Abstract
Objective
This study aimed to explore the quantitative and qualitative condylar changes following stabilization splint (S.S) therapy, including condylar position, morphology, and bone mineral density (BMD) in subjects with temporomandibular disorders (TMD).
Materials and methods
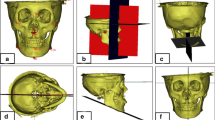
In this retrospective clinical study, we enrolled 40 TMD subjects (80 joints) aged 18 to 35 years, for whom a S.S was used to treat TMD. The 80 TMD consists of 32 masticatory muscle disorders (myalgia) and 48 TMJ disorders (arthralgia). Cone beam computed tomography (CBCT) was used to scan the TMJs of subjects pre- and post-treatment for three-dimensional analysis (3D). Using Mimics software v.21.0, quantitative (3D condylar and joint spaces dimensions parameters were measured using linear measurements in millimeters, according to the Kamelchuk method and Ikeda method, while the assessment of anteroposterior condyle position within the glenoid fossa was based on the method of Pullinger and Hollender), and qualitative (a round bone tissue with an area of 2 mm2 in three representative areas according to the Kamelchuk method to measure condylar BMD) pre- and post-treatment. Intra- and inter-group statistical comparisons were performed using the Wilcoxon signed ranks and the Kruskal–Wallis test, respectively.
Results
The course of treatment was 6–12 months, with an average of 9.1 months. For the pre- and post-treatment quantitative comparisons, there was a statistically significant difference in the anterior joint space (AJS) and coronal medial space, as well as the condyle length in the myalgia group and condylar width in the arthralgia group. For qualitative measurements, a significant difference was observed in the posterior slope of the myalgia group and the arthralgia group’s anterior, superior, and posterior slopes. The inter-group comparisons revealed significant differences in AJS, condylar length, and anterior slope density.
Conclusion
In short-term follow-up, the S.S influenced patients with TMD from different origins; it changes anterior and coronal medial joint space, condyle length in myalgia, and width in arthralgia. Furthermore, it improved the condyle bone density more evidently in arthralgia.
Clinical relevance
This study highlights the influence of S.S on symptomatic populations with TMD of different origins from a qualitative and quantitative perspective.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- TMD:
-
Temporomandibular joint disorders
- BMD:
-
Bone mineral density
- S.S:
-
Stabilization splints
- CBCT:
-
Cone beam computed tomography
- 3D:
-
Three dimensions
- MCD:
-
Measures Condyle Displacement device
- MIC:
-
Maximum intercuspation
- MRI:
-
Magnetic resonance imaging
- HU:
-
Hounsfield unit
- AS:
-
Anterior slope
- SS:
-
Superior slope
- PS:
-
Posterior slope
References
Al-koshab M, Nambiar P, John J (2015) Assessment of condyle and glenoid fossa morphology using CBCT in South-East Asians. PLoS One 10(3):e0121682
De Leeuw R, Klasser GD (2018) Orofacial pain: guidelines for assessment, diagnosis, and management. Quintessence Publishing Company, Incorporated Hanover Park, IL, US
Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet J-P et al (2014) Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache 28(1):6–27
Donovan TE, Marzola R, Murphy KR, Cagna DR, Eichmiller F, McKee JR et al (2018) Annual review of selected scientific literature: a report of the Committee on Scientific Investigation of the American Academy of Restorative Dentistry. J Prosthet Dent 120(6):816–878
Pandarakalam C, Khalaf MWBT-RM in BS. (2014) Temporomandibular disorders. Elsevier. https://doi.org/10.1016/B978-0-12-801238-3.00002-7
Kuzmanovic Pficer J, Dodic S, Lazic V, Trajkovic G, Milic N, Milicic B (2017) Occlusal stabilization splint for patients with temporomandibular disorders: meta-analysis of short and long term effects. PLoS One 12(2):e0171296
