Abstract
Objectives
The aim of this study was to investigate the mechanical, chemical, optical, and adhesive properties of BisGMA-free experimental resin composites containing Exothane-24—an elastomeric urethane monomer—and different co-initiators.
Materials and methods
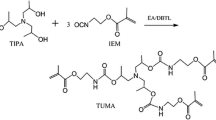
A blend of urethane dimethacrylate (UDMA), extended dimethacrylate urethane (PEG 400), triethylene glycol dimethacrylate (TEGDMA), and camphorquinone was prepared. Two different co-initiators—dimethyl aminoethyl methacrylate (DMAEMA) or 4-N alcohol, N-dimethylamine phenylethyl (DMPOH)—were added to the blend. Exothane-24 monomer was added to the blend for each co-initiator and four groups were established as follows: DMAEMA; DMAEMA + Exothane; DMPOH; and DMPOH + Exothane. Specimens were photo-activated using a multi-wave LED light-curing unit (VALO; 954 mW/cm2 of irradiance). Mechanical (ultimate tensile strength, flexural strength, flexural modulus and hardness), chemical (degree of conversion, hardness reduction, water sorption and solubility), optical (color change), and adhesive (microtensile bond strength) properties were analyzed. Data were submitted to two-way ANOVA and Tukey’s test (α = 0.05).
Results
The resin composite containing DMPOH and Exothane-24 showed similar or superior performance to those of the other experimental composites for mechanical and chemical properties, except for flexural strength. It also showed less color change and greater micro-tensile bond strength.
Conclusions
Among the combinations tested, the BisGMA-free resin composite containing Exothane-24 combined with the DMPOH co-initiator showed the best mechanical, chemical, optical, and adhesive properties.
Clinical relevance
Exothane-24 monomer and DMPOH co-initiator could be useful in the formulation of BisGMA-free resin composites in order to minimize exposure to BPA.

Similar content being viewed by others
References
Van Dijken JW, V, Lindberg A, (2015) A 15-year randomized controlled study of a reduced shrinkage stress resin composite. Dent Mater 31:1150–1158. https://doi.org/10.1016/j.dental.2015.06.012
Jang J-H, Park S-H, Hwang I-N (2015) Polymerization shrinkage and depth of cure of bulk-fill resin composites and highly filled flowable resin. Oper Dent 40:172–180. https://doi.org/10.2341/13-307-L
Moorthy A, Hogg CH, Dowling AH, Grufferty BF, Benetti AR, Fleming GJP (2012) Cuspal deflection and microleakage in premolar teeth restored with bulk-fill flowable resin-based composite base materials. J Dent 40:500–505. https://doi.org/10.1016/j.jdent.2012.02.015
Ferracane JL (2011) Resin composite - state of the art. Dent Mater 27:29–38. https://doi.org/10.1016/j.dental.2010.10.020
Floyd CJE, Dickens SH (2006) Network structure of Bis-GMA- and UDMA-based resin systems. Dent Mater 22:1143–1149. https://doi.org/10.1016/j.dental.2005.10.009
Moszner N, Fischer UK, Angermann J, Rheinberger V (2008) A partially aromatic urethane dimethacrylate as a new substitute for Bis-GMA in restorative composites. Dent Mater 24:694–699. https://doi.org/10.1016/j.dental.2007.07.001
Leprince JG, Palin WM, Vanacker J, Sabbagh J, Devaux J, Leloup G (2014) Physico-mechanical characteristics of commercially available bulk-fill composites. J Dent 42:993–1000. https://doi.org/10.1016/j.jdent.2014.05.009
Ferracane JL (2006) Hygroscopic and hydrolytic effects in dental polymer networks. Dent Mater 22:211–222. https://doi.org/10.1016/j.dental.2005.05.005
Van Landuyt KL, Snauwaert J, De Munck J, Peumans M, Yoshida Y, Poitevin A, Coutinho E, Suzuki K, Lambrechts P, Van Meerbeek B (2007) Systematic review of the chemical composition of contemporary dental adhesives. Biomaterials 28:3757–3785. https://doi.org/10.1016/j.biomaterials.2007.04.044
Münchow EA, De BGD, Alves S, Valente LL, Cava S, Piva E, Ogliari FA (2014) Effect of elastomeric monomers as polymeric matrix of experimental adhesive systems : degree of conversion and bond strength characterization. Appl Adhes Sci 2:3. https://doi.org/10.1186/2196-4351-2-3
Fugolin AP, de Paula AB, Dobson A, Huynh V, Consani R, Ferracane JL, Pfeifer CS (2020) Alternative monomer for BisGMA-free resin composites formulations. Dent Mater 36:884–892. https://doi.org/10.1016/j.dental.2020.04.009
