Abstract
Purpose
During the posteromedial approach to the tibial plateau fracture (TPF), pes anserine is generally retracted. However, pes anserine detachment could provide a better fracture site exposure. Even so, the general conception is that the latter could negatively affect flexor muscle strength. We aimed to evaluate the effect of pes anserine detachment on the flexion force and functional outcomes of TPF with posteromedial involvement.
Methods
In this retrospective-prospective cohort study, 22 TPF patients with Schatzker type IV who were managed with posteromedial approach and pes anserine detachment were included. The knee flexion force was measured 12 months after the surgery at several angles of flexion (30°, 60°, and 90°) and rotations (internal and external). The International Knee Documentation Committee (IKDC) and the Knee Injury and Osteoarthritis Outcome Score (KOOS) were used to assess knee function. A visual analog scale (VAS) was used to measure knee pain.
Results
The mean strength of the knee flexor muscle was not statistically different between the involved and non-involved sides at 30°, 60°, and 90° knee flexion, and also at the internal and external rotation. The mean IKDC score of the patients was 81.6 ± 7.8. The mean KOOS score of the patients was 82.2 ± 9.1. The mean VAS for pain was 2.4 ± 1.8. The mean knee range of motion was 124 ± 10.5°.
Conclusion
Pes anserine release and re-attachment in the posteromedial approach to the TPF has no detrimental effect on the flexion muscle strength and knee function.
Level of Evidence
Therapeutic Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tibial plateau fracture (TPF) is associated with a complication rate as high as 54% [1, 2]. Therefore, optimization of the TPF surgery is of considerable importance.
For TPF involving the posteromedial portion of the tibial plateau, a posteromedial approach is generally implemented to minimize intraoperative soft-tissue injury [3, 4]. In this approach, the pes is usually retracted to expose the fracture site [5]. This retraction does not generally provide a complete exposure. Pes release may allow for improved fracture site exposure and fixation, therefore enhancing TPF treatment outcomes [5]. Many surgeons, however, do not undertake this procedure due to worries regarding the potential negative effects of this release on flexor muscle strength [6, 7].
In this study, we compared the flexor muscle strength between the involved and non-involved knee following the treatment of TPF with a posteromedial approach and pes release. We hypothesized that if pes release in the posteromedial approach of TPF surgery does not cause a significant reduction in flexor muscle strength of the involved knee, it could be implemented instead of pes retraction to ensure better fracture site exposure, thereby leading to a superior fixation and more favorable surgical outcomes.
Patients and methods
This retrospective-prospective study was approved by the review board of our institute under the code IR.IUMS.REC.1400.1252. Medical profiles of 62 TPF patients who were treated with a posteromedial approach and pes release between 2016 and 2020 were retrospectively reviewed. The inclusion criteria were Schatzker type IV [8] and a minimum follow-up of 1 year. Exclusion criteria for the study included patients with an associated knee injury requiring extra-intervention, lateral plateau involvement, involvement of lateral leg muscles, a history of surgical treatment in the ipsilateral limb, pre-injury malunion, or non-union in the ipsilateral limb, severely limited range of motion in the involved knee, and history of the neurologic or rheumatologic disorder. Patients whose medical records were insufficient or who were lost to follow-up were also excluded from the research. Finally, 34 patients were identified as eligible for this study. Twenty-two patients were available for final follow-up and were included in the final analysis.
Surgical technique
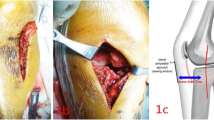
The patient was placed in the supine position while the patient's knee was rotated to the outside (figure of four), and a tourniquet was inflated. Then, a longitudinal incision was performed, beginning roughly 3 cm from the proximal joint portion and finishing at the desired distal joint portion. The nerve of the Saphenous was retracted. During the incision, the fascia was also cut. Pes anserine and the medial head of gastrocnemius were approached by a posteromedial approach (Fig. 1). Pes anserine was released from its distal part (tibial attachment) with a one-centimeter stump. To avoid retraction of the detached pes anserine, it was kept with a suture Vicryl; polyglactin; Ethicon, Johnson & Johnson) during the procedure (Fig. 2). Then, the fracture was exposed through the space between the medial collateral ligament and medial head of the gastrocnemius. The medial collateral ligament was preserved. Then, the fracture was fixed by a plate and screw system (3.5-mm T-plate; Mork-Med, Germany, Fig. 3). The tendon and muscles are re-attached to their previous insertion site using Vicryl-coated absorbable suture (2 Vicryl; polyglactin; Ethicon, Johnson & Johnson).
