Abstract
Objective
The aim of the present study was to evaluate the in vitro biocompatibility of Theracal PT, Theracal LC, and MTA Angelus, considered as bioactive materials used for vital pulp treatment, on human dental pulp stem cells (hDPSCs).
Materials and methods
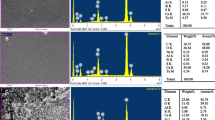
Human dental pulp stem cells (hDPSCs) were isolated from third molars, and material eluates were prepared (undiluted, 1:2, and 1:4 ratios). The hDPSC cytotoxicity, adhesion, morphology, viability, and cell migration were assessed. The mineralization nodule formation was determined by Alizarin red S staining (ARS). The odonto/osteogenic differentiation potential was assessed by osteo/odontogenic marker expression real-time qPCR. The chemical composition and ion release of the vital pulp materials were determined by energy dispersive X-ray (EDX) and inductively coupled plasma-mass spectrometry (ICP-MS), respectively. Statistical differences were assessed by ANOVA and Tukey’s test (p < 0.05).
Results
The three vital pulp materials showed variable levels of calcium, tungsten, silicon, and zirconium release and in their chemical composition. Cytocompatibility assays revealed higher hDPSC viability and migration rates when treated with Theracal PT than with Theracal LC. The lowest cell adhesion and spreading were observed in all Theracal LC-treated groups, whereas the highest were observed when treated with MTA. Theracal PT and MTA promoted the upregulation of DSPP and RUNX2 gene expression (p < 0.05). After 21 days, both MTA Angelus and Theracal PT–treated cells exhibited a significantly higher mineralized nodule formation than the negative control (p < 0.05).
Conclusions
This study demonstrates the favorable in vitro cytocompatibility and bioactive properties of the recently introduced Theracal PT and the well-established MTA Angelus on hDPSCs, as opposed to Theracal LC. More studies, including in vivo animal testing are suggested before these new formulations might be used in the clinical setting.
Clinical relevance
Theracal PT is a new material that could be clinically suitable for vital pulp therapy. Further studies considering its biocompatibility and bioactivity are necessary.









Similar content being viewed by others
References
da Rosa WLO, Piva E, da Silva AF (2018) Disclosing the physiology of pulp tissue for vital pulp therapy. Int Endod J 51:829–846. https://doi.org/10.1111/iej.12906
Tran XV, Gorin C, Willig C, Baroukh B, Pellat B, Decup F, Opsahl Vital S, Chaussain C, Boukpessi T (2012) Effect of a calcium-silicate-based restorative cement on pulp repair. J Dent Res 91:1166–1171. https://doi.org/10.1177/0022034512460833
Hanna SN, Perez Alfayate R, Prichard J (2020) Vital pulp therapy an insight over the available literature and future expectations. Eur Endod J 5:46–53. https://doi.org/10.14744/eej.2019.44154
Meschi N, Patel B, Ruparel NB (2020) Material pulp cells and tissue interactions. J Endod 46:S150–S160. https://doi.org/10.1016/j.joen.2020.06.031
Parirokh M, Torabinejad M, Dummer PMH (2018) Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview - part I: vital pulp therapy. Int Endod J 51:177–205. https://doi.org/10.1111/iej.12841
Rosa V, Zhang Z, Grande RH, Nor JE (2013) Dental pulp tissue engineering in full-length human root canals. J Dent Res 92:970–975. https://doi.org/10.1177/0022034513505772
Tatullo M, Codispoti B, Sied J, Makeeva I, Paduano F, Marrelli M, Spagnuolo G (2019) Stem cells-based and molecular-based approaches in regenerative dentistry: a topical review. Curr Stem Cell Res Ther 14:607–616. https://doi.org/10.2174/1574888X14666190626111154