Becher R, Wellendorf H, Sakhi AK, Samuelsen JT, Thomsen C, Bølling AK, Kopperud HM (2018) Presence and leaching of bisphenol a (BPA) from dental materials. Acta Biomater Odontol Scand 4:56–62. https://doi.org/10.1080/23337931.2018.1476869
Kingman A, Hyman J, Masten SA, Jayaram B, Smith C, Eichmiller F, Arnold MC, Wong PA, Schaeffer JM, Solanki S, Dunn WJ (2012) Bisphenol A and other compounds in human saliva and urine associated with the placement of composite restorations. J Am Dent Assoc 143:1292–1302. https://doi.org/10.14219/jada.archive.2012.0090
Maserejian NN, Trachtenberg FL, Wheaton OB, Calafat AM, Ranganathan G, Kim H-Y, Houser R (2016) Changes in urinary bisphenol A concentrations associated with placement of dental composite restorations in children and adolescents. J Am Dent Assoc 147:620–630. https://doi.org/10.1016/j.adaj.2016.02.020
vom Saal FS, Nagel SC, Coe BL, Angle BM, Taylor JA (2012) The estrogenic endocrine disrupting chemical bisphenol A (BPA) and obesity. Mol Cell Endocrinol 354:74–84. https://doi.org/10.1016/j.mce.2012.01.001
González-López JA, Pérez-Mondragón AA, Cuevas-Suárez CE, Alonso JC, Trejo-Carbajal N, Herrera-González AN (2019) Hydrophobic composite resins using a novel allylic urethane monomer as additive. J Mex Chem Soc 63:105–114. https://doi.org/10.29356/jmcs.v63i4.877
Taira M, Urabe H, Hirose T, Wakasa K, Yamaki M (1988) Analysis of photo-initiators in visible-light-cured dental composite resins. J Dent Res 67:24–28. https://doi.org/10.1177/00220345880670010401
Ogunyinka A, Palin WM, Shortall AC, Marquis PM (2007) Photoinitiation chemistry affects light transmission and degree of conversion of curing experimental dental resin composites. Dent Mater 23:807–813. https://doi.org/10.1016/j.dental.2006.06.016
Schroeder WF, Vallo CI (2007) Effect of different photoinitiator systems on conversion profiles of a model unfilled light-cured resin. Dent Mater 23:1313–1321. https://doi.org/10.1016/j.dental.2006.11.010
Oliveira DC, Silva CB, Muniz BV, Volpato MC, Costa AR, Sinhoreti MA (2014) Effect of 4-(N, N-dimethylamino)phenethyl alcohol on degree of conversion and cytotoxicity of photo-polymerized CQ-based resin composites. Braz Dent J 25:538–542. https://doi.org/10.1590/0103-6440201300113
De Oliveira DCRS, Ayres APA, Rocha MG, Giannini M, Puppin Rontani RM, Ferracane JL, Sinhoreti MA (2015) Effect of different in vitro aging methods on color stability of a dental resin-based composite using CIELAB and CIEDE2000 color-difference formulas. J Esthet Restor Dent 27:322–330. https://doi.org/10.1111/jerd.12155
De Oliveira DCRS, Rocha MG, Gatti A, Correr AB, Ferracane JL, Sinhoret MAC (2015) Effect of different photoinitiators and reducing agents on cure efficiency and color stability of resin-based composites using different LED wavelengths. J Dent 43:1565–1572. https://doi.org/10.1016/j.jdent.2015.08.015
Favarão J, Oliveira D, Zanini MM, Rocha MG, Correr-Sobrinho L, Sinhoreti M (2021) Effect of curing-light attenuation on color stability and physical and chemical properties of resin cements containing different photoinitiators. J Mech Behav Biomed Mater 113:104110. https://doi.org/10.1016/j.jmbbm.2020.104110
Schneider LF, Moraes RR, Cavalcante LM, Sinhoreti MA, Correr-Sobrinho L, Consani S (2008) Cross-link density evaluation through softening tests: effect of ethanol concentration. Dent Mater 24:199–203. https://doi.org/10.1016/j.dental.2007.03.010
Silame FDJ, Geraldeli GP, Sinhoreti MAC, Pires-de-Souza FCP, Roulet JF, Geraldeli S (2017) Dentin µTBS and hardness of bulk-fill and conventional composites placed in a box-shaped cavity preparation. J Adhes Dent 19:395–400. https://doi.org/10.3290/j.jad.a39276
Yu B, Liu F, He J (2014) Preparation of low shrinkage methacrylate-based resin system without Bisphenol A structure by using a synthesized dendritic macromer (G-IEMA). J Mech Behav Biomed Mater 35:1–8. https://doi.org/10.1016/j.jmbbm.2014.03.012
Yin M, Liu F, He J (2016) Preparation and characterization of Bis-GMA free dental resin system with synthesized dimethacrylate monomer TDDMMA derived from tricyclo[5.2.1.0(2,6)]-decanedimethanol. J Mech Behav Biomed Mater 57:157–163. https://doi.org/10.1016/j.jmbbm.2015.11.020
Yap AU, Eweis AH, Yahya NA (2018) Dynamic and static flexural appraisal of resin-based composites: comparison of the ISO and mini-flexural tests. Oper Dent 43:E223–E231. https://doi.org/10.2341/17-224-L
