Abstract
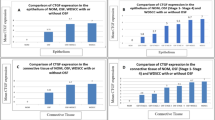
This paper focuses on the status of epithelial markers, E-cadherin, and p63 in the backdrop of an abnormal amount of collagen in the sub-mucosa of dysplastic and non-dysplastic grades of OSF. Histologically confirmed OSF and normal oral mucosa samples were procured. Samples were stained by Van Gieson’s stain (VG) and immunohistochemistry. The captured images were analyzed by ImageJ software to quantify their grayscale intensities. There was a gradual increase in the intensity of VG stain from normal to non-dysplastic and dysplastic OSF and the differences in their mean grayscale values were found to be significant (p < 0.00001). The intensity of E-cadherin was found to be the highest in non-dysplastic conditions and lowest in dysplastic conditions. The intensity difference of E-cadherin between normal and non-dysplastic OSF was found to be significant (p < 0.00001). The grayscale scale intensity values for p63 in whole epithelium depicted significant differences between normal and diseased conditions but for its intensity, in basal cells, significant differences were found between non-dysplastic and other classes of tissues. There was a positive correlation observed between VG and p63 staining intensity. The diseased oral epithelium demonstrated greater deposition of sub-epithelial collagen fibers along with subsequent loss of E-cadherin and an increased p63 expression.


Similar content being viewed by others
References
International Agency for Research on Cancer Lip, oral cavity: Globocan 2018 [Internet]. The Global Cancer Observatory, WHO. 2019. https://gco.iarc.fr/today/data/factsheets/cancers/1-Lip-oral-cavity-fact-sheet.pdf.
International Agency for research on cancer. Lip and oral cavity cancer statistics in India: GLOBOCAN 2018 [Internet]. WHO. 2019. https://gco.iarc.fr/today/data/factsheets/populations/356-india-fact-sheets.pdf.
Iocca O, Sollecito TP, Alawi F, Weinstein GS, Newman JG, De Virgilio A et al (2020) Potentially malignant disorders of the oral cavity and oral dysplasia: a systematic review and meta-analysis of malignant transformation rate by subtype. Head Neck 42(3):539–555
Phookan J, Saikia KP (1998) A clinicopathological study of the pre-malignant conditions of oral cavity. Indian J Otolaryngol Head Neck Surg 50(3):246–249. https://doi.org/10.1007/BF03007000
Yardimci G, Kutlubay Z, Engin B (2014) YTG. Precancerous lesions of oral mucosa. World J Clin Cases. 2(12):866–73.
Wheelock MJ, Jensen PJ (1992) Regulation of keratinocyte intercellular junction organization and epidermal morphogenesis by E-cadherin. J Cell Biol 117(2):415–425
Neville B, Damm D.D, Allen C, Chi A. Color Atlas of oral and maxillofacial diseases. 11th December 2018, 1st Edition. Elsevier, Philadelphia. ISBN: 978–0–323–55225–7.
Diniz-Freitas M, García-Caballero T, Antúnez-López J, Gándara-Rey JM, García-García A (2006) Reduced E-cadherin expression is an indicator of unfavourable prognosis in oral squamous cell carcinoma. Oral Oncol 42(2):190–200
Kaur G, Carnelio S, Rao N, Rao L (2009) Expression of E-cadherin in primary oral squamous cell carcinoma and metastatic lymph nodes : an immunohistochemical study. 20(1):71–6
Hulmes DJ (2002) Building collagen molecules, fibrils, and suprafibrillar structures. J Struct Biol 137(1–2):2–10. https://doi.org/10.1006/jsbi.2002.4450
Kaur P, Kakar V (2012) Collagen: role in oral tissues: a review. Int J Sci Res ISSN (Online Impact Factor. 3(5):2319–7064.
