Abstract
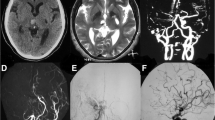
A 40-year-old female with a history of ischemic moyamoya disease treated with indirect revascularization at ages 12 and 25 years presented with a sudden severe headache. Imaging studies revealed focal parenchymal hemorrhage and acute subdural hematoma, confirming a microaneurysm formed on the postoperative transosseous vascular network as the source of bleeding. Conservative management was performed, and no hemorrhage recurred during the 6-month follow-up period. Interestingly, follow-up imaging revealed spontaneous occlusion of the microaneurysm. However, due to the rarity of this presentation, the efficacy of conservative treatment remains unclear. Further research on similar cases is warranted.



Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to conditions of ethical approval but are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Aoyagi M, Fukai N, Yamamoto M, Nakagawa K, Matsushima Y, Yamamoto K (1996) Early development of intimal thickening in superficial temporal arteries in patients with moyamoya disease. Stroke 27(10):1750–1754
Eom KS, Kim DW, Kang SD (2010) Intracerebral hemorrhage caused by rupture of a giant aneurysm complicating superficial temporal artery-middle cerebral artery anastomosis for moyamoya disease. Acta Neurochir (Wien) 152(6):1069–1073
Fukui M, Kono S, Sueishi K, Ikezaki K (2000) Moyamoya disease. Neuropathology 20(SUPPL.):61–64
Ghosh AK (2014) Moyamoya disease presenting with acute subdural hemorrhage. Neurol India 62(2):202–203
Hara S, Mukawa M, Akagawa H, Thamamongood T, Inaji M, Tanaka Y, Maehara T, Kasuya H, Nariai T (2022) Absence of the RNF213 p.R4810K variant may indicate a severe form of pediatric moyamoya disease in Japanese patients. J Neurosurg Pediatr 29:48–56
Hashio A, Hamano E, Ozaki S et al (2024) Pathological changes in the lenticulostriate artery indicate the mechanisms leading to intracranial hemorrhage in moyamoya disease: a case report. Acta Neurochir (Wien). https://doi.org/10.1007/s00701-024-05992-5
Koduri S, Andrew Wilkinson D, Griauzde JM, Gemmete JJ, Maher CO (2019) Development of bilateral dural arteriovenous fistulae following pial synangiosis for moyamoya syndrome: case report. J Neurosurg Pediatr 24(1):9–13
Mauro AJ, Johnson ES, Chikos PM, Alvord EC Jr (1980) Lipohyalinosis and miliary microaneurysms causing cerebral hemorrhage in a patient with moyamoya. A clinicopathological study. Stroke 11:405–412
Mori K, Miyazaki H, Yasunaga A, Tanaka K, Ono H (1979) A case of moyamoya syndrome with subdural and intracerebral hematoma due to different bleeding sources. Acta Med Nagasaki 24:48–54
Myeong HS, Kim K, Lee SH, Yoo DH, Cho YD, Cho WS, Kang HS, Kim JE (2022) Clinical significance of intracranial aneurysms in adult moyamoya disease. World Neurosurg 164:e1034–e1042
Nakakita K, Tanaka S, Fukuda A, Fujii C, Kohama A, Miyasato H (1994) Nontraumatic acute subdural hematoma caused by the rupture of transdural anastomotic vessels in moyamoya disease. Neurol Surg 22(6):561–565
Nishimoto T, Yuki K, Sasaki T, Murakami T, Kodama Y, Kurisu K (2005) A ruptured middle cerebral artery aneurysm originating from the site of anastomosis 20 years after extracranial-intracranial bypass for moyamoya disease: case report. Surg Neurol 64(3):261–265
Umehara T, Goto Y, Kajikawa R, Wakayama A, Kishima H (2018) Life-Threatening hemorrhagic moyamoya disease: report of rare case of atraumatic acute subdural hematoma due to ruptured transdural anastomosis. World Neurosurg 118:16–20
Wiedmann MKH, Davidoff C, Lo PA, Ni W, Rhim JK, Simons M, Stoodley MA (2022) Treatment of ruptured aneurysms of the choroidal collateral system in moyamoya disease: a systematic review and data analysis. J Neurosurg 136(3):637–646
Yamashina M, Inaji M, Hara S, Tanaka Y, Kaneoka A, Nariai T, Maehara T (2023) Encephalo-Duro-pericranio-synangiosis for the treatment of moyamoya disease with posterior cerebral artery lesions. World Neurosurg 175:e678–e685
Ye F, Niu X, Liang F, Dai Y, Liang J, Li J, Wu X, Zheng H, Qi T, Sheng W (2023) RNF213 loss-of-function promotes pathological angiogenesis in moyamoya disease via the Hippo pathway. Brain 146(11):4674–4689
Zhang L, Xu K, Zhang Y, Wang X, Yu J (2015) Treatment strategies for aneurysms associated with moyamoya disease. Int J Med Sci 12(3):234–242
Acknowledgements
We thank a skilled Neuroradiologist in our institution, Dr. Jun Oyama, for retrospectively pointing out the possible formation of microaneurysm.
Author information
Authors and Affiliations
Contributions
Kazuki Kondo contributed to the acquisition and drafting of the article. Shoko Hara contributed to the conception, design, acquisition, and interpretation of data. Azumi Kaneoka contributed to the acquisition and interpretation of the data. Motoki Inaji, Yoji Tanaka and Tadashi Nariai contributed to the interpretation of data. Taketoshi Maehara supervised the study. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval
The observational study of the long-term prognosis of moyamoya disease patients (M2000-1331) and the genetic study (G2016-009) were approved by the Ethics Review Committee of Tokyo Medical and Dental University.
Consent to publish
The patient had consented to the submission of the case report to this journal. The genetic evaluation was performed for the research with ethical approval and with written informed consent of the patient.
Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kondo, K., Hara, S., Kaneoka, A. et al. Spontaneous occlusion of ruptured microaneurysm formed on postoperative transosseous anastomosis after indirect revascularization in a patient with moyamoya disease. Acta Neurochir 166, 206 (2024). https://doi.org/10.1007/s00701-024-06102-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-06102-1