Abstract
Purpose
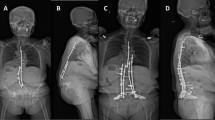
The primary aim of this study was to describe the feasibility, surgical approach window (SAW), and incision line (IL) for oblique lateral interbody fusion at L5-S1 (OLIF51) using computed tomography (CT). A secondary aim was to identify associations among approach characteristics and demographic and anthropometric factors.
Methods
We performed a radiographic study of 50 male and 50 female subjects who received abdominal CT imaging. SAW was measured as the distance from the midline to the medial border of the iliac vessel. IL was measured at the skin surface corresponding to the distance between the center of the disc space and SAW lateral margin. OLIF51 feasibility was defined as the existence of at least a 1-cm SAW without retraction of soft tissues.
Results
For the left side, the OLIF51 SAW and IL were 12.1 ± 4.6 and 175.1 ± 55.3 mm. For the right side, these measures were 10.0 ± 4.3 and 185.0 ± 52.5 mm. Correlations of r = 0.648 (p < 0.001) and r = 0.656 (p < 0.001) were observed between weight and IL on the left and right sides, respectively. OLIF51 was not feasible 23% of the time.
Conclusion
To our knowledge, this is the largest CT study to determine the feasibility of performing an OLIF51. Without the use of retraction, OLIF51 is not feasible 23% of the time. Left-sided OLIF51 allows for a larger surgical approach window and smaller incision compared to the right side. Larger incisions are required for adequate surgical exposure in patients with higher weight.





Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Mayer HM (1997) A new microsurgical technique for minimally invasive anterior lumbar interbody fusion. Spine (Phila Pa 1976) 22:691–9
Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ (2015) Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP LLIF and ALIF. J Spine Surg 1(1):2–18. https://doi.org/10.3978/j.issn.2414-469X.2015.10.05.PMID:27683674;PMCID:PMC5039869
Orita S, Shiga Y, Inage K et al (2020) Technical and conceptual review on the L5–S1 oblique lateral interbody fusion surgery (OLIF51). Spine Surg Relat Res 5(1):1–9. https://doi.org/10.22603/ssrr.2020-0086
Mobbs RJ, Phan K, Daly D et al (2015) Approach-related complications of anterior lumbar interbody fusion: results of a combined spine and vascular surgical team. Glob Spine J 6(2):147–154
Chung HW, Lee HD, Jeon CH, Chung NS (2021) Comparison of surgical outcomes between oblique lateral interbody fusion (OLIF) and anterior lumbar interbody fusion (ALIF). Clin Neurol Neurosurg 209:106901. https://doi.org/10.1016/j.clineuro.2021.106901. (Epub 2021 Aug 21 PMID: 34464832)
Kim JS, Choi WS, Sung JH (2016) 314 Minimally invasive oblique lateral interbody fusion for L4–5: clinical outcomes and perioperative complications—proquest. Neurosurgery 63(Suppl 1):190–191
Julian Li JX, Mobbs RJ, Phan K (2018) Morphometric MRI imaging study of the corridor for the oblique lumbar interbody fusion technique at L1–L5. World Neurosurg 111:e678–e685. https://doi.org/10.1016/j.wneu.2017.12.136
Zhang F, Xu H, Yin B et al (2017) Does right lateral decubitus position change retroperitoneal oblique corridor? A radiographic evaluation from L1 to L5. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 26(3):646–650. https://doi.org/10.1007/s00586-016-4645-7
Kim H, Chang BS, Chang SY (2022) Pearls and pitfalls of oblique lateral interbody fusion: a comprehensive narrative review. Neurospine 19(1):163–176. https://doi.org/10.14245/ns.2143236.618
Cooke RE Jr, Gaeta MG et al (2000) Picture archiving and communication systems. Health Devices 29(11):385–390
Tesoriero JA, Eddy P, Hasso AN (2015) PACS used while on-call: a national survey of radiology program directors and chief residents. J Digit Imaging 28(2):205–212. https://doi.org/10.1007/s10278-014-9741-9
