Abstract
Purpose
Vascular resection (VR) is extended surgery to attain a negative radial margin (RM) for distal cholangiocarcinoma (DCC). The present study explored the significance of VR for DCC, focusing on VR, RM, and findings suggestive of vascular invasion on multidetector-row computed tomography (MDCT).
Methods
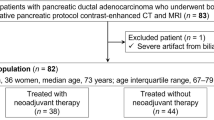
Patients with DCC who underwent resection between 2002 and 2019 were reviewed.
Results
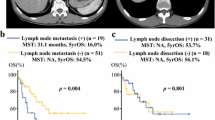
Among 230 patients, 25 received VR. The overall survival (OS) in the VR group was significantly worse than in the non-VR group (16.7% vs. 50.7% at 5 years, P < 0.001). Patients who underwent VR with a negative RM failed to show a better OS than those who did not undergo VR with a positive RM (19.7% vs. 35.7% at 5 years, P = 0.178). Of the 30 patients who were suspected of having vascular invasion on MDCT, 11 did not receive VR because the vessels were freed from the tumor; these patients had a significantly better OS (57.9% at 5 years) than those who underwent VR.
Conclusions
VR for DCC was associated with a poor prognosis, even if a negative RM was obtained. VR is not necessary for DCC when the vessels are detachable from the tumor.




Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during this study are available from the corresponding author on reasonable request.
References
DeOliveira ML, Cunningham SC, Cameron JL, Kamangar F, Winter JM, Lillemoe KD, et al. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg. 2007;245:755–62.
Komaya K, Ebata T, Shirai K, Ohira S, Morofuji N, Akutagawa A, et al. Recurrence after resection with curative intent for distal cholangiocarcinoma. Br J Surg. 2017;104:426–33.
Igami T, Nagino M, Oda K, Nishio H, Ebata T, Yokoyama Y, et al. Clinicopathologic study of cholangiocarcinoma with superficial spread. Ann Surg. 2009;249:296–302.
Park Y, Hwang DW, Kim JH, Hong SM, Jun SY, Lee JH, et al. Prognostic comparison of the longitudinal margin status in distal bile duct cancer: R0 on first bile duct resection versus R0 after additional resection. J Hepatobiliary Pancreat Sci. 2019;26:169–78.
Sakamoto Y, Kosuge T, Shimada K, Sano T, Ojima H, Yamamoto J, et al. Prognostic factors of surgical resection in middle and distal bile duct cancer: an analysis of 55 patients concerning the significance of ductal and radial margins. Surgery. 2005;137:396–402.
Kayahara M, Nagakawa T, Ohta T, Kitagawa H, Tajima H, Miwa K. Role of nodal involvement and the periductal soft-tissue margin in middle and distal bile duct cancer. Ann Surg. 1999;229:76–83.
Kurosaki I, Hatakeyama K, Minagawa M, Sato D. Portal vein resection in surgery for cancer of biliary tract and pancreas: special reference to the relationship between the surgical outcome and site of primary tumor. J Gastrointest Surg. 2008;12:907–18.
Miura F, Sano K, Amano H, Toyota N, Wada K, Yoshida M, et al. Evaluation of portal vein invasion of distal cholangiocarcinoma as borderline resectability. J Hepatobiliary Pancreat Sci. 2015;22:294–300.
Maeta T, Ebata T, Hayashi E, Kawahara T, Mizuno S, Matsumoto N, et al. Pancreatoduodenectomy with portal vein resection for distal cholangiocarcinoma. Br J Surg. 2017;104:1549–57.
Lyu S, Wang F, Ren Z, Cao D, He Q. Long-term survival in patients with distal cholangiocarcinoma after pancreaticoduodenectomy combined with portal vein system resection and reconstruction. Langenbecks Arch Surg. 2021;406:1917–24.
Burasakarn P, Higuchi R, Yazawa T, Uemura S, Izumo W, Matsunaga Y, et al. Hepatic artery resection without reconstruction in pancreatoduodenectomy. Langenbecks Arch Surg. 2021;406:2081–90.
Mizuno T, Ebata T, Yokoyama Y, Igami T, Yamaguchi J, Onoe S, et al. Combined vascular resection for locally advanced perihilar cholangiocarcinoma. Ann Surg. 2020;275:382–90.
Sugiura T, Uesaka K, Okamura Y, Ito T, Yamamoto Y, Ashida R, et al. Major hepatectomy with combined vascular resection for perihilar cholangiocarcinoma. BJS Open. 2021;5:zrab064.
Sobin LH, Gospodarowicz MK, Wittekind C. International union against cancer (UICC) TNM classification of malignant tumours. 7th ed. New York: Wiley-Liss; 2010.
Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12:1500–24.
