Abstract
Objective
To compare dental caries, oral hygiene, periodontal status, bruxism, malocclusion, tooth loss, and salivary alterations between autistic and typical developing individuals.
Material and methods
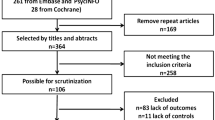
Observational studies presenting clinical measures of oral outcomes between autism spectrum disorder (ASD) individuals and controls. EMBASE, LILACS, PubMed, PsycINFO, Scopus, Web of Science, Google Scholar, and ProQuest were searched up to June 26, 2023. Pairs of reviewers independently conducted study selection, data extraction, and assessments of methodological quality and certainty of evidence. Meta-analyses of standardized mean differences (SMD) and risk ratio (RR) were performed.
Results
A total of 47 studies comprising 6885 autistic individuals were included in the review. Autistic individuals had significantly higher severity of dental-caries experience in primary teeth (SMD 0.29, 95%CI 0.02, 0.56), of dental plaque presence (SMD 0.59, 95%CI 0.24, 0.94), and of gingivitis (SMD 0.45, 95%CI 0.02, 0.88). Autistic individuals showed higher probability of occurrence of gingivitis (RR 1.34, 95%CI 1.08, 1.66,), bruxism (RR 4.23, 95%CI 2.32, 7.74), overjet (RR 2.16, 95%CI 1.28, 3.64), overbite (RR 1.62, 95%CI 1.02, 2.59), crossbite (RR 1.48, 95%CI 1.02, 2.13), and openbite (RR 2.37, 95%CI 1.46, 3.85), when compared to neurotypical individuals. Most estimates showed a small effect size with very low certainty of evidence.
Conclusion
Autistic individuals show worse oral health status than controls.
Clinical relevance
The findings reported herein can help to build health policies to better serve autistic individuals including prevention actions and access to specialized dental care.




Similar content being viewed by others
References
APA, American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders. Washington, DC
WHO, World Health Organization (2022) Autism. https://www.who.int/news-room/factsheets/detail/autism-spectrum-disorders/. Accessed 3 December 2022
Zeidan J, Fombonne E, Scorah J, Ibrahim A, Shih A (2022) Global prevalence of autism: a systematic review update. Autism Res 15:778–790. https://doi.org/10.1002/aur.2696
Al-Sehaibany FS, Aljubour AA (2018) Characteristics of primary dentition occlusion among preschool children with autism spectrum disorder. J Dent Heal Oral Disord Ther 9:262–266. https://doi.org/10.15406/jdhodt.2018.09.00388
AlMusawi MA, Al-Dabagh DJ (2019) Characteristics of malocclusion in Iraqi children with autism spectrum disorder. Indian J Forensic Med Toxicol. https://doi.org/10.5958/0973-9130.2019.00411.0
Onol S, Kirzioǧlu Z (2018) Evaluation of oral health status and influential factors in children with autism. Niger J Clin Pract 21:429–435. https://doi.org/10.4103/njcp.njcp_41_17
Orellana LM, Silvestre FJ, Martínez-Sanchis S, Martínez-Mihi V, Bautista D (2012) Oral manifestations in a group of adults with autism spectrum disorder. Med Oral Patol Oral Cir Bucal 17:415–419. https://doi.org/10.4317/medoral.17573
Daneshvar SH, Kavianfar A, Masoomi SH, Daneshvar MM (2020) Comparison of oral health status and behaviors between children with autistic spectrum disorder and healthy children in Rasht city, Iran. Cumhur Dent J 23:38–44. https://doi.org/10.7126/cumudj.638071
El Khatib AA, El Tekeya MM, El Tantawi MA, Omar T (2014) Oral health status and behaviours of children with autism spectrum disorder: a case-control study. Int J Paediatr Dent 24:314–323. https://doi.org/10.1111/ipd.12067