Youssef AR, Emara R, Taher MM, Al-Allaf FA, Almalki M, Almasri MA, Siddiqui SS (2019) Effects of mineral trioxide aggregate, calcium hydroxide, biodentine and Emdogain on osteogenesis, Odontogenesis, angiogenesis and cell viability of dental pulp stem cells. BMC Oral Health 19:133. https://doi.org/10.1186/s12903-019-0827-0
Zaen El-Din AM, Hamama HH, Abo El-Elaa MA, Grawish ME, Mahmoud SH, Neelakantan P (2020) The effect of four materials on direct pulp capping: an animal study. Aust Endod J 46:249–256. https://doi.org/10.1111/aej.12400
Dahake PT, Panpaliya NP, Kale YJ, Dadpe MV, Kendre SB, Bogar C (2020) Response of stem cells from human exfoliated deciduous teeth (SHED) to three bioinductive materials - an in vitro experimental study. Saudi Dent J 32:43–51. https://doi.org/10.1016/j.sdentj.2019.05.005
Pelepenko LE, Saavedra F, Antunes TBM, Bombarda GF, Gomes B, Zaia AA, Camilleri J, Marciano MA (2020) Physicochemical, antimicrobial, and biological properties of White-MTAFlow. Clin Oral Investig 25:663–672. https://doi.org/10.1007/s00784-020-03543-7
Sauro S, Babbar A, Gharibi B, Feitosa VP, Carvalho RM, Azevedo Rodrigues LK, Banerjee A, Watson T (2018) Cellular differentiation, bioactive and mechanical properties of experimental light-curing pulp protection materials. Dent Mater 34:868–878. https://doi.org/10.1016/j.dental.2018.02.008
Wongwatanasanti N, Jantarat J, Sritanaudomchai H, Hargreaves KM (2018) Effect of bioceramic materials on proliferation and odontoblast differentiation of human stem cells from the Apical Papilla. J Endod 44:1270–1275. https://doi.org/10.1016/j.joen.2018.03.014
Kunert M, Lukomska-Szymanska M (2020) Bio-inductive materials in direct and indirect pulp capping-a review article. Materials (Basel) 13. https://doi.org/10.3390/ma13051204
Jeanneau C, Laurent P, Rombouts C, Giraud T, About I (2017) Light-cured tricalcium silicate toxicity to the dental pulp. J Endod 43:2074–2080. https://doi.org/10.1016/j.joen.2017.07.010
Peters OA (2013) Research that matters - biocompatibility and cytotoxicity screening. Int Endod J 46:195–197. https://doi.org/10.1111/iej.12047
Peters OA, Galicia J, Arias A, Tolar M, Ng E, Shin SJ (2015) Effects of two calcium silicate cements on cell viability, angiogenic growth factor release, and related gene expression in stem cells from the apical papilla. Int Endod J 49:1132–1140. https://doi.org/10.1111/iej.12571
ISO 10993-12 (2012) Biological evaluation of medical devices—Part 12: sample preparation and reference materials. Geneva, Switzerland
Collado-Gonzalez M, Garcia-Bernal D, Onate-Sanchez RE, Ortolani-Seltenerich PS, Alvarez-Muro T, Lozano A, Forner L, Llena C, Moraleda JM, Rodriguez-Lozano FJ (2017) Cytotoxicity and bioactivity of various pulpotomy materials on stem cells from human exfoliated primary teeth. Int Endod J 50:e19–e30. https://doi.org/10.1111/iej.12751
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop D, Horwitz E (2006) Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 8:315–317. https://doi.org/10.1080/14653240600855905
Rodriguez-Lozano FJ, Collado-Gonzalez M, Tomas-Catala CJ, Garcia-Bernal D, Lopez S, Onate-Sanchez RE, Moraleda JM, Murcia L (2019) GuttaFlow Bioseal promotes spontaneous differentiation of human periodontal ligament stem cells into cementoblast-like cells. Dent Mater 35:114–124. https://doi.org/10.1016/j.dental.2018.11.003
