Abstract
Background
Several meta-analyses comparing the outcome of awake versus asleep deep brain stimulation procedures could not reveal significant differences concerning the postoperative improvement of motor symptoms. Only rarely information on the procedural details is provided for awake operations and how often somnolence and disorientation occurred, which might hamper the reliability of intraoperative clinical testing. The aim of our study was to investigate possible influencing factors on the occurrence of somnolence and disorientation in awake DBS procedures.
Methods
We retrospectively analyzed 122 patients with Parkinson's disease having received implantation of a DBS system at our centre. Correlation analyses were performed for the duration of disease prior to surgery, number of microelectrode trajectories, AC-PC-coordinates of the planned target, UPDRS-scores, intraoperative application of sedative drugs, duration of the surgical procedure, perioperative application of apomorphine, and the preoperative L-DOPA equivalence dosage with the occurrence of intraoperative somnolence and disorientation.
Results
Patients with intraoperative somnolence were significantly older (p=0.039). Increased duration of the DBS procedure (p=0.020), delayed start of the surgery (p=0.049), higher number of MER trajectories (p=0.041), and the patients’ % UPDRS improvement (p=0.046) also correlated with the incidence of intraoperative somnolence. We identified the main contributing factor to intraoperative somnolence as the use of sedative drugs applied during skin incision and burr hole trepanation (p=0.019). Perioperatively applied apomorphine could reduce the occurrence of somnolent phases during the operation (p=0.026).
Conclusion
Several influencing factors were found to seemingly increase the risk of intraoperative somnolence and disorientation, while the use of sedative drugs seems to be the main contributing factor. We argue that awake DBS procedures should omit the use of sedatives for best clinical outcome. When reporting on awake DBS surgery these factors should be considered and adjusted for, to permit reliable interpretation and comparison of DBS study results.
Similar content being viewed by others
Introduction
In the beginning of the era of deep brain stimulation (DBS) in Parkinson´s disease (PD) most procedures were performed with the patient awake for intra-operative clinical testing [26] [12] [1]. The purpose of clinical testing is to identify the optimal stimulation site, defined by the best reduction of major motor symptoms, while avoiding any side effects. However, the necessity of operations with the patient awake has been challenged early on [2] and an increasing number of implantations nowadays is performed under general anesthesia, guided by anatomical targeting alone or in combination with microelectrode (MER) recordings. Publications concerning the usefulness of intra-operative clinical testing show heterogeneous results [33][6][14][20][13] [8]. In fact, a prospective, randomized clinical trial [19] and several meta-analyses did not reveal significant differences concerning the improvement of motor symptoms when comparing the outcome of awake versus asleep DBS procedures [22][9][18, 27, 37]. Although, a wide range of anesthesiological approaches and perioperative managements have been described for “awake procedures” [28, 29, 36][24], they are rarely reported in detail when comparing awake versus asleep approaches. During awake procedures, intraoperative drowsiness, somnolence and disorientation might occur with an incidence of 1–33% [4, 11, 15, 25, 31]. This potentially hampers the reliability of the determination of the optimal stimulation site and diminishes the advantages of intraoperative clinical testing compared to operations under general anesthesia.
The aim of our retrospective study is to investigate which factors influence the occurrence of somnolence and disorientation during the awake operation. We provide information that will help to improve the reliability and usefulness of awake procedures in the future.
Materials and methods
A total of 122 patients with PD who underwent bilateral subthalamic nucleus-targeted deep brain stimulation (STN-DBS) between 2002 and 2020 were analyzed in this retrospective, observational study. Patient age ranged from 42 to 75 years (mean: 61.8 years). The mean interval between the first diagnosis of PD and DBS surgery was 11.3 years (range: 2–25 years). 57 patients presented with equivalent type, 48 with hypokinetic-rigid type and 17 with tremor-dominant type of PD. Two patients with intracerebral hemorrhages, documented on postoperative CT scans, were not included in this study.
A multidisciplinary team of trained neurologists, neurosurgeons and psychiatrists evaluated the diagnosis of PD and eligibility to receive DBS based on several preoperative tests. Patients with severe brain atrophy, psychiatric disorders and other serious conditions were excluded. All data was acquired during our standard preoperative examinations for DBS surgery. No additional image acquisition or patient testing was conducted. The study was approved by the local ethics committee at the University Medical Center and conducted in accordance with the Declaration of Helsinki.