Gębska M, Dalewski B, Pałka Ł, Kołodziej Ł, Sobolewska E (2022) Chronotype profile, stress, depression level, and temporomandibular symptoms in students with type D personality. J Clin Med 11(7). https://doi.org/10.3390/jcm11071886
Dijkstra PU, Kalk WWI, Roodenburg JLN (2004) Trismus in head and neck oncology: a systematic review. Oral Oncol 40(9):879–889
Park I-Y, Kim J-H, Park Y-H (2015) Three-dimensional cone-beam computed tomography based comparison of condylar position and morphology according to the vertical skeletal pattern. Korean J Orthod 45(2):66–73
Petersson A (2010) What you can and cannot see in TMJ imaging – an overview related to the RDC/TMD diagnostic system. J Oral Rehabil 37(10):771–778
Barghan S, Tetradis S, Mallya S (2012) Application of cone beam computed tomography for assessment of the temporomandibular joints. Aust Dent J 57(Suppl 1):109–118
DaliliKajan Z, Khaki N, Kia SJ, Salamat F (2012) Assessing joint space and condylar position in the people with normal function of temporomandibular joint with cone-beam computed tomography. Dent Res J (Isfahan) 9:607–612
Almashraqi AA (2020) Dimensional and positional associations between the mandibular condyle and glenoid fossa: a three-dimensional cone-beam computed tomography-based study. J Contemp Dent Pract 21(10):1075–1083
Al-Moraissi EA, Farea R, Qasem KA, Al-Wadeai MS, Al-Sabahi ME, Al-Iryani GM (2020) Effectiveness of occlusal splint therapy in the management of temporomandibular disorders: network meta-analysis of randomized controlled trials. Int J Oral Maxillofac Surg 49(8):1042–1056
Okeson JP (2022) Management of temporomandibular disorders and occlusion, 5th edn. Mosby, St. Louis
Al‐Ani MZ, Davies SJ, Gray RJM, Sloan P, Glenny AM (2004) Stabilisation splint therapy for temporomandibular pain dysfunction syndrome. Cochrane Database Syst Rev (1). https://doi.org/10.1002/14651858.CD002778.pub2
Honnef LR, Pauletto P, Conti Réus J, Massignan C, Souza BDM de, Michelotti A et al (2022) Effects of stabilization splints on the signs and symptoms of temporomandibular disorders of muscular origin: A systematic review. Cranio 21:1–12. https://doi.org/10.1080/08869634.2022.2047510
Dalewski B, Kamińska A, Kiczmer P, Węgrzyn K, Pałka Ł, Janda K et al (2021) Pressure algometry evaluation of two occlusal splint designs in bruxism management-randomized, controlled clinical trial. J Clin Med 10(11). https://doi.org/10.3390/jcm10112342.
Ricketts RM (1950) Variations of the temporomandibular joint as revealed by cephalometric laminagraphy. Am J Orthod 36(12):877–898
Wassell RW, Adams N, Kelly PJ (2004) Treatment of temporomandibular disorders by stabilising splints in general dental practice: results after initial treatment. Br Dent J 197(1):35–41
Lee Y-H, Hong IK, An J-S (2019) Anterior joint space narrowing in patients with temporomandibular disorder. J Orofac Orthop = Fortschritte der Kieferorthopadie Organ/official J Dtsch Gesellschaft fur Kieferorthopadie. 80(3):116–127
Drozdzowska B, Pluskiewicz W (2002) Longitudinal changes in mandibular bone mineral density compared with hip bone mineral density and quantitative ultrasound at calcaneus and hand phalanges. Br J Radiol 75(897):743–747
Mühlberger G, Svejda M, Lottersberger C, Emshoff R, Putz R, Kuhn V (2009) Mineralization density and apparent density in mandibular condyle bone. Oral Surgery, Oral Med Oral Pathol Oral Radiol Endodontology 107(4):573–579
Lin H, Zhu P, Lin Y, Wan S, Shu X, Xu Y et al (2013) Mandibular asymmetry: a three-dimensional quantification of bilateral condyles. Head Face Med 9:42
Lee M-Y, Park JH, Kim S-C, Kang K-H, Cho J-H, Cho J-W et al (2016) Bone density effects on the success rate of orthodontic microimplants evaluated with cone-beam computed tomography. Am J Orthod Dentofac Orthop 149(2):217–224
