Abstract
Introduction
This study investigated the factors of the effectiveness of microimplant-assisted rapid palatal expansion (MARPE) in late adolescents and adults, such as age, midpalatal suture maturation (MPSM) stage, palate length (PL), palatal index (PI), and midpalatal bone thickness (MBT), and at each microimplant position, the palate bone thickness (PBT), the nasal cortical bone thickness (CoTN), the cancellous bone thickness (CaT), and the palate cortical bone thickness (CoTP) were evaluated.
Methods
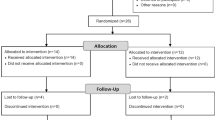
Cone-beam computed tomography (CBCT) images of 50 patients (mean, 23.30 ± 7.03 years; range, 16–51 years) treated with MARPE were evaluated. Maxillary expansion ratio (MER) was used to assess the MARPE effectiveness and grouped patients into low and high MER groups according to the mean of MER. MER was the ratio of maxillary expansion width to MARPE screw expansion measured in CBCT images. The t-test was used to analyze the differences between the low and high MER groups. The Pearson correlation test was performed to investigate the correlation between MER and age, MPSM stage, PL, PI, MBT, PBT, CoTN, CaT, and CoTP.
Results
Age, MPSM stage, and MBT in regions 18 mm and 21 mm behind the incisor foramen correlated negatively with MER (\(r = -0.340\), − 0.390, − 0.386, and − 0.335, respectively, all \(P<0.05\)), whereas PBT and CoTN of anterior microimplant positions correlated positively with MER (\(r = 0.365\) and 0.418, respectively, all \(P<0.01\)). No correlation was observed between other variables and MER.
Conclusions
MARPE effectiveness decreased as age and midpalatal suture maturation stage increased, respectively. Thinner midpalatal suture bone in regions 18 mm and 21 mm behind the incisor foramen, thicker palate bone, and nasal cortical bone of anterior microimplant positions were related to more effective MARPE.
Clinical relevance
In patients with older chronological age and later MPSM stages, MARPE effectiveness might be unsatisfactory. Clinicians should carefully evaluate the palate bone thickness before MARPE treatment.










Similar content being viewed by others
Data availability
The data are not publicly available due to privacy or ethical restrictions.
References
Annarumma F, Posadino M, De Mari A, Drago S, Aghazada H, Gravina GM, Qorri E, Silvestrini-Biavati A, Migliorati M (2021) Skeletal and dental changes after maxillary expansion with a bone-borne appliance in young and late adolescent patients. Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists, its Constit Soc Am Board Orthodontics 159:e363–e375. https://doi.org/10.1016/j.ajodo.2020.11.031
McMullen C, Al Turkestani NN, Ruellas ACO, Massaro C, Rego M, Yatabe MS, Kim-Berman H, McNamara JA Jr, Angelieri F, Franchi L, Ngan P, He H, Cevidanes LHS (2022) Three-dimensional evaluation of skeletal and dental effects of treatment with maxillary skeletal expansion. Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists, Its Constit Soc Am Board Orthodontics 161:666–678. https://doi.org/10.1016/j.ajodo.2020.12.026
Jia H, Zhuang L, Zhang N, Bian Y, Li S (2022) Age-dependent effects of transverse maxillary deficiency treated by microimplant-assisted rapid palatal expansion: a prospective cone-beam computed tomography study. Amer J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists, Its Constituent Soc Am Board Orthodontics 161:557–573. https://doi.org/10.1016/j.ajodo.2020.10.029
Solano Mendoza P, Aceytuno Poch P, Solano Reina E, Solano Mendoza B (2022) Skeletal, dentoalveolar and dental changes after “mini-screw assisted rapid palatal expansion” evaluated with cone beam computed tomography. J Clin Med 11(16):4652. https://doi.org/10.3390/jcm11164652