Blomqvist M, Bejerot S, Dahllöf G (2015) A cross-sectional study on oral health and dental care in intellectually able adults with autism spectrum disorder. BMC Oral Health 15:1–8. https://doi.org/10.1186/s12903-015-0065-z
Diab HM, Motlaq SS, Alsharare A et al (2016) Comparison of gingival health and salivary parameters among autistic and non-autistic school children in Riyadh. J Clin Diagnostic Res 10:110–113. https://doi.org/10.7860/JCDR/2016/23373.8692
Fontaine-Sylvestre C, Roy A, Rizkallah J, Dabbagh B, Ferraz dos Santos B (2017) Prevalence of malocclusion in Canadian children with autism spectrum disorder. Am J Orthod Dentofac Orthop 152:38–41. https://doi.org/10.1016/j.ajodo.2017.02.014
Al-Maweri S, Halboub E, Al-Soneidar W, Al-Sufyani G (2014) Oral lesions and dental status of autistic children in Yemen: a case-control study. J Int Soc Prev Community Dent 4:S199–S203. https://doi.org/10.4103/2231-0762.149040
Bhandary S, Hari N (2017) Salivary biomarker levels and oral health status of children with autistic spectrum disorders: a comparative study. Eur Arch Paediatr Dent 18:91–96. https://doi.org/10.1007/s40368-017-0275-y
Vajawat M, Deepika PC (2012) Comparative evaluation of oral hygiene practices and oral health status in autistic and normal individuals. J Int Soc Prev Community Dent. https://doi.org/10.4103/2231-0762.109369
Jaber MA (2011) Dental caries experience, oral health status and treatment needs of dental patients with autism. J Appl Oral Sci 19:212–217. https://doi.org/10.1590/S1678-77572011000300006
Leiva-García B, Planells E, Planells del Pozo P, Molina-López J (2019) Association between feeding problems and oral health status in children with autism spectrum disorder. J Autism Dev Disord. https://doi.org/10.1007/s10803-019-04211-w
Suhaib F, Saeed A, Gul H, Kaleem M (2019) Oral assessment of children with autism spectrum disorder in Rawalpindi, Pakistan. Autism 23:81–86. https://doi.org/10.1177/1362361317730299
Namal N, Vehit HE, Koksal S (2007) Do autistic children have higher levels of caries? A cross-sectional study in Turkish children. J Indian Soc Pedod Prev Dent 25:97–102. https://doi.org/10.4103/0970-4388.33457
Cermak SA, Curtin C, Bandini LG (2010) Food selectivity and sensory sensitivity in children with autism spectrum disorders. J Am Diet Assoc 110:238–246. https://doi.org/10.1016/j.jada.2009.10.032
Spencer D, Marshall J, Post B et al (2013) Psychotropic medication use and polypharmacy in children with autism spectrum disorders. Pediatrics 132:833–840. https://doi.org/10.1542/peds.2012-3774
Wolff A, Joshi RK, Ekström J et al (2017) A guide to medications inducing salivary gland dysfunction, xerostomia, and subjective sialorrhea: a systematic review sponsored by the World Workshop on Oral Medicine VI. Drugs R D 17:1–28. https://doi.org/10.1007/s40268-016-0153-9
Flink H, Tegelberg Å, Arnetz JE, Birkhed D (2019) Self-reported oral and general health related to xerostomia, hyposalivation, and quality of life among caries active younger adults. Acta Odontol Scand 78:229–235. https://doi.org/10.1080/00016357.2019.1690677
Cunha-Cruz J, Scott JA, Rothen M et al (2013) Salivary characteristics and dental caries: evidence from general dental practices. J Am Dent Assoc 144:e31–e40. https://doi.org/10.14219/jada.archive.2013.0159
Kuter B, Guler N (2019) Caries experience, oral disorders, oral hygiene practices and sociodemographic characteristics of autistic children. Eur J Paediatr Dent 20:237–241. https://doi.org/10.23804/ejpd.2019.20.03.13
Kolawole KA, Folayan MO (2019) Association between malocclusion, caries and oral hygiene in children 6 to 12 years old resident in suburban Nigeria. BMC Oral Health 19:1–9. https://doi.org/10.1186/s12903-019-0959-2