Ganugapanta VR, Ponnada SR, Gaddam KPR, Perumalla K, Khan I, Mohammed NA (2017) Computed tomographic evaluation of condylar symmetry and condyle-fossa relationship of the temporomandibular joint in subjects with normal occlusion and malocclusion: a comparative study. J Clin Diagn Res 11(2):ZC29–ZC33
Yasa Y, Akgül HM (2018) Comparative cone-beam computed tomography evaluation of the osseous morphology of the temporomandibular joint in temporomandibular dysfunction patients and asymptomatic individuals. Oral Radiol 34(1):31–39
Çakur B, Bayrakdar İŞ (2016) No proven correlations between bone quality and degenerative bone changes in the mandibular condyle and articular eminence in temporomandibular joint dysfunction. Oral Radiol 32(1):33–39
Arsan B, Köse TE, Çene E, Özcan İ (2017) Assessment of the trabecular structure of mandibular condyles in patients with temporomandibular disorders using fractal analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 123(3):382–391
Alhammadi MS, Fayed MMS, Labib A (2016) Comprehensive three-dimensional cone beam computed tomography analysis of the temporomandibular joint in different vertical skeletal facial patterns. J World Fed Orthod 5(1):9–17
Alhammadi MS, Shafey AS, Fayed MS, Mostafa YA (2014) Temporomandibular joint measurements in normal occlusion: a three-dimensional cone beam computed tomography analysis. J World Fed Orthod 3(4):155–162
Zonnenberg AJJ, Mulder J (2014) The efficacy of a specific stabilization splint. Cranio 32(1):68–74
Martins A, Aquino L, MELOTO C, Barbosa C (2016) Counseling and oral splint for conservative treatment of temporomandibular dysfunction: preliminary study. Rev Odontol da UNESP 45. https://doi.org/10.1590/1807-2577.28515
Barão VAR, Gallo AKG, Zuim PRJ, Garcia AR, Assunção WG (2011) Effect of occlusal splint treatment on the temperature of different muscles in patients with TMD. J Prosthodont Res 55(1):19–23
Kamelchuk LS, Grace MGA, Major PW (1996) Post-imaging temporomandibular joint space analysis. CRANIO® 14(1):23–29
Ikeda K, Kawamura A (2009) Assessment of optimal condylar position with limited cone-beam computed tomography. Am J Orthod Dentofac Orthop 135(4):495–501
Pullinger AG, Hollender L, Solberg WK, Petersson A (1985) A tomographic study of mandibular condyle position in an asymptomatic population. J Prosthet Dent 53(5):706–713
Hilgers ML, Scarfe WC, Scheetz JP, Farman AG (2005) Accuracy of linear temporomandibular joint measurements with cone beam computed tomography and digital cephalometric radiography. Am J Orthod Dentofac Orthop 128(6):803–811
Van Dessel J, Nicolielo LFP, Huang Y, Coudyzer W, Salmon B, Lambrichts I et al (2017) Accuracy and reliability of different cone beam computed tomography (CBCT) devices for structural analysis of alveolar bone in comparison with multislice CT and micro-CT. Eur J Oral Implantol 10(1):95–105
Hasegawa Y, Kakimoto N, Tomita S, Honda K, Tanaka Y, Yagi K et al (2011) Movement of the mandibular condyle and articular disc on placement of an occlusal splint. Oral Surg, Oral Med Oral Pathol Oral Radiol Endodontology 112(5):640–647
Ramachandran A, Jose R, Tunkiwala A, Varma RB, Shanmugham AM, Nair PK et al (2021) Effect of deprogramming splint and occlusal equilibration on condylar position of TMD patients - a CBCT assessment. Cranio 39(4):294–302
Coelho Filho D, dos Santos LAN, Júnior ASR, Magri LV, Mazzetto MO (2016) Influence of the interocclusal splint in condylar position of patients with tmd: computed cone beam. Brazilian Dent Sci 19(3):32–38
Dawson PE (2007) Functional Occlusion From TMJ to Smile. Des St Louis, MO Elsevier Mosby, pp 380–382
Kim K-J, Park JH, Bay RC, Lee M-Y, Chang N-Y, Chae J-M (2018) Mandibular condyle bone density in adolescents with varying skeletal patterns evaluated using cone-beam computed tomography: a potential predictive tool. Am J Orthod Dentofac Orthop 154(3):382–389
Campos MJ da S, de Souza TS, Mota Júnior SL, Fraga MR, Vitral RWF (2014) Bone mineral density in cone beam computed tomography: only a few shades of gray. World J Radiol 6(8):607–612