Kamath V, Rajkumar K, Kumar A (2015) Expression of type I and type III collagens in oral submucous fibrosis: an immunohistochemical study. J Dent Res Rev 2(4):161
Dellavalle RP, Walsh P, Marchbank A, Grayson TE, Su LJ, Parker ER et al (2002) CUSP/p63 expression in basal cell carcinoma. Exp Dermatol 11(3):203–208
Gatti V, Bongiorno-Borbone L, Fierro C, Annicchiarico-Petruzzelli M, Melino G, Peschiaroli A. p63 at the Crossroads between Stemness and Metastasis in Breast Cancer. Int J Mol Sci. 2019;20(11):2683. Published 2019 May 31. https://doi.org/10.3390/ijms20112683.
Sharma M, Fonseca FP, Hunter KD et al (2020) Loss of oral mucosal stem cell markers in oral submucous fibrosis and their reactivation in malignant transformation. Int J Oral Sci 12:23. https://doi.org/10.1038/s41368-020-00090-5
Yang A, Schweitzer R, Sun D, Kaghad M, Walker N, Bronson RT et al (1999) P63 is essential for regenerative proliferation in limb. Craniofacial Epithelial Dev Nat 398(6729):714–718
Cho HJ, Lee HK, Kim DS, Na JI, Shin JW, Youn SW et al (2008) C-terminal peptide of IGFBP-3, KGRKR, prolongs the proliferative potential of basal keratinocytes. J Dermatol Sci 50(1):61–64
Hosoya A, Lee JM, Cho SW, Kim JY, Shinozaki N, Shibahara T et al (2008) Morphological evidence of basal keratinocyte migration during the re-epithelialization process. Histochem Cell Biol 130(6):1165–1175
Haniffa AM, Saitoh M, Abiko Y, Takeshima M, Nishimura M, Yamazaki M et al (2007) Expression pattern of p63 in oral epithelial lesions and submucous fibrosis associated with betel-quid chewing in Sri Lanka. Med Mol Morphol 40(4):203–207
Xavier FCA, Takiya CM, Reis SRA, Ramalho LMP (2009) P63 Immunoexpression in lip carcinogenesis. J Mol Histol 40(2):131–137
Saravanan C. Color image to grayscale image conversion. 2010 2nd Int Conf Comput Eng Appl ICCEA 2010. 2010;2(April 2010):196–9.
Kiernan JA (2008) Histological and Histochemical Methods: Theory and Practice, fourth ed. Bloxham, UK
Varghese F, Bukhari AB, Malhotra R, De A (2014) IHC Profiler: an open source plugin for the quantitative evaluation and automated scoring of immunohistochemistry images of human tissue samples. PLoS One. 9(5):e96801. Published 2014 May 6. https://doi.org/10.1371/journal.pone.0096801
Takiyama W, Moriwaki S, Mandai K, Takashima S (1996) Relationship of esophageal dysplasia to associated head and neck cancer in patients with esophageal carcinoma. Jpn J Clin Oncol 26(1):12–17
Kobayashi M, Kawachi H, Takizawa T, Uchida K, Sekine M, Kumagai J et al (2007) P53 mutation analysis of low-grade dysplasia and high-grade dysplasia/carcinoma in situ of the esophagus using laser capture microdissection. Oncology 71(3–4):237–245
Perez-Ordoñez B, Beauchemin M, Jordan RCK (2006) Molecular biology of squamous cell carcinoma of the head and neck. J Clin Pathol 59(5):445–453
Bedi R, Butterworth M CG et al. Opportunistic Oral Cancer Screening. British Dental Association. Occasional Paper. April 2000; Issue no. 6.
Pindborg JJ, Reichart PA, Smith CJ, van der Waal I. Berlin: Springer-Verlag; 1997. World Health Organization: Histological Typing of Cancer and Pre-cancer of the Oral Mucosa.
