Abstract
Background
Vertebroplasty has been recently described in the literature as a potential treatment for C2 metastatic lesions. Stentoplasty may represent a safest and equally alternative to the latter.
Objective
To describe a novel technique, stentoplasty, as an alternative for the treatment of metastatic involvement of C2 and to assess its efficacy and safety. To systematically evaluate the pertinent literature regarding the clinical outcomes and complications of C2 vertebroplasty in patients with metastatic disease.
Methods
A systematic review of C2 vertebroplasty, in the English language medical literature was conducted for the needs of this study. Additionally, a cohort of five patients, presenting with cervical instability (SINS > 6) and/or severe pain (VAS > 6) from metastatic involvement of C2 and treated with stentoplasty in our department is presented. Outcomes evaluated include, pain control, stability, and complications.
Results
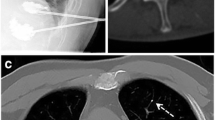
Our systematic review yielded 8 studies that met the inclusion criteria, incorporating 73 patients that underwent C2 vertebroplasty for metastatic disease. There was a reduction in VAS scores following surgery from 7.6 to 2.1. Eleven patients had complications (15%), 3 (4%) required additional stabilization and decompression, 6 (8.2%) had odynophagia and the incidence of cement leak was 31.5% (23/73). With regard to our cohort, all 5 patients presented with severe neck pain (average VAS 6.2 (2–10)) with or without instability (average SINS 10 (6–14)) and underwent C2 stentoplasty. Mean duration of the procedures was 90 min (61–145) and 2.6 mls (2–3) of cement was injected. Postoperatively VAS improved from 6.2 to 1.6 (P = 0.033). No cement leak or other complications were recorded.
Conclusion
A systematic review of the literature demonstrated that C2 vertebroplasty can offer significant pain improvement with a low complication rate. At the same time, this is the first study to describe stentoplasty in a small cohort of patients, as an alternative for the treatment of C2 metastatic lesions in selected cases, offering adequate pain control and improving segmental stability with a high safety profile.










Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author.
Code availability
Not applicable.
References
Jenis LG, Dunn EJ, An HS (1999) Metastatic disease of the cervical spine. Rev Clin Orthop Relat Res 359:89–103. https://doi.org/10.1097/00003086-199902000-00010
Sherk HH (1975) Lesions of the atlas and axis. Clin Orthop Relat Res 109:33–41. https://doi.org/10.1097/00003086-197506000-00005
Bilsky MH, Shannon FJ, Sheppard S, Prabhu V, Boland PJ (2002) Diagnosis and management of a metastatic tumor in the atlantoaxial spine. Spine 27(10):1062–9. https://doi.org/10.1097/00007632-200205150-00011
Vieweg U, Meyer B, Schramm J (2001) Tumour surgery of the upper cervical spine–a retrospective study of 13 cases. Acta Neurochir 143(3):217–225. https://doi.org/10.1007/s007010170101
Stangenberg M, Viezens L, Eicker SO, Mohme M, Mende KC, Dreimann M (2017) Cervical vertebroplasty for osteolytic metastases as a minimally invasive therapeutic option in oncological surgery: outcome in 14 cases. Neurosurg Focus 43(2):E3. https://doi.org/10.3171/2017.5.FOCUS17175
Anselmetti GC, Manca A, Montemurro F, Tutton S, Chiara G, Battistella M, Savojardo M, Marcia S, Masala S, Regge D (2012) Vertebroplasty using transoral approach in painful malignant involvement of the second cervical vertebra (C2): a single-institution series of 25 patients. Pain Phys 15(1):35–42
Galibert P, Deramond H, Rosat P, Le Gars D (1987) Note préliminaire sur le traitement des angiomes vertébraux par vertébroplastie acrylique percutanée [Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty]. Neurochirurgie 33(2):166–8
Pilitsis JG, Rengachary SS (2001) The role of vertebroplasty in metastatic spinal disease. Neurosurg Focus 11(6):e9. https://doi.org/10.3171/foc.2001.11.6.10
Weill A, Chiras J, Simon JM, Rose M, Sola-Martinez T, Enkaoua E (1996) Spinal metastases: indications for and results of percutaneous injection of acrylic surgical cement. Radiology 199(1):241–247. https://doi.org/10.1148/radiology.199.1.8633152
Patel AA, Vaccaro AR, Martyak GG, Harrop JS, Albert TJ, Ludwig SC, Youssef JA, Gelb DE, Mathews HH, Chapman JR, Chung EH, Grabowski G, Kuklo TR, Hilibrand AS, Anderson DG (2007) Neurologic deficit following percutaneous vertebral stabilization. Spine 32(16):1728–34. https://doi.org/10.1097/BRS.0b013e3180dc9c36