Liu L, Liang Y, Zhang H, Wang H, Guo C, Pu X et al (2016) Imaging anatomical research on the operative windows of oblique lumbar interbody fusion. PLoS ONE 11(9):e0163452. https://doi.org/10.1371/journal.pone.0163452
Epic Systems (2023) Epic: about https://www.epic.com/about. Accessed 27 Jan 2023
Ratner B (2009) The correlation coefficient: Its values range between +1/−1, or do they? J Targ Meas Anal Mark 17(2):139–142. https://doi.org/10.1057/jt.2009.5
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86(2):420–428. https://doi.org/10.1037//0033-2909.86.2.420
Molinares DM, Davis TT, Fung DA (2016) Retroperitoneal oblique corridor to the L2–S1 intervertebral discs: an MRI study. J Neurosurg Spine 24(2):248–255. https://doi.org/10.3171/2015.3.SPINE13976. (Epub 2015 Oct 9 PMID: 26451662)
Davis TT, Hynes RA, Fung DA et al (2014) Retroperitoneal oblique corridor to the L2–S1 intervertebral discs in the lateral position: an anatomic study. J Neurosurg Spine 21(5):785–793. https://doi.org/10.3171/2014.7.SPINE13564
Wang K, Zhang C, Wu H, Chen Z, Chou D, Jian F (2019) The anatomic characteristics of the retroperitoneal oblique corridor to the L1–S1 intervertebral disc spaces. Spine (Phila Pa 1976) 44(12):E697–E706. https://doi.org/10.1097/BRS.0000000000002951
Woods KR, Billys JB, Hynes RA (2017) Technical description of oblique lateral interbody fusion at L1–L5 (OLIF25) and at L5–S1 (OLIF51) and evaluation of complication and fusion rates. Spine J 17(4):545–553. https://doi.org/10.1016/j.spinee.2016.10.026
Zairi F, Sunna TP, Westwick HJ et al (2017) Mini-open oblique lumbar interbody fusion (OLIF) approach for multi-level discectomy and fusion involving L5–S1: preliminary experience. Orthop Traumatol Surg Res 103(2):295–299. https://doi.org/10.1016/j.otsr.2016.11.016
Mun HY, Ko MJ, Kim YB, Park SW (2020) Usefulness of oblique lateral interbody fusion at L5–S1 level compared to transforaminal lumbar interbody fusion. J Korean Neurosurg Soc 63(6):723–729. https://doi.org/10.3340/jkns.2018.0215
Song SJ, Shin MH, Kim JT (2019) Anatomical feasibility of right oblique approach for L5–S1 oblique lumbar interbody fusion. World Neurosurg 132:e403–e408. https://doi.org/10.1016/j.wneu.2019.08.135
Deukmedjian AR, Le TV, Dakwar E, Martinez CR, Uribe JS (2012) Movement of abdominal structures on magnetic resonance imaging during positioning changes related to lateral lumbar spine surgery: a morphometric study: clinical article. J Neurosurg Spine 16(6):615–623. https://doi.org/10.3171/2012.3.SPINE1210
Gandhi SV, Dugan R, Farber SH, Godzik J, Alhilali L, Uribe JS (2022) Anatomical positional changes in the lateral lumbar interbody fusion. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 31(9):2220–2226. https://doi.org/10.1007/s00586-022-07195-x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors did not receive support from any organization for the submitted work. Dr. Cheng reports nonfinancial support from K2m during the conduct of the study; he also reports personal fees from Depuy (A Johnson & Johnson Company) and Alphatec Spine, and grants from Medtronic, K2M, Biomet, Ortho Fix, and NuVasive outside the submitted work. Dr. Danisa reports grants and personal fees from Globus Medical, grants from NuVasive, Medtronic, and Musculoskeletal Transplant Foundation outside the submitted work; he is affiliated with The Spine Journal, AAOS Medical Education Committee, and NASS Resident/Fellowship Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nayak, R., Razzouk, J., Ramos, O. et al. Oblique lateral interbody fusion at L5-S1: feasibility, surgical approach window, incision line, and influencing factors. Eur Spine J (2024). https://doi.org/10.1007/s00586-023-08017-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-023-08017-4