músculos elevadores da mandibula em mulheres com disfunção temporomandibular [Tese] Piracicaba UNICAMP/FOP
Sato FRL, Asprino L, de Araújo DE, Moraes M (2009) Short-term outcome of postoperative patient recovery perception after surgical removal of third molars. J Oral Maxillofac Surg 67:1083–1091
Mehra P, Reebye U, Nadershah M (2013) Efficacy of anti-inflammatory drugs in third molar surgery: a randomized clinical trial. Int J Oral Maxillofac Surg 42:835–842
Brunton L, Knollmann B, Hilal-Danda R (2017) Goodman and Gilman’s the pharmacological basis of therapeutics. McGraw-Hill Education, New York
Baxendale BR, Vater M, Lavery KM (1993) Dexamethasone reduces pain and swelling following extraction of third molar teeth. Anaesthesia 48:961–964
Dan AEB, Thygesen TH, Pinholt E (2010) Corticosteroid administration in oral and orthognathic surgery: a systematic review of the literature and meta-analysis. J Oral Maxillofac Surg 68:2207–2220
Nesi H, Vicente A, Loffi (2013) Uso de corticosteroide no pré-operatório em cirurgia de terceiros molares. Rev Bras Odontol 70:22–27
Herrera-Briones FJ, Prados Sánchez E, Reyes Botella C, Vallecillo Capilla M (2013) Update on the use of corticosteroids in third molar surgery: systematic review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol 116:342–351
Ngeow WC, Lim D (2016) Do corticosteroids still have a role in the management of third molar surgery? Adv Ther 33:1105–1139
Lim D, Ngeow WC (2017) A comparative study on the efficacy of submucosal injection of dexamethasone versus methylprednisolone in reducing postoperative sequelae after third molar surgery. J Oral Maxillofac Surg 75:2278–2286
Chugh A, Singh S, Mittal Y, Chugh V (2018) Submucosal injection of dexamethasone and methylprednisolone for the control of postoperative sequelae after third molar surgery: randomized controlled trial. Int J Oral Maxillofac Surg 47:228–233
Mathias IF, Campos MA, Amorim JBO, Moraes MB, Nascimento RD, Santamaria MP, Raldi FV (2013) The influence of single-dose dexamethasone on masseter and temporal muscles after impacted lower third molar extraction. Pilot study through electromyography evaluation. Braz Dent Sci 16:65–76
Grossi GB, Maiorana C, Garramone RA, Borgonovo A, Beretta M, Farronato D, Santoro F (2007) Effect of submucosal injection of dexamethasone on postoperative discomfort after third molar surgery: a prospective study. J Oral Maxillofac Surg 65:2218–2226
Santos TS, Calazans ACM, Martins-Filho PRS (2011) Evaluation of the muscle relaxant cyclobenzaprine after third-molar extraction. JADA 142:1154–1162
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the local ethics committee.
Informed consent
Informed consent was obtained from all participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Raldi, F.V., Nascimento, R.D., Sato, F.R.L. et al. Evaluation of the impact of preoperative use of dexamethasone and cyclobenzaprine in surgical extraction of lower third molars on trismus by electromyographic analysis. Oral Maxillofac Surg 23, 395–405 (2019). https://doi.org/10.1007/s10006-019-00776-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-019-00776-z