L-DOPA withdrawal prior to the operation
From 2002 to 2008, all patients (n=41) were put on L-DOPA monotherapy several days prior to the operation. In the afternoon before surgery, all PD related medication was withdrawn until completion of the operation. From 2008 to 2020 (81 patients), PD medication were replaced by L-DOPA monotherapy 10 days prior to DBS surgery, but on admittance the oral L-DOPA medication was substituted by continuous subcutaneous apomorphine treatment. The apomorphine pump was stopped 1h prior to surgery and continued immediately after completion of the operation.
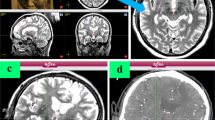
Timing of the pre-operative MRI scan
The first 11 patients received their preoperative stereotactic MRI scan on the day of surgery under general anesthesia with a ceramic head-ring and fiducials attached. In all later patients (n =111) MRI was acquired one or two days prior to the operation under general anesthesia to reduce movement artefacts for optimal surgical planning. The DBS protocol included structural sagittal T1-weighted (1-mm slice thickness) and axial and sagittal T2-weighted (2 mm slice thickness) MRI sequences for trajectory planning. On the day of surgery, a CT scan was performed with a mounted stereotactic frame and fused to the MRI data including the planned trajectories. Target planning was based on MRI anatomy rather than atlas-coordinates in all patients, according to the publication of Bejjani [3]. Nevertheless, atlas coordinates for the central trajectory, related to the mid-commissural point, were determined and documented, as well as the width of the third ventricle. We sought to apply five parallel microelectrode trajectories for each side, but omitted one or more trajectories, if critical cerebral structures were threatened by placing of the electrodes (e.g., blood vessels, sulci, ventricles). For postoperative imaging, a CT scan with 1-mm slice thickness was performed to verify surgery results.
Anesthesiologic regimen
Intraoperative microelectrode recording (MER) and clinical testing was performed in a patient-awake state in all cases. However, from 2002 to 2006 (21 patients), the procedure followed the asleep-awake-asleep-awake protocol with patients receiving sedation (remifentanil and propofol) for skin incision and burr hole trepanation. Sedative drugs were stopped prior to MER and clinical testing.
All subsequent patients were operated with psychological support by the anesthesiologist preferably without any sedative drugs according our awake-awake-awake-protocol [39].
Intraoperative clinical testing
Clinical testing was performed with the macro tip of the microelectrodes (FHC, Bowdoin, ME) starting with the trajectory, that matched best to the anterior-superior-lateral (“sensorimotor”) part of the STN [24]. Depending on the clinical thresholds and the occurrence of side effects we tested 0-3 additional trajectories with STN-positive MER signals at 2–3 different depths, each. Intraoperative clinical testing graded finger tapping and fast, alternating pronation/supination movements of the hands for bradykinesia as well as standardized assessment of rigidity and tremor according to the United Parkinson’s Disease Rating Scale Part III (UPDRS). Improvements were documented in 25% steps as compared to baseline for every amplitude applied.
Documentation of side effects included dysarthria, contralateral facial or limb contractions, paresthesia, diplopia and ptosis as well as conjugated eye deviations. Improvements of symptoms were expected to start at 1–2 mA. Testing for side effects was stopped as soon as reproducible side effects occurred or extended up to a maximum of 6 mA stimulation intensity. The optimal intraoperative stimulation site was defined as the location with the earliest reduction of symptoms and a high threshold for side effects. Having found the optimal stimulation site, the FHC electrode was removed and replaced by a quadripolar (3389, Medtronic, Minneapolis, MN) or octopolar (Abbott (former St. Jude Medical)), or Boston Scientific (Marlborough, US) DBS electrode under fluoroscopic control.
Intraoperative disorientation was determined by patients’ sudden unawareness of their surroundings, including (i) head fixation in stereotactic frame, (ii) recognition of the treating physicians, (iii) understanding of the presented exercises, and (iv) tendency of trying to get up from the operating table.