Reeves TE, Mah P, McDavid WD (2012) Deriving Hounsfield units using grey levels in cone beam CT: a clinical application. Dentomaxillofac Radiol 41(6):500–508
Cassetta M, Stefanelli LV, Pacifici A, Pacifici L, Barbato E (2014) How accurate is CBCT in measuring bone density? A comparative CBCT-CT in vitro study. Clin Implant Dent Relat Res 16(4):471–478
Wen L, Yan W, Yue Z, Bo D, Xiao Y, Chun-Ling W (2015) Study of condylar asymmetry in angle class III malocclusion with mandibular deviation. J Craniofac Surg 26(3):e264–e268
Kawaguchi H, Matsumoto T, Kurokawa T, Orimo H, Mizunashi K, Takuwa Y (1990) Measurement of serum BGP levels by two site immunoradiometric assay (IRMA) using monoclonal antibodies. Horumon To Rinsho Clin Endocrinol 38:1291–1296
Ok S-M, Jeong S-H, Ahn Y-W, Kim Y-I (2016) Effect of stabilization splint therapy on glenoid fossa remodeling in temporomandibular joint osteoarthritis. J Prosthodont Res 60(4):301–307
Ok S-M, Lee J, Kim Y-I, Lee J-Y, Kim KB, Jeong S-H (2014) Anterior condylar remodeling observed in stabilization splint therapy for temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol 118(3):363–370
Derwich M, Pawlowska E (2022) Do the mandibular condyles change their positions within glenoid fossae after occlusal splint therapy combined with physiotherapy in patients diagnosed with temporomandibular joint disorders? A prospective case control study. J Pers Med 12(2). https://doi.org/10.3390/jpm12020254
Acknowledgements
We wish to thank the New Medical Treatment and New Technology of the First Affiliated Hospital of Xi’an Jiaotong University, Shaanxi University Joint Project, for financially supporting this study; Charles S Greene, Professor, University of Illinois College of Dentistry, USA, for his insightful comments in reviewing the manuscript; and Mohammed Elhoumed, Salma Izeldin, and Nahawand Adil, Xi’an Jiaotong University, China, for their statistical assistance.
Funding
This study was funded by the New Medical Treatment and New Technology of the First Affiliated Hospital of Xi’an Jiaotong University (XJYFY-2017ZD02), Shaanxi University Joint Project (2020GXLH-Y-014).
Author information
Authors and Affiliations
Contributions
Mazen Musa and Qianqian Zhang: conception of the study, definition of the methodology, drafting of the manuscript, and analysis and interpretation of data for the work; Riham Awad and Wenfang Wang: contributions to the conception and design of the work and interpretation of data for the work, statistical analysis, and interpretation of the data and clinical examination; Madiha Mohammed Saleh Ahmed and Yunshan Zhao: substantial contributions to the acquisition of data sample recruiting and data collection; Abeer A. Almashraqi: grammatical, typo, and intellectual editing of the manuscript and contributed to critical revision of the article; Xi Chen: supervision and funding acquisition; Maged S. Alhammadi: contributions to the conception and critical revision of the article and contributed to the scope of the discussion. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This retrospective clinical study was approved by the ethics committee of Xi’an Jiaotong University, Xi’an Jiaotong University, China (No. XJTU1AF2022LSK-027).
Informed consent
For research involving human participants, informed consent was obtained from all subjects. All methods were performed following the relevant guidelines and regulations.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mazen Musa and Qianqian Zhang contributed equally to this work, and they are considered as joint first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Musa, M., Zhang, Q., Awad, R. et al. Quantitative and qualitative condylar changes following stabilization splint therapy in patients with temporomandibular joint disorders. Clin Oral Invest 27, 2299–2310 (2023). https://doi.org/10.1007/s00784-023-04963-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-04963-x