Bi WG, Li K (2022) Effectiveness of miniscrew-assisted rapid maxillary expansion: a systematic review and meta-analysis. Clin Oral Invest 26:4509–4523. https://doi.org/10.1007/s00784-022-04415-y
Shin H, Hwang CJ, Lee KJ, Choi YJ, Han SS, Yu HS (2019) Predictors of midpalatal suture expansion by miniscrew-assisted rapid palatal expansion in young adults: a preliminary study. Korean journal of orthodontics 49:360–371. https://doi.org/10.4041/kjod.2019.49.6.360
Jeon JY, Choi SH, Chung CJ, Lee KJ (2022) The success and effectiveness of miniscrew-assisted rapid palatal expansion are age- and sex-dependent. Clin Oral Invest 26:2993–3003. https://doi.org/10.1007/s00784-021-04281-0
Oliveira CB, Ayub P, Angelieri F, Murata WH, Suzuki SS, Ravelli DB, Santos-Pinto A (2021) Evaluation of factors related to the success of miniscrew-assisted rapid palatal expansion. Angle Orthod 91:187–194. https://doi.org/10.2319/051420-436.1
Persson M, Thilander B (1977) Palatal suture closure in man from 15 to 35 years of age. Am J Orthod 72:42–52. https://doi.org/10.1016/0002-9416(77)90123-3
Knaup B, Yildizhan F, Wehrbein H (2004) Age-related changes in the midpalatal suture. A histomorphometric study. Journal of orofacial orthopedics = Fortschritte der Kieferorthopadie : Organ/official. J Deutsche Gesellschaft fur Kieferorthopadie 65:467–74. https://doi.org/10.1007/s00056-004-0415-y
Naya-Imai H, Uchida Y, Inaba M, Namura Y, Osada A, Charleston-Coad T, Nakamura Y, Motoyoshi M (2022) Age dependence of the maturation of the midpalatal suture in the stability of orthodontic anchoring screws. Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists, Its Constit Soc Am Board Orthodontics 161:809–819. https://doi.org/10.1016/j.ajodo.2021.01.032
Angelieri F, Cevidanes LH, Franchi L, Gonçalves JR, Benavides E, McNamara JA Jr (2013) Midpalatal suture maturation: classification method for individual assessment before rapid maxillary expansion. Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists Constit Soc Am Board Orthodontics 144:759–769. https://doi.org/10.1016/j.ajodo.2013.04.022
Jesus AS, Oliveira CB, Murata WH, Suzuki SS, Santos-Pinto AD (2021) Would midpalatal suture characteristics help to predict the success rate of miniscrew-assisted rapid palatal expansion? Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists Constituent Soc Am Board Orthodontics 160:363–373. https://doi.org/10.1016/j.ajodo.2020.04.035
Matsuyama Y, Motoyoshi M, Tsurumachi N, Shimizu N (2015) Effects of palate depth, modified arm shape, and anchor screw on rapid maxillary expansion: a finite element analysis. Eur J Orthod 37:188–193. https://doi.org/10.1093/ejo/cju033
Lyu X, Guo J, Chen L, Gao Y, Liu L, Pu L, Lai W, Long H (2020) Assessment of available sites for palatal orthodontic mini-implants through cone-beam computed tomography. Angle Orthod 90:516–523. https://doi.org/10.2319/070719-457.1
Ichinohe M, Motoyoshi M, Inaba M, Uchida Y, Kaneko M, Matsuike R, Shimizu N (2019) Risk factors for failure of orthodontic mini-screws placed in the median palate. J Oral Sci 61:13–18. https://doi.org/10.2334/josnusd.17-0377
Winsauer H, Walter A, Scherfler M, Ploder O (2017) What are the limits of microimplant-assisted palatal expanders? Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists Constit Soc Am Board Orthodontics 151:3–4. https://doi.org/10.1016/j.ajodo.2016.09.011
Brunetto DP, Sant’Anna EF, Machado AW, Moon W (2017) Non-surgical treatment of transverse deficiency in adults using Microimplant-assisted Rapid Palatal Expansion (MARPE). Dental press journal of orthodontics 22:110–125. https://doi.org/10.1590/2177-6709.22.1.110-125.sar