Statistical analysis
Demographic and clinical data was analyzed using one-sided Fisher’s exact tests and t-tests. The presence or absence of somnolence and disorientation, as well as application of apomorphine and sedative drugs were encoded binarily. For analyses of frequencies of categorical parameters, two-tailed Chi square tests and Fischer’s Exact tests were performed. Correlation between sedation and intraoperative somnolence was also analyzed by logistic regression analysis. All statistical analysis was performed using IBM SPSS Statistics software (versions 25 and 29, Armonk, NY, IBM Corp). A p-value of ≤ 0.05 was considered statistically significant.
Results
Sedative drugs
In total, 21 patients received sedative drugs (propofol and remifentanil) during skin incisions and burr hole trepanations. The remaining 101 patients were operated without or only with minimal sedation during surgery. In the sedated group, 38.1% (8/21) of the patients presented with somnolence during clinical testing after electrode placement on the first side. In the non-sedated group, somnolence occurred in 14.9% (15/101) on the first operated side (p=0.019, Table 1). On the second operated side, 52.4% (11/21) in the sedated group versus 18.8% (19/101) in the non-sedated group presented with somnolence during clinical testing (p=0.004, Table 1). No significant difference could be observed for the occurrence of intraoperative disorientation (p=0.284, Table 1).
Peri-operative apomorphine
In 41 patients, oral L-DOPA medication was withdrawn one day prior to surgery without any subcutaneous apomorphine substitution (no-apomorphine group). Of these 41 patients in the no-apomorphine group, 21 received sedative drugs during surgery. In the remaining 81 patients, subcutaneous apomorphine was started several days prior to surgery and stopped one hour before the procedure (apomorphine group). All patients who received perioperative apomorphine were in the non-sedated group.
After the insertion of microelectrodes on the first operated side, 24.4% (10/41) patients of the no-apomorphine group developed somnolence, whereas 16.0% (13/81) in the apomorphine group presented with somnolence (p=0.192, Table 1). This trend was significant for the second operated side, where 36.6% (15/41) of patients in the no-apomorphine group developed somnolence and 18.5% (15/81) of the apomorphine group presented with this symptom (p=0.026, Table 1). Again, for intraoperative disorientation, no significant difference could be observed (p=0.115, Table 1).
To test for the bias caused by the sedation in the non-apomorphine group, we then analyzed the effect of apomorphine application only for patients in the non-sedated group. No significant difference could be observed (p=0.390 and p=0.550 for somnolence at first and second operated side, respectively).
MRI on the day of surgery
Nine patients received the MRI for stereotactic planning under general anesthesia on the day of surgery, while for 113 patients the MRI was performed a few days prior to the procedure (under general anesthesia). While no significant difference of the occurrence of somnolence could be observed after the first operated side between the two groups (p=0.226, Table 1), the performance of the MRI on the day of the procedure resulted in significantly higher incidence of somnolence after the second operated side (55.6% versus 22.1%, p=0.040, Table 1). No difference could be observed for the occurrence of intraoperative disorientation.
As the use of (i) sedatives, (ii) the application of apomorphine, and (iii) performing the MRI on the day of the surgery significantly correlated with the occurrence of intraoperative somnolence, we further tested patient and procedural characteristics related to these variables. Specifically, we analyzed the age, duration of Parkinson’s disease prior to DBS surgery, and the width of the 3rd ventricle (as a marker for brain atrophy). Concerning the extent of L-DOPA dependency, we included UPDRS scores (off-medication), UPDRS improvement (in %) and the pre-operative L-DOPA equivalent dose in the analysis. As the performance of the MRI on the day of the surgery increased the duration of the procedure, we included the duration of the surgical and the complete procedure, the beginning of the surgery (in minutes after midnight) and the number of MER used.
The occurrence of intraoperative disorientation did not associate with any of the variables mentioned above. Therefore, only the occurrence of intraoperative somnolence was evaluated in the following analyses.
Age
While no difference in the occurrence of somnolence could be seen after the first operated side in the sedated group, patients presenting with somnolence after placement of microelectrodes on the second operated side were significantly older than patients in whom somnolence did not occur (64.0 ± 6.4 years versus 61.0 ± 7.4 years, p=0.039, Table 2). No correlation could be seen in the non-sedated group (p>0.05, Table 3).
Duration of disease prior to surgery
There was no significant correlation of the intraoperative somnolence and the duration of PD prior to the DBS surgery. However, a trend could be seen for the second operated side (12.5 ± 4.0 years versus 10.9± 4.6 years, p = 0.080, Table 2). No correlation could be seen in the non-sedated group (p>0.05, Table 3).
