Abstract
Background
Posterior lumbar interbody fusion (PLIF) surgery represents an effective option to treat degenerative conditions in the lumbar spine. To reduce the drawbacks of the classical technique, we developed a variant, so-called Lateral-PLIF, which we then evaluated through a prospective consecutive series of patients.
Methods
All adult patients treated at our institute with single or double level Lateral-PLIF for lumbar degenerative disease from January to December 2017 were prospectively collected. Exclusion criteria were patients < 18 years of age, traumatic patients, active infection, or malignancy, as well as unavailability of clinical and/or radiological follow-up data. The technique consists of insert the cages bilaterally through the transition zone between the central canal and the intervertebral foramen, just above the lateral recess. Pre- and postoperative (2 years) questionnaires and phone interviews (4 years) assessed pain and functional outcomes. Data related to the surgical procedure, postoperative complications, and radiological findings (1 year) were collected.
Results
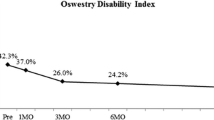
One hundred four patients were selected for the final analysis. The median age was 58 years and primary symptoms were mechanical back pain (100, 96.1%) and/or radicular pain (73, 70.2%). We found a high fusion rate (95%). A statistically significant improvement in functional outcome was also noted (ODI p < 0.001, Roland-Morris score p < 0.001). Walking distance increased from 812 m ± 543 m to 3443 m ± 712 m (p < 0.001). Complications included dural tear (6.7%), infection/wound dehiscence (4.8%), and instrument failure (1.9%) but no neurological deterioration.
Conclusions
Lateral-PLIF is a safe and effective technique for lumbar interbody fusion and may be considered for further comparative study validation with other techniques before extensive use to treat lumbar degenerative disease.







Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and from corresponding authors (F.C.) upon reasonable request.
Abbreviations
- ALIF:
-
Anterior lumbar interbody fusion
- CT:
-
Computed tomography
- ODI:
-
Oswestry Disability Index
- MIS:
-
Minimally invasive technique
- OLIF:
-
Oblique lumbar interbody fusion
- PLIF:
-
Posterior lumbar interbody fusion
- PROCEES:
-
Preferred Reporting of Case Series in Surgery
- RX:
-
Conventional plan radiography
- TLIF:
-
Transforaminal lumbar interbody fusion
- XLIF:
-
Extreme lateral lumbar interbody fusion
- VAS:
-
Visual analogic scale
References
Agha RA, Sohrabi C, Mathew G, Franchi T, Kerwan A, O’Neill N (2020) The PROCESS 2020 guideline: updating consensus Preferred Reporting Of CasESeries in Surgery (PROCESS) guidelines. Int J Surg 84:231–235. https://doi.org/10.1016/j.ijsu.2020.11.005
Aoki Y, Yamagata M, Ikeda Y, Nakajima F, Ohtori S, Nakagawa K, Nakajima A, Toyone T, Orita S, Takahashi K (2012) A prospective randomized controlled study comparing transforaminal lumbar interbody fusion techniques for degenerative spondylolisthesis: unilateral pedicle screw and 1 cage versus bilateral pedicle screws and 2 cages. J Neurosurg Spine 17:153–159. https://doi.org/10.3171/2012.5.Spine111044
Audat Z, Moutasem O, Yousef K, Mohammad B (2012) Comparison of clinical and radiological results of posterolateral fusion, posterior lumbar interbody fusion and transforaminal lumbar interbody fusion techniques in the treatment of degenerative lumbar spine. Singapore Med J 53:183–187
Barrey CY, Boissiere L, D’Acunzi G, Perrin G (2013) One-stage combined lumbo-sacral fusion, by anterior then posterior approach: clinical and radiological results. Eur Spine J 22(Suppl 6):S957-964. https://doi.org/10.1007/s00586-013-3017-9