Lamouille S, Xu J, Derynck R (2014) Molecular mechanisms of epithelial-mesenchymal transition. Nat Rev Mol Cell Biol 15(3):178–196. https://doi.org/10.1038/nrm3758
Jang M, Koh I, Lee JE, Lim JY, Cheong JH, Kim P (2018) Increased extracellular matrix density disrupts E-cadherin/beta-catenin complex in gastric cancer cells. Biomater Sci 6(10):2704–2713
Choi HR, Batsakis JG, Zhan F, Sturgis E, Luna MA, El-Naggar AK (2002) Differential expression of p53 gene family members p63 and p73 in head and neck squamous tumorigenesis. Hum Pathol 33(2):158–164. https://doi.org/10.1053/hupa.2002.30722
Takeda T, Sugihara K, Hirayama Y, Hirano M, Tanuma JI, Semba I (2006) Immunohistological evaluation of Ki-67, p63, CK19 and p53 expression in oral epithelial dysplasias. J Oral Pathol Med 35(6):369–375. https://doi.org/10.1111/j.1600-0714.2006.00444.x
Chen Y-K, Hsue S-S (2005) Lin L-M Expression of p63 protein and mRNA in oral epithelial dysplasia. J Oral Pathol Med 34:232–239
Signoretti S, Waltregny D, Dilks J et al (2000) p63 is a prostate basal cell marker and is required for prostate development. Am J Pathol 157(6):1769–1775. https://doi.org/10.1016/S0002-9440(10)64814-6
Moll UM, Slade N (2004) p63 and p73: roles in development and tumor formation. Mol Cancer Res 2(7):371–386
Lindsay J, McDade SS, Pickard A, McCloskey KD, McCance DJ (2011) Role of DeltaNp63gamma in epithelial to mesenchymal transition. J Biol Chem 286(5):3915–3924. https://doi.org/10.1074/jbc.M110.162511
Das RK, Anura A, Pal M et al (2013) Epithelio-mesenchymal transitional attributes in oral sub-mucous fibrosis. Exp Mol Pathol 95(3):259–269. https://doi.org/10.1016/j.yexmp.2013.08.006
Das RK, Pal M, Barui A et al (2010) Assessment of malignant potential of oral submucous fibrosis through evaluation of p63, E-cadherin and CD105 expression. J Clin Pathol 63(10):894–899. https://doi.org/10.1136/jcp.2010.078964
Cherukuri P, DeCastro AJ, Balboni AL et al (2012) Phosphorylation of ΔNp63α via a novel TGFβ/ALK5 signaling mechanism mediates the anti-clonogenic effects of TGFβ. PLoS ONE 7(11):e50066. https://doi.org/10.1371/journal.pone.0050066
Acknowledgements
The authors would like to thank Guru Nanak Institute of Dental Science and Research, Kolkata; School of Medical Science and Technology, Indian Institute of Technology, Kharagpur and Centre for Biomaterial, Cellular and Molecular Theranostics, Vellore Institute of Technology, Vellore for providing support to carry out the research. We especially thank Vellore Institute of Technology (VIT), Vellore for providing institutional internal research funding (seed 2578).
Funding
No external funding was received for this work.
Author information
Authors and Affiliations
Contributions
SC: data acquisition, data analysis and interpretation, statistical analysis, manuscript preparation, and editing. RRP: study concept and study design. MP: study concept and study design. JC: study concept and study design. RKD: data acquisition, manuscript review and editing, study design, and study concept.
Corresponding author
Ethics declarations
Conflict of interest
The authors would like to declare that there is no conflict of interest.
Ethical clearance
Samples were collected under informed consent of patients and ethical clearance from GNIDSR (GNIDSR/IEC/07/16).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chakraborti, S., Paul, R.R., Pal, M. et al. Collagen deposition correlates with loss of E-cadherin and increased p63 expression in dysplastic conditions of oral submucous fibrosis. Med Mol Morphol 55, 20–26 (2022). https://doi.org/10.1007/s00795-021-00304-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00795-021-00304-7