Intraoperative photographs of tibial plateau fracture surgery with posteromedial approach: a detachment of pes anserine with 1 cm stump and fracture exposure through medial collateral ligament and medial head of the gastrocnemius; b preserving the pes anserine using a suture to avoid its retraction; c Pes anserine repair after fracture reduction and fixation
Postoperative protocol
Postoperative protocols were included active rehabilitation with isometric knee exercises that were started 1 day after the operation and range of motion as tolerated, aiming to achieve full active extension and 90° of knee flexion by the end of the 4 weeks. The patient was allowed partial weight bearing with crutch. Crutches were weaned off progressively from the 8 to 10 weeks after the operation, when sign of union was observed in the radiographic evaluation. Physiotherapy was implemented to strengthen the limb and improve muscles strength, proprioception, and range of motion in patient with poor compliance during follow up.
Outcome measures
All the evaluations were done by one orthopedic surgeon who was not involved in the patients’ care. The outcome of interest was postoperative complication, knee range of motion, knee pain, knee function, and flexor muscle strength. Knee range of motion (ROM) was evaluated with a goniometer. Knee pain was measured using a visual analog scale (VAS) for pain. Accordingly, a score between 0 and 10 was given to each patient, with zero signifying no pain and 10 indicating extreme suffering. The knee function was assessed using the Persian translation of the International Knee Documentation Committee (IKDC) and the Knee injury and Osteoarthritis Outcome Score (KOOS). Both IKDC and KOOS were rated between 0 and 100, whereas a higher score was indicative of greater function. The validity and reliability of the questionnaires in the Persian language were approved in earlier studies [9, 10].
A manual dynamometer (Manual Masucle Tester, M-202) evaluated the flexor muscle strength of the injured and non-injured knees. First, the patients were asked to ride a stationary bike for 5 min and perform hamstrings and quadriceps stretching exercises. Then, the flexor muscle strength was assessed at three angles of 30°, 60°, and 90° of knee flexion in both internal and external knee rotation, making six numbers for each limb and 12 numbers for each patient. Each evaluation was performed three times, and the average of three evaluations was regarded as the patient’s flexor muscle strength (Fig. 4).
Flexor muscle strength was evaluated two times for each limb and the largest value was considered in the analysis. The inter- and intra-observer reliability of the muscle strength evaluation was checked in a pilot study using intraclass correlation coefficient test and showed to be 0.89 and 0.91, respectively.
Statistical analysis
Statistical analysis was done with SPSS for Windows, version 16 (SPSS Inc., Chicago, Ill., USA). Descriptive data were presented by mean ± standard deviation for quantitative variables and with number and percentage for qualitative variables. Using the Kolmogorov–Smirnov test, the distributions’ normality was examined. Wilcoxon signed-rank test was used to compare the mean values between the two limbs. A P value less than 0.05 was determined to be statistically significant.
Results
Twenty-two TPF patients were included in the analysis. The study population consisted of 20 males and two females. The mean age of the patients was 41.1 ± 12.5 years (range 23–61). The mean follow-up of the patients was 16.5 ± 7.2 months (range 6–22) (Table 1).
The mean strength of knee flexor muscle at 30°, 60°, and 90° knee flexion was not significantly different between the involved and non-involved sides, both at internal rotation and external rotation status. The detailed flexor muscle strengths of the involved and non-involved knees are demonstrated in Table 2.
