Abstract
Purpose
To determine the technical feasibility of uncinate process (UP) resection (uncinectomy) during anterior cervical approach with risk-avoidance of vertebral artery (VA) injury.
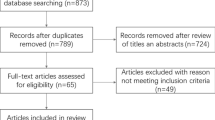
Methods
One hundred and seventy-six magnetic resonance imaging images with cervical spondylosis were evaluated. The diameter between UP and VA (UP–VA distance), the presence of a fat plane, and the VA's anterior–posterior position relative to UP (anterior[A], middle[M], posterior[P]) at C3-4 to C6-7 segments were investigated. Subsequently, easy-to-use classifications were developed according to the feasibility of total and partial uncinectomy. Total uncinectomy: easy (distance: > 2 mm); moderate (distance: ≤ 2 and fat plane: +); advanced (no fat plane). Partial uncinectomy: easy (distance: > 2 mm and P, A, or M position); moderate (distance: ≤ 2; fat plane: + and P position), and advanced (no fat plane and P position).
Results
UP-VA distance of C5-6 on the right side (left/right: 0.41/0.31 mm) was the smallest. The ratio of no fat plane of C5-6 (46.6%/49.4%) was the highest. C5-6 had a high rate of P position (7.4%/8.5%) while C6-7 had a high rate of A position (19.3%/18.2%). More than 90% individuals were classified as easy for partial uncinectomy at any vertebral segment (C3-7), while more than 30% were classified as advanced at C4-7 with the highest rate at C5-6 for total uncinectomy.
Conclusion
When performing uncinectomy during the anterior cervical approach, the C5-6 segment may be at the greatest risk of VA injury. Hence, preoperative MR images should be thoroughly evaluated to avoid VA injury.





Similar content being viewed by others
References
Montano N, Ricciardi L, Olivi A (2019) Comparison of anterior cervical decompression and fusion versus laminoplasty in the treatment of multilevel cervical spondylotic myelopathy: a meta-analysis of clinical and radiological outcomes. World Neurosurg 130:530-536.e532. https://doi.org/10.1016/j.wneu.2019.06.144
Katsuura Y, York PJ, Goto R, Yang J, Vaishnav AS, McAnany S, Albert T, Iyer S, Gang CH, Qureshi SA (2019) Sagittal reconstruction and clinical outcome using traditional ACDF, versus stand-alone ACDF versus TDR: a systematic review and quantitative analysis. Spine (Phila Pa 1976) 44:E1151–E1158. https://doi.org/10.1097/brs.0000000000003077
Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, Lee GP, Robinson JS, Jr. (2007) Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 32:2310–2317. doi: https://doi.org/10.1097/BRS.0b013e318154c57e
Guan Q, Chen L, Long Y, Xiang Z (2017) Iatrogenic vertebral artery injury during anterior cervical spine surgery: a systematic review. World Neurosurg 106:715–722. https://doi.org/10.1016/j.wneu.2017.07.027
Peng CW, Chou BT, Bendo JA, Spivak JM (2009) Vertebral artery injury in cervical spine surgery: anatomical considerations, management, and preventive measures. Spine J 9:70–76. https://doi.org/10.1016/j.spinee.2008.03.006
Lunardini DJ, Eskander MS, Even JL, Dunlap JT, Chen AF, Lee JY, Ward TW, Kang JD, Donaldson WF (2014) Vertebral artery injuries in cervical spine surgery. Spine J 14:1520–1525. https://doi.org/10.1016/j.spinee.2013.09.016
Neo M, Fujibayashi S, Miyata M, Takemoto M, Nakamura T (2008) Vertebral artery injury during cervical spine surgery: a survey of more than 5600 operations. Spine (Phila Pa 1976) 33:779–785. https://doi.org/10.1097/BRS.0b013e31816957a7
Segar AH, Riccio A, Smith M, Protopsaltis TS (2019) Total uncinectomy of the cervical spine with an osteotome: technical note and intraoperative video. J Neurosurg Spine:1–4. https://doi.org/10.3171/2019.6.Spine19332
Pakzaban P (2014) Ultrasonic total uncinectomy: a novel technique for complete anterior decompression of cervical nerve roots. Neurosurgery 10 Suppl 4:535–541; discussion 541. https://doi.org/10.1227/neu.0000000000000549
Safaee MM, Nichols NM, Yerneni K, Zhang Y, Riew KD, Tan LA (2020) Safety and efficacy of direct nerve root decompression via anterior cervical discectomy and fusion with uncinectomy for cervical radiculopathy. J Spine Surg 6:205–209