UPDRS prior to surgery: off-medication-state and extent of improvement
The preoperative UPDRS in off-medication-state did not significantly correlate with the occurrence of intraoperative somnolence on the first operated side (p=0.248), while a trend was observable for the second operated side (p=0.071, Table 2). For the extent of UPDRS improvement (in %), a significant correlation could be seen for the second operated side (p=0.046, Table 2). No correlation was found in the non-sedated group (p>0.05, Table 3).
Width of 3rd ventricle (in [mm])
The width of the third ventricle as an indirect indicator for brain atrophy did not seem to have any influence on the occurrence of somnolence during the procedure (p>0.05, Table 2). No correlation could be seen in the non-sedated group (p>0.05, Table 3).
Pre-operative L-DOPA equivalent dose (in [mg])
The amount of the pre-operative L-DOPA equivalent dose did not significantly differ between the patients with or without intraoperative somnolence (p>0.05, Table 2). No correlation could be seen in the non-sedated group (p>0.05, Table 3).
Beginning of surgery (in [min] after midnight)
The beginning of the surgical procedure (as the time of first skin incision after midnight) was significantly later in the patients presenting with somnolence after both, the first and the second operated side (p=0.049 and p=0.027, respectively, Table 2). No correlation could be seen in the non-sedated group (p>0.05, Table 3).
Duration of surgical and complete procedure (in [min])
The duration of the surgical DBS procedure (from first skin incision to last skin closure) did not significantly correlate with the occurrence of intraoperative somnolence (p=0.341 and p=0.082 for first and second side respectively, Table 2). However, the overall time of the procedure on the day of the surgery (starting with the application of the stereotactic frame and ending with the last skin closure) was significantly longer in patients who developed somnolence on the second operated side (p= 0.020, Table 2). No correlation could be seen in the non-sedated group (p>0.05, Table 3).
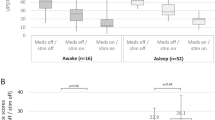
Number of microelectrode trajectories
Intraoperative somnolence did not occur in patients with few MER (1 or 2 MER on the first operated side, 2 or 4 total MER). 21.3%, 14.6%, and 26.7% of patients receiving 5, 4, or 3 MER on the first operated side presented with intraoperative somnolence, respectively (Fig. 1). Taking the number of MER trajectories together, somnolence occurred in 28.8% of patients with 10 MER trajectories and 12.0% of patients with 9 MER. Patients with 5 MER trajectories on the first operated side presented significantly more often with intraoperative somnolence compared to patients with 1–3 MER (p=0.041, Fig. 1). When looking at the total number of MER trajectories, patients with 10 trajectories (n=52) tended to present more frequently with somnolence (28.8% versus 12.0%) compared to patients with a total of 9 trajectories (n=25, p=0.102, Fig. 1).
The occurrence of disorientation was found more frequently in patients with 10 trajectories (19.2%) than in patients with 9 (8.0%; p=0.023) or in patients with 8 trajectories (9.1%; p=0.041).
AC-PC coordinates of the planned targets
Next, we wanted to test whether electrode placement might have influenced the occurrence of intraoperative somnolence. Regarding the whole collective, the planned targets tended to be more medial (p=0.060) and more inferior (p=0.051, Suppl. Table 1) in patients with somnolence and disorientation as in patients who did not deteriorate. In the anterior-posterior direction (y-coordinate) no differences were found (Suppl. Table 1). We then analyzed the sedated and non-sedated subgroups separately and found no significant differences concerning the x-, y-, z-coordinates in the non-sedated group. In the sedated group the planned target coordinates were significantly more medial (p=0.045) and more inferior (p=0.052) in patients with intraoperative somnolence (Suppl. Table 2).
To account for the use of sedative drugs, we then analyzed the patient and procedural characteristics for the non-sedated subgroup only. No significant correlation could be observed, indicating that the use of sedative drugs is the main contributing variable for the occurrence of intraoperative somnolence during DBS for PD patients. Logistic regression analysis confirmed a significant correlation between the use of sedative drugs and intraoperative somnolence (p=0.017 and p=0.002 for first and second operated side, respectively) with an odds ratio of 3.528 (95% confidence interval 1.250–9.957) and 4.747 (95% confidence interval 1.762–12.791) for first and second operated side, respectively. Patients that presented with intraoperative somnolence were therefore 3.528 to 4.747 times more likely to have received sedative drugs during the DBS procedure.