The mean IKDC score of the patients was 81.6 ± 7.8 (range 71–90). The mean KOOS score of the patients was 82.2 ± 9.1 (range 69–89). The mean VAS for pain was 2.4 ± 1.8 (range 1–4). The mean knee ROM was 124 ± 10.5° (range 100–135). All patients achieved bone union (bridging callus in 3 of 4 cortices) within an average of 11.2 ± 2.6 weeks (range 9–12). One varus deformity of 5° was the only postoperative complication in this series. No intervention was done for varus deformity because the patient had no complaints. No patient had pain in the incision site of over the pes anserine.
Discussion
We evaluated the effect of pes anserine release instead of retraction in the posteromedial approach of TPF surgery to provide better intraoperative exposure. The knee function, as measured by the IKDC score and KOOS, was satisfactory after this change. The average VAS for postoperative pain was 2.4. Knee range of motion averaged 124°. The flexor muscle strength was not significantly different between the involved and non-involved knees at different flexion degrees and knee rotations. No major postoperative complication was observed in our series.
Pes anserine is a critical factor in knee flexion force. In a biomechanical analysis, Di Stefano et al. [7] evaluated the impact of pes anserine transfer on the knee flexion force in 15 patients. The mean torque value of the quadriceps and hamstring in the involved knee was significantly reduced compared to the contralateral knee (192.2 ft-Ib vs. 221.3 ft-Ib and 116.1 ft-Ib vs. 129.1 ft-Ib, respectively). The mean internal rotation torque values at 90° were also significantly reduced in the involved knee (19.3 ft-Ib vs. 22.8 ft-Ib). Murakami et al. observed the same decrease in flexion force [6]. Although the influence of pes anserine muscles on knee flexion force is well-established, no previous research has examined the effect of pes anserine detachment and re-attachment on knee flexion force. The same reduction in flexion force was reported by Murakami et al. While the effect of pes anserine muscles on the knee flexion force is accepted, no earlier study is available regarding the effect of pes anserine detachment and re-attachment on the knee flexion force. We hypothesized that temporary detachment of pes anserine from its tibial attachment for better exposure of TPF during the posteromedial approach and its re-attachment after fracture reduction and fixation does not affect the knee flexion force. This was confirmed by the comparable knee flexion force of the involved and non-involved knees at different flexion degrees and rotations.
The pes is often retracted during the posteromedial approach for surgical treatment of TPF with posteromedial involvement. Several past studies have shown the results of this method. Weil et al. [11] evaluated the outcomes of the posteromedial approach for the reduction and fixation of the medial (n = 10) and bicondylar (n = 17) TPF. After a mean follow-up of 3.5 years, 75% of patients had a good reduction. The average Oxford knee score was 19.9/48. The articular malreduction rate was 4%. No wound complications occurred. Manikandan and Saravanakumar [12] prospectively investigated the functional and radiological results of the posteromedial surgical approach to the knee in the treatment of twenty patients with complicated TPF and a posteromedial column fracture. Fractures were Schatzker type IV or more. All fractures were healed without complication. The postoperative anatomic reduction was achieved in 16 patients. The median knee range of flexion was 135°. The mean Oxford knee score was 29.3 (range 25–33). In comparison with earlier studies with pes retraction, we obtained a similar Average knee ROM. Likewise, we had no serious postoperative complications. While different functional measures were used (Oxford knee score vs. IKDC and KOOS), the knee function seems to be superior. This superiority could be attributed to the better fracture exposure achieved by the pes anserine detachment instead of its retraction. However, the patient’s and fracture’s characteristics are determining factors in the surgical outcomes and potentially could be the underlying cause of these inconsistent functional outcomes.
To the best of our knowledge, the present cohort was the first study reporting the outcomes of pes anserine release instead of retraction in the posteromedial approach of TPF surgery. Similar to any other study, this study was not without limitations. The main weakness of the research was the lack of a control group treated using a conventional posteromedial technique (pes anserine retraction). Manual evaluation of muscle strength is prone to bias. The small number of patients could be regarded as the other limitation of this study, which was posed by the concurrent COVID-19 pandemic and lack of patients’ cooperation to attend the final follow-up evaluation.
