Abstract
Background
Videoangiography using indocyanine green (ICG) has been used in the ophthalmologic field for a long time. It was introduced to the neurosurgical field several years ago but has been limited to vascular surgeries. We applied ICG videoangiography to brain tumor surgery and evaluated the usefulness.
Methods
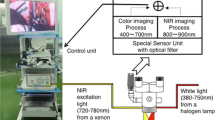
Twenty-three patients with a brain tumor who underwent microsurgical resection were analyzed. The pathological diagnosis was meningioma in 15 patients, metastasis in three, glioma in three, and hemangioblastoma in two. A microscope with a special filter and infrared excitation light to illuminate the operating field was used in this study. The intravascular fluorescence was imaged with a video camera attached to the microscope. ICG was injected intravenously with the dose of 5–25 mg, and overall, ICG was injected intraoperatively 32 times.
Results
ICG videoangiography allowed for an excellent evaluation of blood flow in the tumoral and peri-tumoral vessels both before and after the resection in all cases.
Conclusions
ICG videoangiography is a useful method for monitoring blood flow in the exposed vessels during microsurgery for a brain tumor. This noninvasive method is simple, safe, cost-effective, and easily repeatable. Before resection, it provides information on the tumoral and peri-tumoral circulation including sequential visualization of vessels or direction of the blood flow. After resection, it checks the patency of the peri-tumoral vessels and is especially useful for the vein. This ICG videoangiography can be an alternative tool to intraoperative angiography or Doppler ultrasonography in selective cases.





Similar content being viewed by others
References
Cochran ST, Bomyea K, Sayre JW (2001) Trends in adverse events after IV administration of contrast media. Am J Roentgenol 176:1385–1388
de Oliveira JG, Beck J, Seifert V, Teixeira MJ, Raabe A (2008) Assessment of flow in perforating arteries during intracranial aneurysm surgery using intraoperative near-infrared indocyanine green videoangiography. Neurosurgery 62:1300–1310
Ferroli P, Acerbi F, Albanese E, Tringali G, Broggi M (2011) Application of intraoperative indocyanine green angiography for CNS tumors: results on the first 100 cases. Acta Neurochir Suppl 109:251–257
Hänggi D, Etminan N, Steiger HJ (2010) The impact of microscope-integrated intraoperative near-infrared indocyanine green videoangiography on surgery of arteriovenous malformations and Dural arteriovenous fistulae. Neurosurgery 67:1094–1104
Hope-Ross M, Yannuzzi LA, Gragoudas ES, Guyer DR, Slakter JS, Sorenson JA, Krupsky S, Orlock DA, Puliafito CA (1994) Adverse reactions due to indocyanine green. Ophthalmology 101:529–533
Imizu S, Kato Y, Sangli A, Oguri D, Sano H (2008) Assessment of incomplete clipping of aneurysms intraoperatively by a near-infrared indocyanine green-video angiography (Niicg-Va) integrated microscope. Minim Invasive Neurosurg 51:199–203
Jing Z, Ou S, Ban Y, Tong Z, Wang Y (2010) Intraoperative assessment of anterior circulation aneurysms using the indocyanine green video angiography technique. J Clin Neurosci 17:26–28
Killory BD, Nakaji P, Gonzales LF, Ponce FA, Wait SD, Spetzler RF (2009) Prospective evaluation of surgical microscope-integrated intraoperative near-infrared indocyanine green angiography during cerebral arteriovenous malformation surgery. Neurosurgery 65:456–462
Ma C-Y, Shi J-X, Wang H-D, Hang C-H, Cheng H-L, Wu W (2009) Intraoperative indocyanine green angiography in intracranial aneurysm surgery: Microsurgical clipping and revascularization. Clin Neurol Neurosurg 111:840–846
Murai Y, Adachi K, Matano F, Tateyama K, Teramoto A (2011) Indocyanin green videoangiography study of hemangioblastomas. Can J Neurol Sci 38:41–47
Raabe A, Beck J, Gerlach R, Zimmermann M, Seifert V (2003) Near-infrared indocyanine green video angiography: a new method for intraoperative assessment of vascular flow. Neurosurgery 52:132–139
Woitzik J, Horn P, Vajkoczy P, Schmiedek P (2005) Intraoperative control of extracranial-intracranial bypass patency by near-infrared indocyanine green videoangiography. J Neurosurg 102:692–698
Acknowledgments
This work was supported by the Mid-career Researcher Program through a National Research Foundation grant funded by the Korean Ministry of Education, Science, and Technology (No. R01-2008-000-20545-0), and a faculty research grant of Yonsei University College of Medicine for 2008 (6-2008-0174) to Jong Hee Chang.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
The authors present their experience on brain tumor surgery assisted by the intra-operative use of indocyanine green videoangiography (ICG). In this series, ICG emerges as a simple, inexpensive, rapid, non-invasive, and reliable implementation for vascular management in the neuro-oncological setting. The authors report advantages and limits of the technique by means of an effectively illustrated surgical series. For educational purposes, we can synthesize that ICG might be functional to selected surgical scenarios. For example, when the tumor is located close to major vessels that could be potentially injured by surgery (i.e., Sylvian fissure tumors), when approaching high vascularized tumors (i.e., hemangioblastomas or some meningiomas), or when the direction of the blood flow of peri-tumoral vasculature must be recognized in a pre-resection stage in order to plan a correct removal strategy (i.e., cortical veins in parasagittal meningioma surgery).
We agree with the authors that brain tumor surgery can, in selected cases, take advantage of the intra-operative use of ICG. Further studies on a large series of patients are needed to define the real clinical impact of ICG on a patient’s outcome.
Domenico d’Avella
Alessandro Della Puppa
Padova, Italy
Comment
Intraoperative indocyanine green (ICG) angiography is an established method to support the microsurgical therapy of intracranial aneurysms and AVMs. The authors performed ICG angios during the removal of 15 meningiomas, three metastases, three gliomas, and two hemangioblastomas, which allowed them to make several useful findings at different phases of surgeries, including:
* localization of the sinus and cortical veins before opening the dura.
* visualization of feeding arteries, draining veins, and mass of a hemangioblastoma before opening the dura.
* relationship between an insular anaplastic astrocytoma and branches of the MCA.
* cortical vein patency in the tumor bed after removal of a meningioma.
* a vein thought to be open was not and could be sacrificed for a total removal.
The authors are to be congratulated for a timely addition to the growing list of instances during CNS tumor surgery in which ICG angio may reveal important aspects.
Juha E Jääskeläinen
Kuopio, Finland
Rights and permissions
About this article
Cite this article
Kim, E.H., Cho, J.M., Chang, J.H. et al. Application of intraoperative indocyanine green videoangiography to brain tumor surgery. Acta Neurochir 153, 1487–1495 (2011). https://doi.org/10.1007/s00701-011-1046-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-011-1046-x