Sequeira DB, Seabra CM, Palma PJ, Cardoso AL, Peca J, Santos JM (2018) Effects of a new bioceramic material on human apical papilla cells. J Funct Biomater 9. https://doi.org/10.3390/jfb9040074
Pedano MS, Li X, Li S, Sun Z, Cokic SM, Putzeys E, Yoshihara K, Yoshida Y, Chen Z, Van Landuyt K, Van Meerbeek B (2018) Freshly-mixed and setting calcium-silicate cements stimulate human dental pulp cells. Dent Mater 34:797–808. https://doi.org/10.1016/j.dental.2018.02.005
Pedano MS, Li X, Yoshihara K, Landuyt KV, Van Meerbeek B (2020) Cytotoxicity and bioactivity of dental pulp-capping agents towards human tooth-pulp cells: a systematic review of in-vitro studies and meta-analysis of randomized and controlled clinical trials. Materials (Basel) 13. https://doi.org/10.3390/ma13122670
Li X, Pedano MS, Li S, Sun Z, Jeanneau C, About I, Hauben E, Chen Z, Van Landuyt K, Van Meerbeek B (2020) Preclinical effectiveness of an experimental tricalcium silicate cement on pulpal repair. Mater Sci Eng C Mater Biol Appl 116:111167. https://doi.org/10.1016/j.msec.2020.111167
Nam OH, Kim JH, Choi SC, Kim Y (2020) Time-dependent response of human deciduous tooth-derived dental pulp cells treated with TheraCal LC: functional analysis of gene interactions compared to MTA. J Clin Med 9. https://doi.org/10.3390/jcm9020531
Tomas-Catala CJ, Collado-Gonzalez M, Garcia-Bernal D, Onate-Sanchez RE, Forner L, Llena C, Lozano A, Moraleda JM, Rodriguez-Lozano FJ (2017) Biocompatibility of new pulp-capping materials NeoMTA Plus, MTA Repair HP, and Biodentine on human dental pulp stem cells. J Endod 44:126–132. https://doi.org/10.1016/j.joen.2017.07.017
Costa BC, Guerreiro-Tanomaru JM, Bosso-Martelo R, Rodrigues EM, Bonetti-Filho I, Tanomaru-Filho M (2018) Ytterbium oxide as radiopacifier of calcium silicate-based cements. Physicochemical and Biological Properties. Braz Dent J 29:452–458. https://doi.org/10.1590/0103-6440201802033
Dong X, Wang X, Xing M, Zhao C, Guo B, Cao J, Chang J (2020) Inhibition of the negative effect of high glucose on osteogenic differentiation of bone marrow stromal cells by silicon ions from calcium silicate bioceramics. Regen Biomater 7:9–17. https://doi.org/10.1093/rb/rbz030
Giraud T, Jeanneau C, Rombouts C, Bakhtiar H, Laurent P, About I (2019) Pulp capping materials modulate the balance between inflammation and regeneration. Dent Mater 35:24–35. https://doi.org/10.1016/j.dental.2018.09.008
Collado-Gonzalez M, Garcia-Bernal D, Onate-Sanchez RE, Ortolani-Seltenerich PS, Alvarez Muro T, Lozano A, Forner L, Llena C, Moraleda JM, Rodriguez-Lozano FJ (2017) Cytotoxicity and bioactivity of various pulpotomy materials on stem cells from human exfoliated primary teeth. Int Endod J 50:e19–e30. https://doi.org/10.1111/iej.12751
Lopez-Garcia S, Myong-Hyun B, Lozano A, Garcia-Bernal D, Forner L, Llena C, Guerrero-Girones J, Murcia L, Rodriguez-Lozano FJ (2020) Cytocompatibility, bioactivity potential, and ion release of three premixed calcium silicate-based sealers. Clin Oral Investig 24:1749–1759. https://doi.org/10.1007/s00784-019-03036-2
Koutroulis A, Kuehne SA, Cooper PR, Camilleri J (2019) The role of calcium ion release on biocompatibility and antimicrobial properties of hydraulic cements. Sci Rep 9:19019. https://doi.org/10.1038/s41598-019-55288-3
Nilsen BW, Jensen E, Ortengren U, Michelsen VB (2017) Analysis of organic components in resin-modified pulp capping materials: critical considerations. Eur J Oral Sci 125:183–194. https://doi.org/10.1111/eos.12347