Discussion
In awake DBS procedures, somnolence and disorientation may occur during the operation which might hamper the reliability of clinical testing, performed to find the optimal stimulation area for the individual patient [4, 11, 15, 25, 31].
In deep brain stimulation, the validity and necessity of intraoperative clinical testing has been questioned repeatedly [2]. The majority of comparative studies concerning awake versus asleep procedures did not find significant differences with regard to the postoperative benefit of the patients [6, 8, 9, 13, 14, 18,19,20, 22, 27, 33, 37]. However, the execution of awake DBS procedures is quite heterogeneous, if at all reported in detail, which makes a generalization of the results difficult.
In this study, we show that the usage of analgesics and sedatives during DBS surgery is the main influencing factor for the occurrence of intraoperative somnolence which reduces the reliability and validity of intraoperative clinical testing. In our institution, we have developed an interdisciplinary approach to awake DBS surgery with psychological support for the patients by the anesthesiologist [24, 40]. We initially tended to assume that we increase the patients’ comfort by the application of intra-operative analgesics and sedatives to avoid the stress during skin incisions and burr hole trepanation. Yet, we observe a much greater discomfort when patients wake up after sedation in an unfamiliar environment. Pulse rate and blood pressure then rise significantly and are combined with a palpable state of anxiety, which further hampers the reliability of intra-operative testing [16]. Omitting the drugs and providing psychological assistance during the whole procedure significantly reduced autonomic and mental stress reactions. Clinical testing can start immediately when needed and without the restriction of reduced vigilance and compliance due to prior sedation [24, 40].
While the use of sedatives seems to be the main contributing factor, prolonged L-DOPA deprivation and any means increasing the time of the DBS procedure might also influence the occurrence of intraoperative somnolence, thus hindering meaningful intraoperative clinical testing. In this study we found that the drastic reduction of the period of dopamine deprivation by using perioperative subcutaneous apomorphine application reduced the occurrence of somnolence during the procedure. Similarly, the later the surgery starts and the longer the operation lasts, the longer the time of dopamine deprivation will be. In addition, patients are prone to get tired in long procedures which further reduces compliance and vigilance. It is not surprising that patients who went through MRI scans under general anesthesia on the day of surgery, following a night without dopamine substitution and having received sedative drugs during the operation were those with the highest rates of somnolence and disorientation.
We assumed that the number of microelectrode trajectories in a patient would correlate with the incidence of somnolence and disorientation as the length of the clinical testing, MER recording, and therefore the procedure increases with a greater number of trajectories. Also, more severe trauma to the brain is caused [17, 41]. Yet, the correlation was not as clear as anticipated. In the total collective, we found a significantly higher incidence of somnolence and disorientation in patients with 5 compared to patients with 1-3 trajectories on the first operated side. This might be explained by the low number of patients with only 1–3 MER trajectories, as the vast majority of our patients had received 4 or 5 trajectories on the first operated side and 8, 9, or 10 trajectories taken both sides together.
There are several limitations in this study, mainly that some of the subgroups were mutually exclusive (e.g., sedation and apomorphine treatment) which hinders the statistical comparison of these groups. Another influencing factor, which was not investigated in the present study was the path of the trajectories of the electrodes through the brain. For example, Witt et al. pointed out that if the electrodes traverse the caudate nucleus postoperative cognitive deficits might occur [38], even though the study results could not be replicated by Bot et al. [7].
The goal of awake DBS surgery includes not only the functional verification of the ideal electrode placement as determined by MRI and anatomy, but to clinically determine optimal electrode placement with a good clinical benefit (minimal stimulation needed with wide therapeutic range) and minimization of adverse effects before permanent implantation. This benefit of awake DBS procedures requires a vigilant and cooperative patient for intraoperative testing. The present study sheds light on possible influencing factors (i.e., use of sedatives, increased length of DBS procedure, prolonged L-DOPA withdrawal) that might be accountable for the occurrence of intraoperative somnolence and disorientation, both of which limit the reliability of clinical testing in awake DBS surgery.