Lee RJ, Moon W, Hong C (2017) Effects of monocortical and bicortical mini-implant anchorage on bone-borne palatal expansion using finite element analysis. Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists Constit Soc Am Board Orthodontics 151:887–897. https://doi.org/10.1016/j.ajodo.2016.10.025
Paredes N, Colak O, Sfogliano L, Elkenawy I, Fijany L, Fraser A, Zhang B, Moon W (2020) Differential assessment of skeletal, alveolar, and dental components induced by microimplant-supported midfacial skeletal expander (MSE), utilizing novel angular measurements from the fulcrum. Prog Orthod 21:18. https://doi.org/10.1186/s40510-020-00320-w
Cantarella D, Dominguez-Mompell R, Moschik C, Mallya SM, Pan HC, Alkahtani MR, Elkenawy I, Moon W (2018) Midfacial changes in the coronal plane induced by microimplant-supported skeletal expander, studied with cone-beam computed tomography images. Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists Constit Soc Am Board Orthodontics 154:337–345. https://doi.org/10.1016/j.ajodo.2017.11.033
Ok G, Sen Yilmaz B, Aksoy DO, Kucukkeles N (2021) Maturity evaluation of orthodontically important anatomic structures with computed tomography. Eur J Orthod 43:8–14. https://doi.org/10.1093/ejo/cjaa009
Cho AR, Park JH, Moon W, Chae JM, Kang KH (2022) Short-term effects of microimplant-assisted rapid palatal expansion on the circummaxillary sutures in skeletally mature patients: a cone-beam computed tomography study. Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists Constituent Soc Am Board Orthodontics 161:e187–e197. https://doi.org/10.1016/j.ajodo.2021.01.023
Miyawaki S, Koyama I, Inoue M, Mishima K, Sugahara T, Takano-Yamamoto T (2003) Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists Constituent Soc Am Board Orthodontics 124:373–378. https://doi.org/10.1016/s0889-5406(03)00565-1
Salmoria I, de Souza EC, Furtado A, Franzini CM, Custodio W (2022) Dentoskeletal changes and their correlations after micro-implant-assisted palatal expansion (MARPE) in adults with advanced midpalatal suture ossification. Clin Oral Invest 26:3021–3031. https://doi.org/10.1007/s00784-021-04284-x
MacGinnis M, Chu H, Youssef G, Wu KW, Machado AW, Moon W (2014) The effects of micro-implant assisted rapid palatal expansion (MARPE) on the nasomaxillary complex–a finite element method (FEM) analysis. Prog Orthod 15:52. https://doi.org/10.1186/s40510-014-0052-y
Li N, Sun W, Li Q, Dong W, Martin D, Guo J (2020) Skeletal effects of monocortical and bicortical mini-implant anchorage on maxillary expansion using cone-beam computed tomography in young adults. Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists Constituent Soc Am Board Orthodontics 157:651–661. https://doi.org/10.1016/j.ajodo.2019.05.021
Fernandes LC, FarinazzoVitral RW, Noritomi PY, Maximiano GS, da Silva J, Campos M (2021) Influence of the hyrax expander screw position on displacement and stress distribution in teeth: a study with finite elements. Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists Constit Soc Am Board Orthodontics 160:266–275. https://doi.org/10.1016/j.ajodo.2020.04.031
Fernandes LC, FarinazzoVitral RW, Noritomi PY, Schmitberger CA, da Silva J, Campos M (2019) Influence of the hyrax expander screw position on stress distribution in the maxilla: a study with finite elements. Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists Constit Soc Am Board Orthodontics 155:80–87. https://doi.org/10.1016/j.ajodo.2018.03.019
Cantarella D, Savio G, Grigolato L, Zanata P, Berveglieri C, Lo Giudice A, Isola G, Del Fabbro M, Moon W (2020) A new methodology for the digital planning of micro-implant-supported maxillary skeletal expansion. Medical devices (Auckland, NZ) 13:93–106. https://doi.org/10.2147/mder.S247751
