Abstract
Purpose
To share long-term clinical outcomes and our experience with full-endoscopic interlaminar decompression (FEI) for lateral recess stenosis (LRS).
Methods
We included all patients who underwent FEI for LRS from 2009 to 2013. VAS for leg pain, ODI, neurological findings, radiographic findings, and complications were analyzed at one week, one month, three months, and one year postoperation. The telephone interview for local patients with simple questions was done approximately ten years after the operation. International patients receive an email with the same questionnaire as local patients during the same follow-up period.
Results
One hundred and twenty-nine patients underwent FEI for LRS with complete data during 2009–2013. Most of the patients (70.54%) had LRS radiculopathy for less than one year, mainly L4-5 (89.92%), followed by L5-S1 (17.83%). Early outcomes three months after surgery showed that most patients (93.02%) reported significant pain relief, and 70.54% reported no pain at their ODI scores were significantly reduced from 34.35 to 20.32% (p = 0.0052). In contrast, the mean VAS for leg pain decreased substantially by 3.77 points (p < 0.0001). There were no severe complications. At ten years of follow-up, 62 patients responded to the phone call or email. 69.35% of the patients reported having little or no back or leg pain, did not receive any further lumbar surgery, and were still satisfied with the result of the surgery. There were six patients (8.06%) who underwent reoperation.
Conclusion
FEI for LRS was satisfactory at 93.02%, with a low complication rate during the early follow-up period. Its effect seems to decline slightly in the long term at a 10-year follow-up. 8.06% of the patients subsequently underwent reoperation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lateral recess stenosis is a common form of spinal stenosis. Its main characteristics are degeneration of the surrounding structures, from the intervertebral disc to the facet joint and the ligamentum flavum. Sciatica is the most common presentation, which can be initially managed with medications and physical therapy [1, 2]. When conservative treatments fail in some patients with severe stenosis and/or motor weakness, surgical management to free the nerve from compression by surrounding structures is essential [1, 2].
To date, there is no consensus on surgical technique for lateral recess stenosis [3,4,5,6,7,8]. The most widely used approach is a microscope-assisted partial facetectomy. Other techniques include lumbar fusion, as well as laser-assisted [9] and full-endoscopic [10, 11] decompression, which showed less tissue traumatization, shorter surgery duration, and better patient acceptance [12].
Full-endoscopic interlaminar decompression (FEI) for lateral recess stenosis (LRS) uses a 7.9-mm-diameter probe that contains a working channel of 4.2 mm inside with a 25-degree angled lens at the tip of the probe [12]. All surgical instruments are used through this working channel. The decompression can be done using an interlaminar approach. High-speed burr and cutting instruments cut the bone and ligament that compress the nerve. Continuous irrigation with water and a 25-degree angle lens allows the surgeon to have a clear vision of the nerve and surrounding tissue.
The early evidence was based on a prospective, randomized, controlled study conducted in Germany [11]. Of 161 patients, 95% reported a significant improvement in improvement in pain [11], comparable to the conventional technique, but with less operative time, surgical complications, postoperative pain level, and analgesic requirement [11]. However, the steep learning curve of this technique must be noted [12,13,14,15].
Long-term studies that use the same technique have not yet been conducted. Using our database, this study aimed to share long-term clinical outcomes and reoperation rates.
Materials and methods
Our local institutional review board approved the study. One hundred and twenty-nine patients were treated with FEI for LRS during 2009–2013. Study variables such as the Oswestry Disability Index (ODI), Visual Analog Scale (VAS), neurological findings, and complications of all patients with complete records were analyzed.
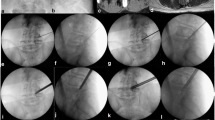
The clinical and imaging criteria for offering FEI for LRS at our institution are radicular symptoms for more than three months without improvement with a conservative approach or weakness of the muscle supplied by the entrapped nerve root without apparent spinal instability in the flexion and extension films. MRI of the lumbar spine showed lateral recess stenosis with nerve root compression. This procedure was not offered to patients with gross spinal instability or predominant mechanical back pain. All patients have unilateral radicular symptoms. Those with bilateral leg symptoms of central canal stenosis will be studied in another study (Figs. 1 and 2).