Floeth FW, Herdmann J, Rhee S, Turowski B, Krajewski K, Steiger HJ, Eicker SO (2014) Open microsurgical tumor excavation and vertebroplasty for metastatic destruction of the second cervical vertebra-outcome in seven cases. Spine J 14(12):3030–3037. https://doi.org/10.1016/j.spinee.2014.09.018
Martín-López JE, Pavón-Gómez MJ, Romero-Tabares A, Molina-López T (2015) Stentoplasty effectiveness and safety for the treatment of osteoporotic vertebral fractures: a systematic review. Orthop Traumatol Surg Res 101(5):627–632. https://doi.org/10.1016/j.otsr.2015.06.002
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA (2015) PRISMA-P group preferred reporting items for systematic review and meta-analysis protocols PRISMA-P statement. Syst Rev 4(1):1. https://doi.org/10.1186/2046-4053-4-1
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) (2021) Cochrane handbook for systematic reviews of interventions, Version 6.2. Cochrane, Oxford
Moulin B, Brisse H, Dutertre G, Brenet O, Queinnec M, Cottu P, Zadegan F, Moreau S, Benchimol R, Cao K, Servois V (2021) CT-guided vertebroplasty of first (C1) or second (C2) cervical vertebra using an electromagnetic navigation system and a transoral approach. Diagn Interv Imaging 102(9):571–575. https://doi.org/10.1016/j.diii.2021.04.007
Mont’Alverne F, Vallée JN, Cormier E, Guillevin R, Barragan H, Jean B, Rose M, Chiras J (2005) Percutaneous vertebroplasty for metastatic involvement of the axis. AJNR Am J Neuroradiol 26(7):1641–1645
Sun G, Jin P, Li M, Liu X, Li F, Yu AK, Lu Y (2010) Percutaneous vertebroplasty for treatment of osteolytic metastases of the C2 vertebral body using anterolateral and posterolateral approach. Technol Cancer Res Treat 9(4):417–422. https://doi.org/10.1177/153303461000900411
Wang KW, Wang HK, Lu K, Liang CL, Chen YW, Liliang PC (2016) Fluoroscopically guided C2 percutaneous vertebroplasty: a surgical technique note on an anterior ascending approach. Pain Phys 19(4):E625–E629
Rhiew R, Manjila S, Dezure A, Tabbosha M, Guthikonda M, Eltahawy H (2008) Minimally invasive anterior vertebroplasty for C-2 metastatic lesions. Neurosurg Focus 25(2):E4. https://doi.org/10.3171/FOC/2008/25/8/E4
Ishii T, Mukai Y, Hosono N, Sakaura H, Nakajima Y, Sato Y, Sugamoto K, Yoshikawa H (2004) Kinematics of the upper cervical spine in rotation: in vivo three-dimensional analysis. Spine 29(7):E139-44. https://doi.org/10.1097/01.brs.0000116998.55056.3c
Vender JR, McDonnell DE (2001) Management of lesions involving the craniocervical junction. Neurosurg Q 11(2):151–171. https://doi.org/10.1097/00013414-200106000-00007
Fourney DR, York JE, Cohen ZR, Suki D, Rhines LD, Gokaslan ZL (2003) Management of atlantoaxial metastases with posterior occipitocervical stabilization. J Neurosurg 98(2 Suppl):165–170. https://doi.org/10.3171/spi.2003.98.2.0165
Delank KS, Wendtner C, Eich HT, Eysel P (2011) The treatment of spinal metastases. Dtsch Arztebl Int 108(5):71–9. https://doi.org/10.3238/arztebl.2011.0071
Gilbert HA, Kagan AR, Nussbaum H, Rao AR, Satzman J, Chan P, Allen B, Forsythe A (1977) Evaluation of radiation therapy for bone metastases: pain relief and quality of life. AJR Am J Roentgenol 129(6):1095–1096. https://doi.org/10.2214/ajr.129.6.1095
Willert HG, Enderle A (1979) Temporäre zementplombe bei knochentumoren fraglicher dignität [temporary plugging of cystic bone tumors by bone cement (author’s transl)]. Z Orthop Ihre Grenzgeb. 117(2):224–32
Nelson DA, Barker ME, Hamlin BH (1997) Thermal effects of acrylic cementation at bone tumour sites. Int J Hyperth 13(3):287–306. https://doi.org/10.3109/02656739709023537
Reddy AS, Hochman M, Loh S, Rachlin J, Li J, Hirsch JA (2005) CT guided direct transoral approach to C2 for percutaneous vertebroplasty. Pain Phys 8(2):235–238
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
MT contributed to the study conception and design. Data collection and analysis were performed by EN and AM. The first draft of the manuscript was written by EN and all authors commented on previous versions of the manuscript. Final version of the article reviewed by MT, EN, and SK.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no competing interests. No financial support was provided for this study, and no potential conflict of interest or associated biases were present from any of the authors.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Najjar, E., Rampersad, R., Komaitis, S. et al. C2 stentoplasty: an alternative to conventional vertebroplasty in the treatment of axis metastatic lesions: a systematic review with meta-analysis and case series. Eur Spine J 32, 3450–3462 (2023). https://doi.org/10.1007/s00586-023-07809-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07809-y