Pulver RJ, Campbell PM, Opperman LA, Buschang PH (2016) Miniscrew-assisted slow expansion of mature rabbit sutures. Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists Constituent Soc Am Board Orthodontics 150:303–312. https://doi.org/10.1016/j.ajodo.2015.12.026
Suzuki SS, Braga LFS, Fujii DN, Moon W, Suzuki H (2018) Corticopuncture facilitated microimplant-assisted rapid palatal expansion. Case Reports Dentistry 2018:1392895. https://doi.org/10.1155/2018/1392895
Chen W, Zhang K, Liu D (2021) Palatal bone thickness at the implantation area of maxillary skeletal expander in adult patients with skeletal Class III malocclusion: a cone-beam computed tomography study. BMC Oral Health 21:144. https://doi.org/10.1186/s12903-021-01489-0
Motoyoshi M, Inaba M, Ono A, Ueno S, Shimizu N (2009) The effect of cortical bone thickness on the stability of orthodontic mini-implants and on the stress distribution in surrounding bone. Int J Oral Maxillofac Surg 38:13–18. https://doi.org/10.1016/j.ijom.2008.09.006
Kang S, Lee SJ, Ahn SJ, Heo MS, Kim TW (2007) Bone thickness of the palate for orthodontic mini-implant anchorage in adults. Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists Constit Soc Am Board Orthodontics 131:S74-81. https://doi.org/10.1016/j.ajodo.2005.09.029
Negrisoli S, Angelieri F, Gonçalves JR, da Silva HDP, Maltagliati L, RaphaelliNahás-Scocate AC (2022) Assessment of the bone thickness of the palate on cone-beam computed tomography for placement of miniscrew-assisted rapid palatal expansion appliances. Am J Orthodontics Dentofacial Orthopedics : Official Public Am Ass Orthodontists Constit Soc Am Board Orthodontics 161:849–857. https://doi.org/10.1016/j.ajodo.2021.01.037
Nucera R, Ciancio E, Maino G, Barbera S, Imbesi E, Bellocchio AM (2022) Evaluation of bone depth, cortical bone, and mucosa thickness of palatal posterior supra-alveolar insertion site for miniscrew placement. Prog Orthod 23:18. https://doi.org/10.1186/s40510-022-00412-9
Cantarella D, Karanxha L, Zanata P, Moschik C, Torres A, Savio G, Del Fabbro M, Moon W (2021) Digital planning and manufacturing of maxillary skeletal expander for patients with thin palatal bone. Medical devices (Auckland, NZ) 14:299–311. https://doi.org/10.2147/mder.S331127
Funding
This study was funded by the National Natural Science Foundation of China (81970964 to Jie Guo).
Author information
Authors and Affiliations
Contributions
Xiuping Nie: study conception and design, material preparation, data collection and analysis, writing—original draft. Xin Zhang: writing—review and editing. Jie Guo and Jian Yu: guidance throughout the study and manuscript editing. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Research Ethics Committee of Shandong University Dental School (Protocol No. 20210821).
Consent to participate
Informed consent was not required for this retrospective study. All data were de-identified to ensure confidentiality.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiuping Nie and Xin Zhang contributed equally to this work and should be considered the co-first authors.
Jian Yu and Jie Guo contributed equally to this work and should be considered the co-corresponding authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nie, X., Zhang, X., Liu, Y. et al. Evaluation of palate-related factors of the effectiveness of microimplant-assisted rapid palatal expansion in late adolescents and adults. Clin Oral Invest 27, 3531–3544 (2023). https://doi.org/10.1007/s00784-023-04967-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-04967-7