Barrey C, Darnis A (2015) Current strategies for the restoration of adequate lordosis during lumbar fusion. World J Orthop 6:117–126. https://doi.org/10.5312/wjo.v6.i1.117
Brantigan JW (1994) Pseudarthrosis rate after allograft posterior lumbar interbody fusion with pedicle screw and plate fixation. Spine (Phila Pa 1976) 19:1271–1279. https://doi.org/10.1097/00007632-199405310-00014
Brantigan JW, Steffee AD, Lewis ML, Quinn LM, Persenaire JM (2000) Lumbar interbody fusion using the Brantigan I/F cage for posterior lumbar interbody fusion and the variable pedicle screw placement system: two-year results from a Food and Drug Administration investigational device exemption clinical trial. Spine (Phila Pa 1976) 25:1437–1446. https://doi.org/10.1097/00007632-200006010-00017
Chi KY, Cheng SH, Kuo YK, Lin EY, Kang YN (2021) Safety of lumbar interbody fusion procedures for degenerative disc disease: a systematic review with network meta-analysis of prospective studies. Global Spine J 11:751–760. https://doi.org/10.1177/2192568220938024
Cho JH, Hwang CJ, Lee DH, Lee CS (2021) Clinical and radiological outcomes in patients who underwent posterior lumbar interbody fusion: comparisons between unilateral and bilateral cage insertion. BMC Musculoskelet Disord 22:963. https://doi.org/10.1186/s12891-021-04852-y
Cloward RB (1985) Posterior lumbar interbody fusion updated. Clin Orthopaed Related Res 193:16–19
Cloward RB (1981) Spondylolisthesis: treatment by laminectomy and posterior interbody fusion. Clin Orthopaed Related Res 154:74–82
Cloward RB (1953) The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. I. Indications, operative technique, after care. J Neurosurg 10:154–168. https://doi.org/10.3171/jns.1953.10.2.0154
Cole CD, McCall TD, Schmidt MH, Dailey AT (2009) Comparison of low back fusion techniques: transforaminal lumbar interbody fusion (TLIF) or posterior lumbar interbody fusion (PLIF) approaches. Curr Rev Musculoskelet Med 2:118–126. https://doi.org/10.1007/s12178-009-9053-8
de Kunder SL, van Kuijk SMJ, Rijkers K, Caelers I, van Hemert WLW, de Bie RA, van Santbrink H (2017) Transforaminal lumbar interbody fusion (TLIF) versus posterior lumbar interbody fusion (PLIF) in lumbar spondylolisthesis: a systematic review and meta-analysis. Spine J 17:1712–1721. https://doi.org/10.1016/j.spinee.2017.06.018
Du L, Sun XJ, Zhou TJ, Li YC, Chen C, Zhao CQ, Zhang K, Zhao J (2017) The role of cage height on the flexibility and load sharing of lumbar spine after lumbar interbody fusion with unilateral and bilateral instrumentation: a biomechanical study. BMC Musculoskelet Disord 18:474. https://doi.org/10.1186/s12891-017-1845-1
Fallatah S, Wai E, Baily CS (2013) The value of adding posterior interbody fusion in the surgical treatment of degenerative lumbar spine disorders: a systematic review. Int J Spine Surg 7:e24-28. https://doi.org/10.1016/j.ijsp.2013.01.003
Fraser RD (1995) Interbody, posterior, and combined lumbar fusions. Spine (Phila Pa 1976) 20:167–177. https://doi.org/10.1097/00007632-199512151-00016
Ghobrial GM, Theofanis T, Darden BV, Arnold P, Fehlings MG, Harrop JS (2015) Unintended durotomy in lumbar degenerative spinal surgery: a 10-year systematic review of the literature. Neurosurg Focus 39:E8. https://doi.org/10.3171/2015.7.Focus15266
Ghogawala Z, Dziura J, Butler WE, Dai F, Terrin N, Magge SN, Coumans JV, Harrington JF, Amin-Hanjani S, Schwartz JS, Sonntag VK, Barker FG 2nd, Benzel EC (2016) Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med 374:1424–1434. https://doi.org/10.1056/NEJMoa1508788