Ames CP, Smith JS, Scheer JK, Shaffrey CI, Lafage V, Deviren V, Moal B, Protopsaltis T, Mummaneni PV, Mundis GM Jr, Hostin R, Klineberg E, Burton DC, Hart R, Bess S, Schwab FJ (2013) A standardized nomenclature for cervical spine soft-tissue release and osteotomy for deformity correction: clinical article. J Neurosurg Spine 19:269–278. https://doi.org/10.3171/2013.5.Spine121067
Lee BH, Park JH, Lee JY, Jeon HJ, Park SW (2021) Efficiency of minimal oblique resection of the uncinate process during an anterior cervical discectomy and fusion. Medicine (Baltimore) 100:e26790. https://doi.org/10.1097/MD.0000000000026790
Ng JP, Scott-Young M, Chan DN, Oh JY (2021) The feasibility of anterior spinal access: the vascular corridor at the L5-S1 level for anterior lumbar interbody fusion. Spine (Phila Pa 1976) 46:983–989. https://doi.org/10.1097/brs.0000000000003948
Eskander MS, Drew JM, Aubin ME, Marvin J, Franklin PD, Eck JC, Patel N, Boyle K, Connolly PJ (2010) Vertebral artery anatomy: a review of two hundred fifty magnetic resonance imaging scans. Spine (Phila Pa 1976) 35:2035–2040. doi: https://doi.org/10.1097/BRS.0b013e3181c9f3d4
Belykh E, Xu DS, Yağmurlu K, Lei T, Byvaltsev VA, Dickman CA, Preul MC, Nakaji P (2017) Repair of V2 vertebral artery injuries sustained during anterior cervical diskectomy. World Neurosurg 105:796–804. https://doi.org/10.1016/j.wneu.2017.05.154
McHugh ML (2012) Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 22:276–282
Urbanschitz L, Merat S, Bensler S, Lenz CG, Mameghani AT, Eid K (2021) Cervical disc degeneration reduces distance between vertebral artery and surgical landmarks. Clin Neurol Neurosurg 200:106332. doi: https://doi.org/10.1016/j.clineuro.2020.106332
Lee HJ, Kim JH, Kim IS, Hong JT (2018) Anatomical evaluation of the vertebral artery (V2) and its influence in cervical spine surgery. Clin Neurol Neurosurg 174:80–85. https://doi.org/10.1016/j.clineuro.2018.09.002
Russo VM, Graziano F, Peris-Celda M, Russo A, Ulm AJ (2011) The V(2) segment of the vertebral artery: anatomical considerations and surgical implications. J Neurosurg Spine 15:610–619. https://doi.org/10.3171/2011.7.Spine1132
Güvençer M, Men S, Naderi S, Kiray A, Tetik S (2006) The V2 segment of the vertebral artery in anterior and anterolateral cervical spinal surgery: a cadaver angiographic study. Clin Neurol Neurosurg 108:440–445. https://doi.org/10.1016/j.clineuro.2005.04.006
Mihara H, Ohnari K, Hachiya M, Kondo S, Yamada K (2000) Cervical myelopathy caused by C3-C4 spondylosis in elderly patients: a radiographic analysis of pathogenesis. Spine (Phila Pa 1976) 25:796–800. https://doi.org/10.1097/00007632-200004010-00006
Huang T, Qin J, Zhong W, Tang K, Quan Z (2021) The CT assessment of uncovertebral joints degeneration in a healthy population. Eur J Med Res 26:145. https://doi.org/10.1186/s40001-021-00619-2
Tubbs RS, Rompala OJ, Verma K, Mortazavi MM, Benninger B, Loukas M, Chambers MR (2012) Analysis of the uncinate processes of the cervical spine: an anatomical study. J Neurosurg Spine 16:402–407. https://doi.org/10.3171/2011.12.SPINE11541
Acknowledgements
We appreciate the English proofreading of this manuscript by Editage (www.editage.com).
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No relevant financial activities outside the submitted work.
Ethical statement
This study was approved by the institutional ethics committee (R2901).
Patient consent
Written informed consent for the publication of clinical details and images was obtained from the patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shima, K., Shimizu, T., Fujibayashi, S. et al. Feasibility of total and partial uncinectomy during anterior cervical approach: MRI-based analysis of 176 patients regarding vertebral artery location. Eur Spine J 32, 3540–3546 (2023). https://doi.org/10.1007/s00586-023-07888-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07888-x