Elmore JL, Bruhn AM, Bobzien JL (2016) Interventions for the reduction of dental anxiety and corresponding behavioral deficits in children with autism spectrum disorder. J Dent Hyg 90:111–120
Thomas N, Blake S, Morris C, Moles DR (2018) Autism and primary care dentistry: parents’ experiences of taking children with autism or working diagnosis of autism for dental examinations. Int J Paediatr Dent 28:226–238. https://doi.org/10.1111/ipd.12345
Bartolomé-Villar B, Mourelle-Martínez MR, Diéguez-Pérez M, de Nova-García MJ (2016) Incidence of oral health in paediatric patients with disabilities: Sensory disorders and autism spectrum disorder. Systematic review II. J Clin Exp Dent. https://doi.org/10.4317/jced.52923
Corridore D, Zumbo G, Corvino I, Guaragna M, Bossù M, Polimeni A (2020) Systematic review prevalence of oral disease and treatment types proposed to children affected by autistic spectrum disorder in pediatric dentistry: a systematic review. Clin Ter 171:275–282. https://doi.org/10.7417/CT.2020.2226
Lam PPY, Du R, Peng S, McGrath CPJ, Yiu CKY (2020) Oral health status of children and adolescents with autism spectrum disorder: a systematic review of case-control studies and meta-analysis. Autism 24:1047–1066. https://doi.org/10.1177/1362361319877337
Valendriyani Ningrum, Abu Bakar, Tzong-Ming Shieh Y-HS (2021) The oral health inequities between special needs children and normal children in Asia: a systematic review and meta-analysis. Healthcare (Basel) 1–12
Granja GL, Lacerda-Santos JT, Firmino RT et al (2022) Occurrence of bruxism in individuals with autism spectrum disorder: a systematic review and meta-analysis. Spec Care Dent 42:476–485. https://doi.org/10.1111/scd.12707
Barros A, Mascarenhas P, Botelho J, Machado V, Balixa G, Lopes LB (2022) Autism spectrum disorders and malocclusions: systematic review and meta-analyses. J Clin Med 11:1–13. https://doi.org/10.3390/jcm11102727
Page MJ, McKenzie JE, Bossuyt PM et al (2021) Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J Clin Epidemiol 134:103–112. https://doi.org/10.1016/j.jclinepi.2021.02.003
Wiebe N, Vandermeer B, Platt RW, Klassen TP, Moher D, Barrowman NJ (2006) A systematic review identifies a lack of standardization in methods for handling missing variance data. J Clin Epidemiol 59:342–353. https://doi.org/10.1016/j.jclinepi.2005.08.017
The Newcastle-Ottawa Scale (NOS) for assess- ing the quality of nonrandomised studies in meta-analyses [word file] (2011) http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 8 November 2021
Moskalewicz A, Oremus M (2020) No clear choice between Newcastle-Ottawa Scale and Appraisal Tool for Cross-Sectional Studies to assess methodological quality in cross-sectional studies of health-related quality of life and breast cancer. J Clin Epidemiol 120:94–103. https://doi.org/10.1016/j.jclinepi.2019.12.013
Lo CKL, Mertz D, Loeb M (2014) Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol 14:1–5. https://doi.org/10.1186/1471-2288-14-45
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page M, Welch VA (2023) Cochrane Handb Syst Rev Interv version 6.4
Global Burden of Disease Collaborative Network (2020) Global burden of disease study (GBD 2019) Socio-Demographic Index (SDI) 1950–2019. Seattle, United States of America: Institute for Health Metrics and Evaluation (IHME)
Santesso N, Glenton C, Dahm P et al (2020) GRADE guidelines 26: informative statements to communicate the findings of systematic reviews of interventions. J Clin Epidemiol 119:126–135. https://doi.org/10.1016/j.jclinepi.2019.10.014
Yuanyuan L, Chen H, Ph D (2017) How big is a big hazard ratio?