Gjessing MH (1951) Osteoplastic anterior fusion of the lower lumbar spine in spondylolisthesis, localized spondylosis, and tuberculous spondylitis. Acta Orthop Scand 20:200–213. https://doi.org/10.3109/17453675108991168
Goldstein CL, Macwan K, Sundararajan K, Rampersaud YR (2016) Perioperative outcomes and adverse events of minimally invasive versus open posterior lumbar fusion: meta-analysis and systematic review. J Neurosurg Spine 24:416–427. https://doi.org/10.3171/2015.2.Spine14973
Hackenberg L, Halm H, Bullmann V, Vieth V, Schneider M, Liljenqvist U (2005) Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to five year results. Eur Spine J 14:551–558. https://doi.org/10.1007/s00586-004-0830-1
Harms J, Rolinger H (1982) A one-stager procedure in operative treatment of spondylolistheses: dorsal traction-reposition and anterior fusion (author’s transl). Z Orthop Ihre Grenzgeb 120:343–347. https://doi.org/10.1055/s-2008-1051624
Hsieh PC, Koski TR, O’Shaughnessy BA, Sugrue P, Salehi S, Ondra S, Liu JC (2007) Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine 7:379–386. https://doi.org/10.3171/spi-07/10/379
Humphreys SC, Hodges SD, Patwardhan AG, Eck JC, Murphy RB, Covington LA (2001) Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine (Phila Pa 1976) 26:567–571. https://doi.org/10.1097/00007632-200103010-00023
Jin-Tao Q, Yu T, Mei W, Xu-Dong T, Tian-Jian Z, Guo-Hua S, Lei C, Yue H, Zi-Tian W, Yue Z (2015) Comparison of MIS vs. open PLIF/TLIF with regard to clinical improvement, fusion rate, and incidence of major complication: a meta-analysis. Eur Spine J 24:1058–1065. https://doi.org/10.1007/s00586-015-3890-5
Katz AD, Mancini N, Karukonda T, Greenwood M, Cote M, Moss IL (2019) Approach-based comparative and predictor analysis of 30-day readmission, reoperation, and morbidity in patients undergoing lumbar interbody fusion using the ACS-NSQIP dataset. Spine (Phila Pa 1976) 44:432–441. https://doi.org/10.1097/brs.0000000000002850
Kepler CK, Rihn JA, Radcliff KE, Patel AA, Anderson DG, Vaccaro AR, Hilibrand AS, Albert TJ (2012) Restoration of lordosis and disk height after single-level transforaminal lumbar interbody fusion. Orthop Surg 4:15–20. https://doi.org/10.1111/j.1757-7861.2011.00165.x
Kunze B, Drasseck T, Kluba T (2011) Posterior and transforaminal lumbar interbody fusion (PLIF/TLIF) for the treatment of localised segment degeneration of lumbar spine. Z Orthop Unfall 149:312–316. https://doi.org/10.1055/s-0030-1250689
Kuslich SD, Ulstrom CL, Griffith SL, Ahern JW, Dowdle JD (1998) The Bagby and Kuslich method of lumbar interbody fusion. History, techniques, and 2-year follow-up results of a United States prospective, multicenter trial. Spine (Phila Pa 1976) 23:1267–1278. https://doi.org/10.1097/00007632-199806010-00019
Lan T, Hu SY, Zhang YT, Zheng YC, Zhang R, Shen Z, Yang XJ (2018) Comparison between posterior lumbar interbody fusion and transforaminal lumbar interbody fusion for the treatment of lumbar degenerative diseases: a systematic review and meta-analysis. World Neurosurg 112:86–93. https://doi.org/10.1016/j.wneu.2018.01.021
Launay O, Perrin G, Barrey C (2016) Instrumented PLIF in lumbar degenerative spine: principles, indications, technical aspects, results, complications and pitfalls. In. pp 407–420. https://doi.org/10.1007/978-3-662-47756-4_31
Liu X, Wang Y, Qiu G, Weng X, Yu B (2014) A systematic review with meta-analysis of posterior interbody fusion versus posterolateral fusion in lumbar spondylolisthesis. Eur Spine J 23:43–56. https://doi.org/10.1007/s00586-013-2880-8
Martin CT, Niu S, Whicker E, Ward L, Yoon ST (2020) Radiographic factors affecting lordosis correction after transforaminal lumbar interbody fusion with unilateral facetectomy. Int J Spine Surg 14:681–686. https://doi.org/10.14444/7099