Yamamoto R, Sugiura T, Okamura Y, Ashida R, Ohgi K, Yamada M, et al. A novel method for predicting perineural invasion of distal cholangiocarcinoma on multidetector-row computed tomography. Surg Today. 2021;52:774–82.
Yamamoto Y, Ashida R, Ohgi K, Sugiura T, Okamura Y, Ito T, et al. Combined antrectomy reduces the incidence of delayed gastric emptying after pancreatoduodenectomy. Dig Surg. 2018;35:121–30.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the international study group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017;161:584–91.
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. Posthepatectomy liver failure: a definition and grading by the international study group of liver surgery (ISGLS). Surgery. 2011;149:713–24.
Yasukawa K, Shimizu A, Motoyama H, Kubota K, Notake T, Fukushima K, et al. Impact of remnant carcinoma in situ at the ductal stump on long-term outcomes in patients with distal cholangiocarcinoma. World J Surg. 2021;45:291–301.
Sugiura T, Uesaka K, Okamura Y, Ito T, Yamamoto Y, Ashida R, et al. Adjuvant chemoradiotherapy for positive hepatic ductal margin on cholangiocarcinoma. Ann Gastroenterol Surg. 2020;4:455–63.
Yamamoto R, Sugiura T, Ashida R, Ohgi K, Yamada M, Otsuka S, et al. Converted-hepatopancreatoduodenectomy for an intraoperative positive ductal margin after pancreatoduodenectomy in distal cholangiocarcinoma. Langenbecks Arch Surg. 2022. https://doi.org/10.1007/s00423-022-02598-2.
Alves A, Farges O, Nicolet J, Watrin T, Sauvanet A, Belghiti J. Incidence and consequence of an hepatic artery injury in patients with postcholecystectomy bile duct strictures. Ann Surg. 2003;238:93–6.
Tohma T, Cho A, Okazumi S, Makino H, Shuto K, Mochiduki R, et al. Communicating arcade between the right and left hepatic arteries: evaluation with CT and angiography during temporary balloon occlusion of the right or left hepatic artery. Radiology. 2005;237:361–5.
Strasberg SM, Helton WS. An analytical review of vasculobiliary injury in laparoscopic and open cholecystectomy. HPB (Oxford). 2011;13:1–14.
Okada K, Kawai M, Hirono S, Miyazawa M, Shimizu A, Kitahata Y, et al. A replaced right hepatic artery adjacent to pancreatic carcinoma should be divided to obtain R0 resection in pancreaticoduodenectomy. Langenbecks Arch Surg. 2015;400:57–65.
Miura F, Asano T, Amano H, Yoshida M, Toyota N, Wada K, et al. Eleven cases of postoperative hepatic infarction following pancreato-biliary surgery. J Gastrointest Surg. 2010;14:352–8.
Hackert T, Stampfl U, Schulz H, Strobel O, Büchler MW, Werner J. Clinical significance of liver ischaemia after pancreatic resection. Br J Surg. 2011;98:1760–5.
D’Souza MA, Valdimarsson VT, Campagnaro T, Cauchy F, Chatzizacharias NA, D’Hondt M, et al. Hepatopancreatoduodenectomy-a controversial treatment for bile duct and gallbladder cancer from a European perspective. HPB (Oxford). 2020;22:1339–48.
Welch JC, Gleeson EM, Karachristos A, Pitt HA. Hepatopancreatoduodenectomy in North America: are the outcomes acceptable? HPB (Oxford). 2020;22:360–7.
Endo I, Hirahara N, Miyata H, Yamamoto H, Matsuyama R, Kumamoto T, et al. Mortality, morbidity, and failure to rescue in hepatopancreatoduodenectomy: an analysis of patients registered in the national clinical database in Japan. J Hepatobiliary Pancreat Sci. 2021;28:305–16.
Acknowledgements
The protocol for this research project was approved by a suitable institutional ethics committee and conformed to the provisions of the Declaration of Helsinki. The Institutional Review Board of Shizuoka Cancer Center approved the study (approval number J2020-135-2020-1-3).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests and no funding to declare.
Informed consent
Informed consent was substituted by the informed opt-out procedure because of the retrospective nature of the study, and anonymous clinical data were used for the analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
595_2022_2634_MOESM2_ESM.tiff
Supplementary file2 Supplementary Fig. 1 The overall survival according to the surgical procedure. PD pancreatoduodenectomy, HPD hepatopancreatoduodenectomy (TIFF 1944 KB)
595_2022_2634_MOESM3_ESM.tiff
Supplementary file3 Supplementary Fig. 2 The overall survival according to microscopic tumor invasion to the hepatic artery or portal vein in patients who underwent vascular resection (TIFF 1919 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yamamoto, R., Sugiura, T., Ashida, R. et al. Vascular resection for distal cholangiocarcinoma. Surg Today 53, 899–906 (2023). https://doi.org/10.1007/s00595-022-02634-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-022-02634-0