As these factors influence patients’ intraoperative vigilance and cooperation, they need to be considered individually when planning patients’ DBS procedures. If they cannot be omitted or considered due to institutional or personal/patient requirements or circumstances, the advantages of awake surgery might be lost and an asleep procedure might be non-inferior to the awake surgery with intraoperative testing.
However, when awake DBS surgery is performed, especially the use of sedatives should be avoided by any means.
Abbreviations
- AC-PC line:
-
Anterior commissure - posterior commissure line
- DBS:
-
Deep brain stimulation
- MER:
-
Microelectrode recording
- PD:
-
Parkinson’s disease
- STN:
-
Subthalamic nucleus
- UPDRS:
-
Unified Parkinson’s Disease Rating Scale
References
Abosch A, Timmermann L, Bartley S, Rietkerk HG, Whiting D, Connolly PJ, Lanctin D, Hariz MI (2013) An international survey of deep brain stimulation procedural steps. Stereotact Funct Neurosurg 91:1–11
Aziz TZ, Hariz M (2017) To sleep or not to sleep during deep brain stimulation surgery for Parkinson disease? Neurology
Bejjani BP, Dormont D, Pidoux B, Yelnik J, Damier P, Arnulf I, Bonnet a M, Marsault C, Agid Y, Philippon J, Cornu P (2000) Bilateral subthalamic stimulation for Parkinson’s disease by using three-dimensional stereotactic magnetic resonance imaging and electrophysiological guidance. J Neurosurg 92:615–625
Benabid AL, Krack PP, Benazzouz A, Limousin P, Koudsie A, Pollak P (2000) Deep brain stimulation of the subthalamic nucleus for Parkinson’s disease: methodologic aspects and clinical criteria. Neurology 55:S40–S44
Blasberg F, Wojtecki L, Elben S, Slotty PJ, Vesper J, Schnitzler A, Groiss SJ (2018) Comparison of Awake vs. Asleep Surgery for Subthalamic Deep Brain Stimulation in Parkinson’s Disease. Neuromodulation 2018
Blume J, Schlaier J, Rothenfußer E, Anthofer J, Zeman F, Brawanski A, Bogdahn U, Lange M (2017) Intraoperative clinical testing overestimates the therapeutic window of the permanent DBS electrode in the subthalamic nucleus. Acta Neurochir (Wien) 159:1721–1726
Bot M, van den Munckhof P, Schmand BA, de Bie RMA, Schuurman PR (2018) Electrode penetration of the caudate nucleus in deep brain stimulation surgery for Parkinson’s disease. Ster Func Neurosurg 96(4):223–230
Brodsky MA, Anderson S, Murchison C, Seier M, Wilhelm J, Vederman A, Burchiel KJ (2017) Clinical outcomes of asleep vs awake deep brain stimulation for Parkinson disease. Neurology
Chen T, Mirzadeh Z, Chapple KM, Lambert M, Shill HA, Moguel-Cobos G, Tröster AI, Dhall R, Ponce FA (2019) Clinical outcomes following awake and asleep deep brain stimulation for Parkinson disease. J Neurosurg
Coenen VA, Honey CR, Hurwitz T, Rahman AA, McMaster J, Bürgel U, Mädler B (2009) Medial forebrain bundle stimulation as a pathophysiological mechanism for hypomania in subthalamic nucleus deep brain stimulation for Parkinson’s disease. Neurosurgery 64:1106–1114
Deep-Brain Stimulation for Parkinson’s Disease Study Group, Obeso JA, Olanow CW, Rodriguez-Oroz MC, Krack P, Kumar R, Lang AE (2001) Deep-brain stimulation of the subthalamic nucleus or the pars interna of the globus pallidus in Parkinson’s disease. N Engl J Med 345:956–963
Deuschl G, Schade-Brittinger C, Krack P, Volkmann J, Schäfer H, Bötzel K, Daniels C, Deutschländer A, Dillmann U, Eisner W, Gruber D, Hamel W, Herzog J, Hilker R, Klebe S, Kloß M, Koy J, Krause M, Kupsch A et al (2006) A Randomized Trial of Deep-Brain Stimulation for Parkinson’s Disease. N Engl J Med 355:896–908
Engelhardt J, Caire F, Damon-Perrière N, Guehl D, Branchard O, Auzou N, Tison F, Meissner WG, Krim E, Bannier S, Bénard A, Sitta R, Fontaine D, Hoarau X, Burbaud P, Cuny E (2020) A Phase 2 randomized trial of asleep versus awake subthalamic nucleus deep brain stimulation for Parkinson’s disease. Stereotact Funct Neurosurg