Atsumi T, Ishihara M, Kadoma Y, Tonosaki K, Fujisawa S (2004) Comparative radical production and cytotoxicity induced by camphorquinone and 9-fluorenone against human pulp fibroblasts. J Oral Rehabil 31:1155–1164. https://doi.org/10.1111/j.1365-2842.2004.01357.x
Engelmann J, Volk J, Leyhausen G, Geurtsen W (2005) ROS formation and glutathione levels in human oral fibroblasts exposed to TEGDMA and camphorquinone. J Biomed Mater Res B Appl Biomater 75:272–276. https://doi.org/10.1002/jbm.b.30360
Bortoluzzi EA, Niu LN, Palani CD, El-Awady AR, Hammond BD, Pei DD, Tian FC, Cutler CW, Pashley DH, Tay FR (2015) Cytotoxicity and osteogenic potential of silicate calcium cements as potential protective materials for pulpal revascularization. Dent Mater 31:1510–1522. https://doi.org/10.1016/j.dental.2015.09.020
Feng G, Zhang J, Feng X, Wu S, Huang D, Hu J, Zhu S, Song D (2016) Runx2 modified dental pulp stem cells (DPSCs) enhance new bone formation during rapid distraction osteogenesis (DO). Differentiation 92:195–203. https://doi.org/10.1016/j.diff.2016.06.001
Siew Ching H, Thirumulu Ponnuraj K, Luddin N, Ab Rahman I, Nik Abdul Ghani NR (2020) Early odontogenic differentiation of dental pulp stem cells treated with nanohydroxyapatite-silica-glass ionomer cement. Polymers (Basel) 12. https://doi.org/10.3390/polym12092125
Rodrigues EM, Cornelio AL, Mestieri LB, Fuentes AS, Salles LP, Rossa-Junior C, Faria G, Guerreiro-Tanomaru JM, Tanomaru-Filho M (2016) Human dental pulp cells response to mineral trioxide aggregate (MTA) and MTA Plus: cytotoxicity and gene expression analysis. Int Endod J 50:780–789. https://doi.org/10.1111/iej.12683
Mello-Moura ACV, Santos AMA, Bonini G, Zardetto C, Moura-Netto C, Wanderley MT (2017) Pulp calcification in traumatized primary teeth - classification, clinical and radiographic aspects. J Clin Pediatr Dent 41:467–471. https://doi.org/10.17796/1053-4628-41.6.9
Bakhtiar H, Nekoofar MH, Aminishakib P, Abedi F, Naghi Moosavi F, Esnaashari E, Azizi A, Esmailian S, Ellini MR, Mesgarzadeh V, Sezavar M, About I (2017) Human pulp responses to partial pulpotomy treatment with TheraCal as compared with biodentine and ProRoot MTA: a clinical trial. J Endod 43:1786–1791. https://doi.org/10.1016/j.joen.2017.06.025
Funding
This work was supported by the Spanish Network of Cell Therapy (TerCel), RETICS subprograms of the I+D+I 2013-2016 Spanish National Plan, project “RD16/0011/0001” funded by the Instituto de Salud Carlos III to JMM and cofunded by the European Regional Development Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
The study protocol was approved by the Clinical Research Ethics Committee of the University of Murcia (procedure number: 2199/2018). Likewise, permission was obtained from the Health Department authorities to use the information contained in the CDHs, previously anonymized by one of the investigators belonging to the medical staff of the Health Department in order to protect patient confidentiality. All the information was processed in abidance with the confidentiality regulations defined under Act 15/1999 referred to personal data protection.
Informed consent
Informed consent was obtained from the parents of all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rodríguez-Lozano, F.J., López-García, S., García-Bernal, D. et al. Cytocompatibility and bioactive properties of the new dual-curing resin-modified calcium silicate-based material for vital pulp therapy. Clin Oral Invest 25, 5009–5024 (2021). https://doi.org/10.1007/s00784-021-03811-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03811-0