Nayif MM, Nakajima M, Foxton RM, Tagami J (2008) Bond strength and ultimate tensile strength of resin composite filled into dentine cavity; effect of bulk and incremental filling technique. J Dent 36:228–234. https://doi.org/10.1016/j.jdent.2007.12.006
Feitosa VP, Fugolin AP, Correr AB, Correr-Sobrinho L, Consani S, Watson TF, Sinhoreti MA, Sauro S (2012) Effects of different photo-polymerization protocols on resin-dentine μTBS, mechanical properties and cross-link density of a nano-filled resin composite. J Dent 40:802–809. https://doi.org/10.1016/j.jdent.2012.05.014
Delgado AJ, Castellanos EM, Sinhoreti M, Oliveira DC, Abdulhameed N, Geraldeli S, Sulaiman TA, Roulet JF (2019) The use of different photoinitiator systems in photopolymerizing resin cements through ceramic veneers. Oper Dent 44:396–404. https://doi.org/10.2341/17-263-L
Borges BC, Souza-Júnior EJ, Catelan A, Paulillo LA, Aguiar FH (2012) Can extended photoactivation time of resin-based fissure sealer materials improve ultimate tensile strength and decrease water sorption/solubility? Eur J Dent 6:402–407
Yin M, Guo S, Liu F, He J (2015) Synthesis of fluorinated dimethacrylate monomer and its application in preparing Bis-GMA free dental resin. J Mech Behav Biomed Mater 51:337–344. https://doi.org/10.1016/j.jmbbm.2015.07.025
Van Landuyt KL, Nawrot T, Geebelen B, De Munck J, Snauwaert J, Yoshihara K, Scheers H, Godderis L, Hoet P, Van Meerbeek B (2011) How much do resin-based dental materials release? A meta-analytical approach. Dent Mater 27:723–747. https://doi.org/10.1016/j.dental.2011.05.001
Herrera-Gonzalez AN, Caldera-Villalobos M, Perez-Mondragon AA, Cuevas-Suarez CE, Gonzalez-Lopez JA (2019) Analysis of double bond conversion of photopolymerizable monomers by FTIR-ATR spectroscopy. J Chem Educ 96:1786–1789. https://doi.org/10.1021/acs.jchemed.8b00659
Podgórski M (2010) Synthesis and characterization of novel dimethacrylates of different chain lengths as possible dental resins. Dent Mater 26:188–194. https://doi.org/10.1016/j.dental.2010.02.011
Cornelio RB, Wikant A, Mjøsund H, Molvig H, Haasum J, Gedde UW, Ortengren UT (2014) The influence of bis-EMA vs bis GMA on the degree of conversion and water susceptibility of experimental composite materials. Acta Odontol Scand 72:440–447. https://doi.org/10.3109/00016357.2013.856467
Duff J, Barclift T, Newman S, Stansbury J, Lewis S, Abuelenain D (2012) Novel resins for dental composite and sealants. J Dent Res 91 (Spec Iss A): abstract #837
Guarda MB, Di Nizo PT, Abuna GF, Catelan A, Sinhoreti MAC, Vitti RP (2020) Effect of electric current-assisted application of adhesives on their bond strength and quality. J Adhes Dent 22:393–398. https://doi.org/10.3290/j.jad.a44870
Sano H, Chowdhury AFMA, Saikaew P, Matsumoto M, Hoshika S, Yamauti M (2020) The microtensile bond strength test: its historical background and application to bond testing. Jpn Dent Sci Rev 56:24–31. https://doi.org/10.1016/j.jdsr.2019.10.001
Ersen KA, Gürbüz Ö, Özcan M (2020) Evaluation of polymerization shrinkage of bulk-fill resin composites using microcomputed tomography. Clin Oral Invest 24:1687–1693. https://doi.org/10.1007/s00784-019-03025-5
Ye S, Azarnoush S, Smith IR, Cramer NB, Stansbury JW, Bowman CN (2012) Using hyperbranched oligomer functionalized glass fillers to reduce shrinkage stress. Dent Mater 28:1004–1011. https://doi.org/10.1016/j.dental.2012.05.003
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
This manuscript does not contain any studies with human participants or animals performed by any of the authors. All procedures performed involving human wastes were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Approval was obtained from the ethics committee of Piracicaba Dental School, University of Campinas, Brazil (#55806016.6.5418). The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to participate
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Oliveira, R.F., Abuna, G.F., Roulet, JF. et al. Effect of an elastomeric urethane monomer on BisGMA-free resin composites containing different co-initiators. Clin Oral Invest 26, 957–967 (2022). https://doi.org/10.1007/s00784-021-04078-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-04078-1