Abstract
Objective
To derive the health utility scores of type 2 diabetes (T2D) patients using basal insulin (BI) with diverse characteristics in China.
Methods
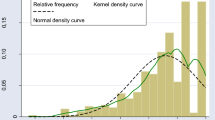
The study used the data of insulin-using T2D patients on BI treatment enrolled in the BEYOND II study, which is a multi-center, observational study from 78 hospitals nationwide. The 3-level EQ-5D (EQ-5D-3L) questionnaire was administered to each patient to derive their health utility scores using the EQ-5D-3L value set for China. Patients’ clinical and sociodemographic information were retrieved from their electronic case report form (eCRF). Ordinary least-square models with different specifications were explored to identify the best-fitting model to predict the utility scores.
Results
The sample (n = 12,583) achieved a mean (standard deviation) EQ-5D-3L utility score of 0.936 (0.120). According to the model, a Chinese male who was younger than 59 years, not underweight, diagnosed with T2D shorter than 10 years, with controlled plasma glucose and free of diabetes complications/comorbidities, would have a mean utility of 0.993. Being female, older age, underweight, and higher plasma glucose, longer diabetes duration was negatively related to EQ-5D-3L scores. Comorbidities and seven of eleven complications were associated with utility decrement. Interactions between some complications were also discovered.
Conclusions
The derived health utility scores for diabetes complications could facilitate the assessment of the cost-effectiveness of health interventions for Chinese insulin-using T2D patients.
Similar content being viewed by others
References
Federation ID (2019) IDF DIABETES ATLAS 9th edition 2019. Available at: https://diabetesatlas.org/data/en/. Accessed May 16 2020
Xu Y, Wang L, He J et al (2013) Prevalence and control of diabetes in Chinese adults. JAMA 310:948–959
Funnell MM (2008) Quality of life and insulin therapy in type 2 diabetes mellitus. Insulin 3:31–36
Gao LL, Ji LN, Lu JM et al (2014) Current status of blood glucose control and treatment of type 2 diabetes in China 2009–2012. Chin J Diabetes 22:594–598
Cai X, Shi L, Yang W et al (2019) Cost-effectiveness analysis of dapagliflozin treatment versus metformin treatment in Chinese population with type 2 diabetes. J Med Econ 22:336–343
Geng J, Yu H, Mao Y et al (2015) Cost effectiveness of dipeptidyl peptidase-4 inhibitors for type 2 diabetes. Pharmacoeconmics 33:581–597
Cheng H, Wan X, Ma J et al (2019) Cost-effectiveness of insulin degludec versus insulin glargine in insulin-naive chinese patients with type 2 diabetes. Clin Ther 41:445–455
Drummond MF, Sculpher MJ, Torrance GW, O’Brien B, Stoddart GL (2005) Methods for the economic evaluation of health care programmes, 3rd edn. Oxford University Press, New York
Dolan P (1997) Modeling valuations for EuroQol health states. Med Care 35:1095–1108
Brazier J, Roberts J, Deverill M (2002) The estimation of a preference-based measure of health from the SF-36. J Health Econ 21:271–292
Yfantopoulos J, Chantzaras A (2018) Health-related quality of life and health utilities in insulin-treated type 2 diabetes: the impact of related comorbidities/complications. Eur J Health Econ. 10.1007/s10198-020-01167-y.[Epub ahead of print]
Zhang P, Brown MB, Bilik D, et al. (2012) Health utility scores for people with type 2 diabetes in U.S. managed care health plans: results from translating research into action for diabetes (TRIAD). Diabetes Care 35 2250–2256
Morgan CL, McEwan P, Morrissey M et al (2006) Characterization and comparison of health-related utility in people with diabetes with various single and multiple vascular complications. Diabet Med 23:1100–1105
Bagust A, Beale S (2005) Modelling EuroQol health-related utility values for diabetic complications from CODE-2 data. Health Econ 14:217–230
Clarke P, Gray A, Holman R (2002) Estimating utility values for health states of type 2 diabetic patients using the EQ-5D (UKPDS62). Med Decis Mak 22:340–349
Coffey JT, Brandle M, Zhou H et al (2002) Valuing health-related quality of life in diabetes. Diabetes Care 25:2238–2243
Redekop WK, Koopmanschap MA, Stolk RP et al (2002) Health-related quality of life and treatment satisfaction in Dutch patients with type 2 diabetes. Diabetes Care 25:458–463