Mehta VA, McGirt MJ, Garcés Ambrossi GL, Parker SL, Sciubba DM, Bydon A, Wolinsky JP, Gokaslan ZL, Witham TF (2011) Trans-foraminal versus posterior lumbar interbody fusion: comparison of surgical morbidity. Neurol Res 33:38–42. https://doi.org/10.1179/016164110x12681290831289
Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ (2015) Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 1:2–18. https://doi.org/10.3978/j.issn.2414-469X.2015.10.05
Nakai S, Yoshizawa H, Kobayashi S (1999) Long-term follow-up study of posterior lumbar interbody fusion. J Spinal Disord 12:293–299
Ohrt-Nissen S, Carreon LY, Andresen AK, Andersen M, Udby P (2022) Clinical and patient-reported outcomes after posterior versus transforaminal lumbar interbody fusion-a propensity score-matched cohort study on 422 patients with 2-year follow-up. Spine(Phila Pa 1976) 47:180–185. https://doi.org/10.1097/brs.0000000000004215
Park MS, Ju YS, Moon SH, Kim TH, Oh JK, Lim JK, Kim CH, Chung CK, Chang HG (2019) Repeat decompression and fusions following posterolateral fusion versus posterior/transforaminal lumbar interbody fusion for lumbar spondylosis: a national database study. Sci Rep 9:4926. https://doi.org/10.1038/s41598-019-41366-z
Phan K, Thayaparan GK, Mobbs RJ (2015) Anterior lumbar interbody fusion versus transforaminal lumbar interbody fusion—systematic review and meta-analysis. Br J Neurosurg 29:705–711. https://doi.org/10.3109/02688697.2015.1036838
Postacchini F (1999) Surgical management of lumbar spinal stenosis. Spine (Phila Pa 1976) 24:1043–1047. https://doi.org/10.1097/00007632-199905150-00020
Reid PC, Morr S, Kaiser MG (2019) State of the union: a review of lumbar fusion indications and techniques for degenerative spine disease. J Neurosurg Spine 31:1–14. https://doi.org/10.3171/2019.4.Spine18915
Resnick DK, Choudhri TF, Dailey AT, Groff MW, Khoo L, Matz PG, Mummaneni P, Watters WC 3rd, Wang J, Walters BC, Hadley MN (2005) Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 7: intractable low-back pain without stenosis or spondylolisthesis. J Neurosurg Spine 2:670–672. https://doi.org/10.3171/spi.2005.2.6.0670
Rosenberg WS, Mummaneni PV (2001) Transforaminal lumbar interbody fusion: technique, complications, and early results. Neurosurgery 48:569–574. https://doi.org/10.1097/00006123-200103000-00022
Rothrock RJ, McNeill IT, Yaeger K, Oermann EK, Cho SK, Caridi JM (2018) Lumbar lordosis correction with interbody fusion: systematic literature review and analysis. World Neurosurg 118:21–31. https://doi.org/10.1016/j.wneu.2018.06.216
Said E, Abdel-Wanis ME, Ameen M, Sayed AA, Mosallam KH, Ahmed AM, Tammam H (2022) Posterolateral fusion versus posterior lumbar interbody fusion: a systematic review and meta-analysis of randomized controlled trials. Global Spine J 12:990–1002. https://doi.org/10.1177/21925682211016426
Sakaura H, Yamashita T, Miwa T, Ohzono K, Ohwada T (2013) Outcomes of 2-level posterior lumbar interbody fusion for 2-level degenerative lumbar spondylolisthesis. J Neurosurg Spine 19:90–94. https://doi.org/10.3171/2013.4.Spine12651
Salehi SA, Tawk R, Ganju A, LaMarca F, Liu JC, Ondra SL (2004) Transforaminal lumbar interbody fusion: surgical technique and results in 24 patients. Neurosurgery 54:368–374. https://doi.org/10.1227/01.neu.0000103493.25162.18
Schnee CL, Freese A, Ansell LV (1997) Outcome analysis for adults with spondylolisthesis treated with posterolateral fusion and transpedicular screw fixation. J Neurosurg 86:56–63. https://doi.org/10.3171/jns.1997.86.1.0056