Foltynie T, Zrinzo L, Martinez-Torres I, Tripoliti E, Petersen E, Holl E, Aviles-Olmos I, Jahanshahi M, Hariz M, Limousin P (2011) MRI-guided STN DBS in Parkinson’s disease without microelectrode recording: efficacy and safety. J Neurol Neurosurg Psychiatry 82:358–363
Goodman RR, Kim B, McClelland S, Senatus PB, Winfield LM, Pullman SL, Yu Q, Ford B, McKhann GM (2006) Operative techniques and morbidity with subthalamic nucleus deep brain stimulation in 100 consecutive patients with advanced Parkinson’s disease. J Neurol Neurosurg Psychiatry 77:12–17
Hansen E, Seemann M, Zech N, Doenitz C, Luerding R, Brawanski A (2013) Awake craniotomies without any sedation: The awake-awake-awake technique. Acta Neurochir (Wien) 155:1417–1424
Hariz MI (2002) Safety and risk of microelectrode recording in surgery for movement disorders. Stereotact Funct Neurosurg 78:146–157
Ho AL, Ali R, Connolly ID, Henderson JM, Dhall R, Stein SC, Halpern CH (2017) Awake versus asleep deep brain stimulation for Parkinson’s disease: a critical comparison and meta-analysis. J Neurol Neurosurg Psychiatry jnnp-2016-314500
Holewijn RA, Verbaan D, van den Munckhof PM, Bot M, Geurtsen GJ, Dijk JM et al (2021) General Anesthesia vs local anesthesia in microelectrode recording–guided deep-brain stimulation for Parkinson disease. JAMA Neurol 78(10):1212. https://doi.org/10.1001/jamaneurol.2021.2979
Jin H, Gong S, Tao Y, Huo H, Sun X, Song D, Xu M, Xu Z, Liu Y, Wang S, Yuan L, Wang T, Song W, Pan H (2020) A comparative study of asleep and awake deep brain stimulation robot-assisted surgery for Parkinson’s disease. npj Park Dis 6:1–7
Klotz U (2009) Pharmacokinetics and drug metabolism in the elderly. Drug Metab Rev 41:67–76
Kochanski RB, Sani S (2018) Awake versus asleep deep brain stimulation surgery: Technical considerations and critical review of the literature. Brain Sci 8
Lambert C, Zrinzo L, Nagy Z, Lutti A, Hariz M, Foltynie T, Draganski B, Ashburner J, Frackowiak R (2012) Confirmation of functional zones within the human subthalamic nucleus: Patterns of connectivity and sub-parcellation using diffusion weighted imaging. Neuroimage 60:83–94
Lange M, Zech N, Seemann M, Janzen A, Halbing D, Zeman F, Doenitz C, Rothenfusser E, Hansen E, Brawanski A, Schlaier J (2015) Anesthesiologic regimen and intraoperative delirium in deep brain stimulation surgery for Parkinson’s disease. J Neurol Sci 355
Limousin P, Krack P, Pollak P, Benazzouz A, Ardouin C, Hoffmann D, Benabid AL (1998) Electrical stimulation of the subthalamic nucleus in advanced Parkinson’s disease. N Engl J Med 339:1105–1111
Limousin P, Pollak P, Benazzouz A, Hoffmann D, Broussolle E, Perret JE, Benabid A-L (1995) Bilateral subthalamic nucleus stimulation for severe Parkinson’s disease. Mov Disord
Liu Z, He S, Li L (2019) General Anesthesia versus Local Anesthesia for Deep Brain Stimulation in Parkinson’s Disease: A Meta-Analysis. Stereotact Funct Neurosurg 97:381–390
Machado A, Rezai AR, Kopell BH, Gross RE, Sharan AD, Benabid A-L (2006) Deep brain stimulation for Parkinson’s disease: surgical technique and perioperative management. Mov Disord 21:S247–S258
Maltête D, Navarro S, Welter M-L, Roche S, Bonnet A-M, Houeto J-L, Mesnage V, Pidoux B, Dormont D, Cornu P, Agid Y (2004) Subthalamic stimulation in Parkinson disease. Arch Neurol 61:390
McGuigan S, Zhou S-H, Brosnan MB, Thyagarajan D, Bellgrove MA, Chong TT-J (2019) Dopamine restores cognitive motivation in Parkinson’s disease. Brain 142:719–732