Conclusion
Pes anserine detachment in the posteromedial surgical approach to the knee in the treatment complex TPF with a posteromedial involvement provides a better fracture exposure. This modification seems to have no adverse effect on the functional outcomes of the patients. It does not affect the knee flexion strength. Besides, it is not associated with a particular postoperative complication. Future controlled studies with larger patients are required for better evaluation of the effect of the pes anserine detachment in TPF treatment.
References
Sament R, Mayanger JC, Tripathy SK, Sen RK (2012) Closed reduction and percutaneous screw fixation for tibial plateau fractures. J Orthop Surg (Hong Kong) 20(1):37–41. https://doi.org/10.1177/230949901202000108
Mankar SH, Golhar AV, Shukla M, Badwaik PS, Faizan M, Kalkotwar S (2012) Outcome of complex tibial plateau fractures treated with external fixator. Indian J Orthop 46(5):570–574. https://doi.org/10.4103/0019-5413.101041
Barei DP, Nork SE, Mills WJ, Coles CP, Henley MB, Benirschke SK (2006) Functional outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J Bone Joint Surg Am 88(8):1713–1721. https://doi.org/10.2106/jbjs.e.00907
Kandemir U, Maclean J (2014) Surgical approaches for tibial plateau fractures. J Knee Surg 27(1):21–29. https://doi.org/10.1055/s-0033-1363519
Rollick N, Wellman D (2018) Posterior approaches to the tibial plateau. Oper Tech Orthop 28(3):152–156. https://doi.org/10.1053/j.oto.2018.07.005
Murakami H, Soejima T, Inoue T, Kanazawa T, Noguchi K, Katouda M, Tabuchi K, Noyama M, Yasunaga H, Nagata K (2012) Inducement of semitendinosus tendon regeneration to the pes anserinus after its harvest for anterior cruciate ligament reconstruction-A new inducer grafting technique. Sports Med Arthrosc Rehabil Ther Technol 4(1):17. https://doi.org/10.1186/1758-2555-4-17
DiStefano V, Nixon J, O’Neil R, Davis O (1977) Pes anserinus transfer: an in vivo biomechanical analysis. Am J Sports Med 5(5):204–208
Kfuri M, Schatzker J (2018) Revisiting the Schatzker classification of tibial plateau fractures. Injury 49(12):2252–2263. https://doi.org/10.1016/j.injury.2018.11.010
Rahimi A, Nowrouzi A, Sohani SM (2013) The validity and reliability of the persian version of the international knee documentation committee (IKDC) questionnaire in Iranian patients after ACL and meniscal surgeries. Arch Rahabil 14(2):116–124
Saraei-Pour S, Salavati M, Akhbari B, Kazem-Nezhad A (2007) Translation and adaptation of knee injury and osteoarthritis outcome score (KOOS) in to persian and testing persian version reliability among Iranians with osteoarthritis. Arch Rahabil 8(1):42–46
Weil YA, Gardner MJ, Boraiah S, Helfet DL, Lorich DG (2008) Posteromedial supine approach for reduction and fixation of medial and bicondylar tibial plateau fractures. J Orthop Trauma 22(5):357–362. https://doi.org/10.1097/BOT.0b013e318168c72e
Manikandan N, Saravanakumar K (2019) A study on functional and radiological outcome of complex tibial plateau fractures by posteromedial plating. Int J Res Orthop 5(2):223–226
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Mahmud Jabalameli, Hooman Yahyazadeh, Abolfazl Bagherifard, Alireza Askari, Zahra Imani Pahlavanloo, and Mohsen Ostovar have no conflict of interest to declare.
Ethical statement
This study was approved by the review board of our institute under the code IR.IUMS.REC.1400.1252. Patients provided written consent before participation in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jabalameli, M., Yahyazadeh, H., Bagherifard, A. et al. Pes anserine detachment in posteromedial approach to the tibial plateau fracture provides better intraoperative exposure without compromising the flexor muscle strength. Eur J Orthop Surg Traumatol 33, 2399–2404 (2023). https://doi.org/10.1007/s00590-022-03447-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-022-03447-0