Schwab F, Blondel B, Chay E, Demakakos J, Lenke L, Tropiano P, Ames C, Smith JS, Shaffrey CI, Glassman S, Farcy JP, Lafage V (2014) The comprehensive anatomical spinal osteotomy classification. Neurosurgery 74:112–120. https://doi.org/10.1227/NEU.0000000000000182o
Seo DK, Kim MJ, Roh SW, Jeon SR (2017) Morphological analysis of interbody fusion following posterior lumbar interbody fusion with cages using computed tomography. Medicine (Baltimore) 96:e7816. https://doi.org/10.1097/md.0000000000007816
Sim HB, Murovic JA, Cho BY, Lim TJ, Park J (2010) Biomechanical comparison of single-level posterior versus transforaminal lumbar interbody fusions with bilateral pedicle screw fixation: segmental stability and the effects on adjacent motion segments. J Neurosurg Spine 12:700–708. https://doi.org/10.3171/2009.12.Spine09123
Stonecipher T, Wright S (1989) Posterior lumbar interbody fusion with facet-screw fixation. Spine (Phila Pa 1976) 14:468–471. https://doi.org/10.1097/00007632-198904000-00026
Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG (1997) Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine (Phila Pa 1976) 22:210–219. https://doi.org/10.1097/00007632-199701150-00016
Tye EY, Alentado VJ, Mroz TE, Orr RD, Steinmetz MP (2016) Comparison of clinical and radiographic outcomes in patients receiving single-level transforaminal lumbar interbody fusion with removal of unilateral or bilateral facet joints. Spine (Phila Pa 1976) 41:E1039-e1045. https://doi.org/10.1097/brs.0000000000001535
Wang H, Chen W, Jiang J, Lu F, Ma X, Xia X (2016) Analysis of the correlative factors in the selection of interbody fusion cage height in transforaminal lumbar interbody fusion. BMC Musculoskelet Disord 17:9. https://doi.org/10.1186/s12891-016-0866-5
Wimmer C, Krismer M, Gluch H, Ogon M, Stöckl B (1999) Autogenic versus allogenic bone grafts in anterior lumbar interbody fusion. Clin Orthop Relat Res:122–126. https://doi.org/10.1097/00003086-199903000-00015
Xiao YX, Chen QX, Li FC (2009) Unilateral transforaminal lumbar interbody fusion: a review of the technique, indications and graft materials. J Int Med Res 37:908–917. https://doi.org/10.1177/147323000903700337
Xu H, Tang H, Guan X, Jiang F, Xu N, Ju W, Zhu X, Zhang X, Zhang Q, Li M (2013) Biomechanical comparison of posterior lumbar interbody fusion and transforaminal lumbar interbody fusion by finite element analysis. Neurosurgery 72:21–26. https://doi.org/10.1227/NEU.0b013e3182742a69
Zhang BF, Ge CY, Zheng BL, Hao DJ (2016) Transforaminal lumbar interbody fusion versus posterolateral fusion in degenerative lumbar spondylosis: a meta-analysis. Medicine (Baltimore) 95:e4995. https://doi.org/10.1097/md.0000000000004995
Author information
Authors and Affiliations
Contributions
Conceptualization: C.B.; methodology: C.B. and G.C.; investigation: F.C. and I.Z.; data curation: G.C., F.C., A.V., I.Z.; formal analysis: G.C., A.V., R.C.; writing original draft preparation, G.C., and C.B.; writing—review and editing, G.C., F.C., and C.B.; visualization, D.T. and D.C.; supervision: C.B.; project administration, C.B.; all authors have read and agreed to the submitted version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Ethics committee approval has been provided (N°21–312).
Informed consent
The authors state that all the patients gave their informed consent.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Capo, G., Calvanese, F., Vandenbulcke, A. et al. Lateral-PLIF for spinal arthrodesis: concept, technique, results, complications, and outcomes. Acta Neurochir 166, 123 (2024). https://doi.org/10.1007/s00701-024-06024-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-06024-y