Zhang Y, Wu J, Chen Y et al (2020) EQ-5D-3L decrements by diabetes complications and comorbidities in China. Diabetes Ther 11:939–950
Pan CW, Sun HP, Zhou HJ et al (2016) Valuing health-related quality of life in type 2 diabetes patients in China. Med Decis Mak 36:234–241
Weng J, Zhao J, Zhou Z et al (2020) Observational study evaluating the effectiveness of physician-targeted education for improving glycemic management of patients with type 2 diabetes (BEYOND II). J Diabetes 12:66–76
Liu GG, Wu H, Li M et al (2014) Chinese time trade-off values for EQ-5D health states. Value Health 17:597–604
Wang H, Kindig DA, Mullahy J (2005) Variation in Chinese population health related quality of life: results from a EuroQol study in Beijing. China Qual Life Res 14:119–132
Zhao FL, Yue M, Yang H et al (2010) Validation and comparison of EuroQol and short form 6D in chronic prostatitis patients. Value Health 13:649–656
Wang HM, Patrick DL, Edwards TC et al (2012) Validation of the EQ-5D in a general population sample in urban China. Qual Life Res 21:155–160
Pan CW, Wang S, Wang P et al (2018) Diabetic retinopathy and health-related quality of life among Chinese with known type 2 diabetes mellitus. Qual Life Res 27:2087–2093
Lu Y, Wang N, Chen Y et al (2017) Health-related quality of life in type-2 diabetes patients: a cross-sectional study in East China. BMC Endocr Disord 17:38
Jiao F, Wong CKH, Gangwani R et al (2017) Health-related quality of life and health preference of Chinese patients with diabetes mellitus managed in primary care and secondary care setting: decrements associated with individual complication and number of complications. Health Qual Life Outcomes 15:125
Beaudet A, Clegg J, Thuresson PO et al (2014) Review of utility values for economic modeling in type 2 diabetes. Value Health 17:462–470
Sakamaki H, Ikeda S, Ikegami N et al (2006) Measurement of HRQOL using EQ-5D in patients with type 2 diabetes mellitus in Japan. Value Health 9:47–53
Pan CW, Cong XL, Zhou HJ et al (2018) Evaluating health-related quality of life impact of chronic conditions among older adults from a rural town in Suzhou. China Arch Gerontol Geriatr 76:6–11
Yan LL, Daviglus ML, Liu K et al (2004) BMI and health-related quality of life in adults 65 years and older. Obes Res 12:69–76
Acknowledgments
The authors would like to thank Prof. Chen Wen from School of Public Health, Fudan University for facilitating the study
Funding
This study is supported by Sanofi China.
Author information
Authors and Affiliations
Contributions
Chaoyun Li and Pei Wang designed the study and analyzed the data. Pei Wang drafted the manuscript. All authors reviewed and approved to publish the final version.
Corresponding author
Ethics declarations
Conflict of interest
Chaoyun Li is an employee of Sanofi China; Pei Wang has received the research grant from Sanofi China.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the the Clinical Trial Ethics Committee of the Third Ailiated Hospital, Sun Yat-sen University (Reference Number [2015] 2–152 on 21 July 2015) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all participants at the time of data collection.
Data availability statement
Qualified researchers may request access to patient-level data and related study documents including the clinical study report, study protocol with any amendments, blank case report form, statistical analysis plan, and dataset specifications. Patient-level data will be anonymized, and study documents will be redacted to protect the privacy of trial participants. Further details on Sanofi’s data-sharing criteria, eligible studies, and process for requesting access can be found at: ‘https://www.clinicalstudydatarequest.com.’
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to the topical collection Health Education and Psycho-Social Aspects, managed by Massimo Porta and Marina Trento.
Appendices
Appendix 1: Goodness of fit of the three OLS models in the modeling sample
See Table
Appendix 2: Goodness of fit of the three OLS models in the validation sample
See Table
Rights and permissions
About this article
Cite this article
Li, C., Zhou, H. & Wang, P. Health utility of type 2 diabetes patients using basal insulin in China: results from the BEYOND II study. Acta Diabetol 58, 329–339 (2021). https://doi.org/10.1007/s00592-020-01618-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-020-01618-1