Nakajima T, Zrinzo L, Foltynie T, Olmos IA, Taylor C, Hariz MI, Limousin P (2011) MRI-guided subthalamic nucleus deep brain stimulation without microelectrode recording: can we dispense with surgery under local anaesthesia? Stereotact Funct Neurosurg 89:318–325
Plantinga BR, Temel Y, Duchin Y, Uludağ K, Patriat R, Roebroeck A, Kuijf M, Jahanshahi A, ter Haar Romenij B, Vitek J, Harel N (2016) Individualized parcellation of the subthalamic nucleus in patients with Parkinson’s disease with 7T MRI. Neuroimage
Sammartino F, Rege R, Krishna V (2020) Reliability of intraoperative testing during deep brain stimulation surgery. Neuromodulation
Triantafillidis JK (2013) Sedation in gastrointestinal endoscopy: Current issues. World J Gastroenterol 19:463
Tsai S-T, Lin S-H, Lin S-Z, Chen J-Y, Lee C-W, Chen S-Y (2007) Neuropsychological effects after chronic subthalamic stimulation and the topography of the nucleus in parkinson’s diseasE. Neurosurgery 61:E1024–E1030
Venkatraghavan L, Luciano M, Manninen P (2010) Anesthetic management of patients undergoing deep brain stimulator insertion. Anesth Analg 110(4):1138–1145
Wang J, Ponce FA, Tao J, Yu H, Liu J, Wang Y, Luan G, Ou S (2020) Comparison of awake and asleep deep brain stimulation for Parkinson’s disease: a detailed analysis through literature review. Neuromodulation Technol Neural Interface 23:444–450
Witt K, Granert O, Daniels C, Volkmann J, Falk D, van Eimeren T, Deuschl G (2013) Relation of lead trajectory and electrode position to neuropsychological outcomes of subthalamic neurostimulation in Parkinson’s disease: results from a randomized trial. Brain 136:2109–2119
Zech N, Seemann M, Seyfried TF, Lange M, Schlaier J, Hansen E (2018a) Deep Brain Stimulation Surgery without Sedation. Stereotact Funct Neurosurg 96:370–378
Zech N, Seemann M, Seyfried TF, Lange M, Schlaier J, Hansen E (2018b) Deep Brain Stimulation Surgery without Sedation. Stereotact Funct Neurosurg 96:370–378
Zrinzo L, Foltynie T, Limousin P, Hariz MI (2012) Reducing hemorrhagic complications in functional neurosurgery: a large case series and systematic literature review. J Neurosurg 116:84–94
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the local ethics committee at the University Medical Center and conducted in accordance with the Declaration of Helsinki.
Informed consent
Not applicable.
Conflict of interest
Tobias Mederer and Daniel Deuter have received travel grants for educational purposes from Medtronic. Juergen Schlaier has received teaching fees from Medtronic and research support from St Jude Medical, Antisense Pharma, and Medtronic. Talks in the last years were partly sponsored by Medtronic, St Jude Medical, and BrainLab. In addition, he received compensation from Medtronic for his services as a consultant. The remaining authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Comments
This is an interesting retrospective study. The authors have investigated factors that influence the quality of intraoperative testing in the awake and semi-awake states during STN DBS surgery. We now enter a time where the pendulum swings toward more an more DBS-electrode implantation under general anesthesia.
This might not be the final word and we can envision that some patients will still benefit from awake surgery. This work shares important information as to how such surgery can be perfromed and what the pitfalls are.
Volker A. Coenen,
Freiburg, Germany
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mederer, T., Deuter, D., Bründl, E. et al. Factors influencing the reliability of intraoperative testing in deep brain stimulation for Parkinson’s disease. Acta Neurochir 165, 2179–2187 (2023). https://doi.org/10.1007/s00701-023-05624-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05624-4