Higgins JPT, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:1–9. https://doi.org/10.1136/bmj.d5928
Ryan R, Hill S (2016) How to GRADE the quality of the evidence. http://cccrg.cochrane.org/author-resources. Accessed 31 August 2022
Fahlvik-Planefeldt C, Herrstrom P (2011) Dental care of autistic children within the non-specialized Public Dental Service. Swed Dent J 25:113–118
Loo CY, Graham RM, Hughes CV (2008) The caries experience and behavior of dental patients with autism spectrum disorder. J Am Dent Assoc 139:1518–1524. https://doi.org/10.14219/jada.archive.2008.0078
Tsai SJ, Hsu JW, Huang KL, Bai YM, Su TP, Chen TJ, Chen MH (2023) Autism spectrum disorder and periodontitis risk: a cohort study of 38,203 adolescents. J Am Dent Assoc 154:479–485. https://doi.org/10.1016/j.adaj.2023.02.020
Du RY, Yiu CKY, King NM, Wong VCN, McGrath CPJ (2015) Oral health among preschool children with autism spectrum disorders: a case-control study. Autism 19:746–751. https://doi.org/10.1177/1362361314553439
Hasell S, Hussain A, Da Silva K (2022) The oral health status and treatment needs of pediatric patients living with autism spectrum disorder: a retrospective study. Dent J (Basel) 10:224. https://doi.org/10.3390/dj10120224
Qiao Y, Wu M, Feng Y, Zhou Z, Chen L, Chen F (2018) Alterations of oral microbiota distinguish children with autism spectrum disorders from healthy controls. Sci Rep 8:1597. https://doi.org/10.1038/s41598-018-19982-y
Bassoukou IH, Nicolau J, Santos MT (2009) Saliva flow rate, buffer capacity, and pH of autistic individuals. Clin Oral Investig 13:23–27. https://doi.org/10.1007/s00784-008-0209-5
Klein U (1999) Characteristics of patients with autistic disorder (AD) presenting for dental treatment: a survey and chart review. Spec Care Dent. https://doi.org/10.1111/j.1754-4505.1999.tb01386.x
Stein LI, Polido JC, Cermak SA (2013) Oral care and sensory over-responsivity in children with autism spectrum disorders. Pediatr Dent 35:230–235
Rai K, Hegde AM, Jose N (2012) Salivary antioxidants and oral health in children with autism. Arch Oral Biol 57:1116–1120. https://doi.org/10.1016/j.archoralbio.2012.03.006
Karande S (2006) Autism: a review for family physicians. Indian J Med Sci 60:205–215. https://doi.org/10.4103/0019-5359.25683
Al-Sehaibany FS (2017) Occurrence of oral habits among preschool children with autism spectrum disorder. Pakistan J Med Sci. https://doi.org/10.12669/pjms.335.13554
Medina AC, Sogbe R, Gómez-Rey AM, Mata M (2003) Factitial oral lesions in an autistic paediatric patient. Int J Paediatr Dent 13:130–137. https://doi.org/10.1046/j.1365-263X.2003.00440.x
Warren JJ, Bishara SE, Steinbock KL, Yonezu T, Nowak AJ (2001) Effects of oral habits’ duration on dental characteristics in the primary dentition. J Am Dent Assoc. https://doi.org/10.14219/jada.archive.2001.0121
Sudha P, Bhasin S, Anegundi R (2005) Prevalence of dental caries among 5–13-year-old children of Mangalore city. J Indian Soc Pedod Prev Dent 23:74–79. https://doi.org/10.4103/0970-4388.16446
Acknowledgements
We thank the Brazilian fostering agency Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) for the financial support.
Autistic individuals have worse oral status than neurotypical controls: A systematic review and meta-analysis of observational studies
Funding
This study was funded by the Brazilian fostering agency Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
Author information
Authors and Affiliations
Contributions
Jaine C Uliana: Substantial contributions to the design of the work; the acquisition, analysis, and interpretation of data.
Catiusse C Del’Agnese: Substantial contributions to the acquisition, analysis, and interpretation of data.
Raquel P Antoniazzi: Substantial contributions to the design of the work; the acquisition, analysis, and interpretation of data.
Karla Z Kantorski: Substantial contributions to the conception and design of the study; the acquisition, analysis, and interpretation of data for the work; final approval of the version to be published.
All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Uliana, J.C., Del’ Agnese, C.C., Antoniazzi, R.P. et al. Autistic individuals have worse oral status than neurotypical controls: a systematic review and meta-analysis of observational studies. Clin Oral Invest 28, 137 (2024). https://doi.org/10.1007/s00784-024-05500-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-024-05500-0