Both patients and clinicians measured clinical outcomes. The patient's leg and back pain self-assessment was performed using VAS and ODI in the clinic before the patient met with their doctors. Neurological functions were assessed by clinicians who may or may not participate in the study. Our institute is an international hospital serving both local patients and international patients who fly in for treatment and fly out after treatment is over. The follow-up examination was performed one week, one month, three months, and one year after the operation. International patients received an online questionnaire by email during the same follow-up period. At approximately ten years after surgery (mean follow-up duration 10.05 years (95%CI 9.79–10.32)), 66 local patients received a telephone interview, while 63 international patients received an email with a questionnaire containing the same set of questions as the telephone interview. For simplicity, we asked whether they currently have leg or back pain, whether the pain disturbs their quality of life, and whether they have undergone further fusion or decompression surgery in the lumbar spine or not, if not already indicated in medical records.
Surgical technique and instruments
-
1.
Instruments
We used the Vertebris endoscope set from Richard-Wolf GmBH, Germany. The endoscope is a 7.9-mm single portal with a working channel and two channels for the fiber optic lens and the water irrigation system. The lens is at a 25-degree angle to facilitate viewing of the area inside the spinal canal. The water outflow is five times more than the inflow. This feature prevents the accumulation of water inside the spinal canal.
-
2.
Patient positioning
After general anesthesia, the patient is positioned prone on a flexible surgical table or a Jackson table to facilitate positioning. Care is taken to avoid compression of the abdominal organs, eyes, and bony prominences.
-
3.
Operating theatre setting
The surgeon and the assistants stand on the ipsilateral side of the decompression with the endoscope workstation and the C-arm on the opposite side. We always stand on a raised platform to make our stance and shoulder as relaxed as possible.
-
4.
Soft tissue preparation
The interlaminar window of the indexed level is verified with a C arm. A small incision in the skin is made slightly lateral to the midline. A blunt probe is used to dissect the soft tissue down to the level of the ligamentum flavum before the working sleeve, and the endoscope is introduced, respectively. Soft tissue and muscle are removed to identify bony structures, such as the descending facet, ascending facet, and caudal and cranial lamina. The clear view of these structures gives us an idea of the extent of the decompression.
-
5.
Bone work
For effective and safe bone resection, the tip of the burr should be visible at all times. Various drills are available and can be chosen according to the specific situation. Among all types, we most frequently use the oval-shaped burr. Smooth bone resection surfaces facilitate hemostasis of cancellous bone, particularly the lamina. Periodic fluoroscopy can be performed to check the extent of decompression. In cases of severe facet hypertrophy, thinning the ascending facet with a drill before using the Kerrison Rongeur provides additional safety. This minimizes the chance of nerve injury from the foot plate of the Kerrison Rongeur. To determine adequate bone resection without inducing spinal instability, we recommend resecting only a few millimeters of the descending facet, enough to expose the medial aspect of the ascending facet’s tip. This is where the deep layer of the ligamentum flavum inserts into the ascending facet and is also the usual location of the shoulder of the traversing nerve root.
-
6.
Flavum resection
In the case of thick ligamentum flavum, endoscope rotation can provide an additional viewing angle to the undersea neural structures. The flavum and ascending facet is removed to enlarge the lateral recess until the nerve is free from compression and pulsates along with water irrigation.
-
7.
Adequate nerve decompression
We must see the nerve from its shoulder along its path to the lower pedicle to ensure adequate decompression.
-
8.
How to avoid complications
To avoid a dura tear, the tip of any instrument must be always seen before cutting. Create a safe dissection plane using a blunt probe to avoid pulling the dura when cutting the flavum. Keep the surgical field free of too many bleeding points. Minimal bleeding in endoscopic surgery does not cause problems for the patient but can make the surgical area cloudy and unpleasant.
-
9.
Postoperative care
Patients can walk as soon as they return to the ward and are discharged the following morning. Rehabilitation is scheduled as an outpatient as needed. The antibiotic is given only once, 30–60 min before surgery. Pain medications are prescribed at the patient's request.
Results
Demographics of the patients and clinical characteristics
One hundred twenty-nine patients underwent FED for LRS. The mean age of the patients was 58.47 years (95%CI 56.21–60.72), and 48.84% were men. They were generally overweight (mean BMI 27.23; 95%CI 26.36–28.09). Most of the patients (70.54%) had radiculopathy of LRS for less than one year, mainly from L4-5 (89.92%), followed by L5-S1 (17.83%) (Table 1). The average operation time was 82.50 min (95%CI 70.52–94.48). Of 129, there are 113 cases of single-level decompression and 16 cases of two-level decompression (Table 2). There were 66 local patients and 63 international patients who flew in to receive the treatment and returned when it ended. All patients had MRI findings of LRS (i.e., thickened ligamentum flavum, facet arthrosis, disc desiccation). Eleven out of 129 cases had a stable grade 1 spondylolisthesis (8.52%).
Clinical outcomes
Of 129 patients receiving FEI for LRS with complete data, 93.02% reported significant pain relief, and 70.54% reported no pain. All patients could stand and walk immediately after the anesthesia effect wore off, and 97.67% stayed in the hospital for less than 24 h. At month three after surgery, their ODI scores were significantly reduced from 34.35 to 20.32% (p = 0.0052), while the mean VAS for leg pain decreased significantly by 3.77 points (p < 0.0001). No patients demonstrated worsening motor weakness. One case reported temporary numbness after surgery. The incidental durotomy encountered in one case was treated conservatively with bed rest. No neurological sequelae were observed during the 2-year clinical follow-up (Table 3).
Sixty-three patients responded to telephone follow-ups or emails approximately ten years after surgery (Table 4). 69.35% of the patients (43/62) reported having no or occasional leg and back pain that did not affect their quality of life. They had not undergone any lumbar surgery since their first surgery. A patient passed away four years after the surgery at 96 due to unrelated matters to a spinal condition. There were six reoperations (Table 5), four of which were fusion. Two of the fusion cases had progression of spondylolisthesis at two years and five years (Fig. 3). One did it due to residual radicular symptoms. One had a disc herniation at the operating level 9 months after the first surgery. Two patients received another decompression at another hospital. One did it a few months and another four years after the first surgery.
Discussion
Few studies reported long-term outcomes of minimally invasive decompression for spinal stenosis with a follow-up of more than ten years [16]. Most long-term studies followed the patient for 2—5 years [17,18,19,20,21]. To our knowledge, this study is the first study to report long-term outcomes of full-endoscopic uniportal decompression for lateral recess stenosis with a mean follow-up period of 10 years.
The initial results showed favorable results with a low complication rate (Tables 5 and 6). Most patients reported having no leg pain, and ODI and VAS scores dropped significantly at the initial follow-up. The advantages of FEI-LRS include fewer tissue traumatizations, a short hospital stay, and results comparable to the standard microsurgical technique [11]. Our institute is an international hospital that serves both domestic and international patients. The international patients flew in for treatment and returned home after treatment. Clinical follow-up is challenging for this group as they rarely respond to follow-up emails or phone calls. We saw this as an opportunity to develop a new platform to collect data from these patients for future research and to improve the quality of care. Although our sample size is relatively small, approximately two-thirds of the patients reported having little or no back or leg pain for a very long time and were still satisfied with the results.
The reoperation rate in our group is similar to the previous rate reported in other long-term studies [22,23,24,25,26,27]. Two out of 4 cases who underwent fusion surgery underwent it because there was the progression of the spondylolisthesis. Radicular and back pain recurred after two years in one case and after five years in another. On the other hand, out of the 8 cases that were documented for stable grade 1 spondylolisthesis and responded to the follow-up call at ten years, six patients reported having little or no back or leg pain and still had a good quality of life. We selectively perform postoperative scans on individuals who experience back pain or leg pain. We diagnose postoperative spinal instability if the patient develops new mechanical back pain after the FEI-LRS procedure. Similar to most spinal conditions, the patient will undergo a period of conservative treatment and will opt for surgical stabilization only if conservative measures prove unsuccessful. Although many long-term studies showed promising results from decompression without fusion in a group of lumbar stenosis with stable spondylolisthesis [22,23,24,25,26,27], more studies with a minimum follow-up period of 10 years could be needed to confirm this finding. One case had a new herniated disc after a traumatic event. Since it happened at the decompressed segment, we offered him a fusion even without spondylolisthesis. Two patients received another decompression surgery a few months and four years after the first surgery at another institute. These two patients did not return to our institute for investigations when pain recurred. This, again, is another challenge in developing a systematic and proactive follow-up measure for quality improvement.
Conclusions
FEI for LRS is an effective procedure for patients with predominant unilateral radicular symptoms. Its benefit can be seen through the 10-year follow-up. A systematic and proactive follow-up strategy should be developed for international patients to increase the follow-up rate.
References
Tadokoro K, Miyamoto H, Sumi M, Shimomura T (2005) The prognosis of conservative treatments for lumbar spinal stenosis: analysis of patients over 70 years of age. Spine 30:2458–2463. https://doi.org/10.1097/01.brs.0000184692.71897.a2
Amundsen T, Weber H, Nordal HJ, Magnaes B, Abdelnoor M, Lilleas F (2000) Lumbar spinal stenosis: conservative or surgical management?: a prospective 10-year study. Spine 25:1424–1435. https://doi.org/10.1097/00007632-200006010-00016
Kambin P, Casey K, O’Brien E, Zhou L (1996) Transforaminal arthroscopic decompression of lateral recess stenosis. J Neurosurg 84:462–467. https://doi.org/10.3171/jns.1996.84.3.0462
Knight MT, Goswami A, Patko JT, Buxton N (2001) Endoscopic foraminoplasty: a prospective study on 250 consecutive patients with independent evaluation. J Clin Laser Med Surg 19:73–81. https://doi.org/10.1089/104454701750285395
Ahn Y, Lee SH, Park WM, Lee HY (2003) Posterolateral percutaneous endoscopic lumbar foraminotomy for L5–S1 foraminal or lateral exit zone stenosis. Technical note J Neurosurg 99:320–323. https://doi.org/10.3171/spi.2003.99.3.0320
Haufe SM, Mork AR (2007) Effects of unilateral endoscopic facetectomy on spinal stability. J Spinal Disord Tech 20:146–148. https://doi.org/10.1097/01.bsd.0000211256.05626.6b
Haufe SM, Baker RA, Pyne ML (2009) Endoscopic thoracic laminoforaminoplasty for the treatment of thoracic radiculopathy: report of 12 cases. Int J Med Sci 6:224–226. https://doi.org/10.7150/ijms.6.224
Haufe SM, Mork AR, Pyne MA, Baker RA (2009) Endoscopic laminoforaminoplasty success rates for treatment of foraminal spinal stenosis: report on sixty-four cases. Int J Med Sci 6:102–105. https://doi.org/10.7150/ijms.6.102
Knight MT, Vajda A, Jakab GV, Awan S (1998) Endoscopic laser foraminoplasty on the lumbar spine–early experience. Minim Invasive Neurosurg 41:5–9. https://doi.org/10.1055/s-2008-1052006
Schubert M, Hoogland T (2005) Endoscopic transforaminal nucleotomy with foraminoplasty for lumbar disk herniation. Oper Orthop Traumatol 17:641–661. https://doi.org/10.1007/s00064-005-1156-9
Ruetten S, Komp M, Merk H, Godolias G (2009) Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study. J Neurosurg Spine 10:476–485. https://doi.org/10.3171/2008.7.17634
Ruetten S, Komp M, Merk H, Godolias G (2008) Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine 33:931–939. https://doi.org/10.1097/BRS.0b013e31816c8af7
Kuonsongtum V, Paiboonsirijit S, Kesornsak W, Chaiyosboorana V, Rukskul P, Chumnanvej S, Ruetten S (2009) Result of full endoscopic uniportal lumbar discectomy: preliminary report. J Med Assoc Thai 92:776–780
Chumnanvej S, Kesornsak W, Sarnvivad P, Paiboonsirijit S, Kuansongthum V (2011) Full endoscopic lumbar discectomy via interlaminar approach: 2-year results in Ramathibodi Hospital. J Med Assoc Thai 94:1465–1470
Wang B, Lu G, Patel AA, Ren P, Cheng I (2011) An evaluation of the learning curve for a complex surgical technique: the full endoscopic interlaminar approach for lumbar disc herniations. Spine J 11:122–130. https://doi.org/10.1016/j.spinee.2010.12.006
Aihara T, Endo K, Suzuki H, Kojima A, Sawaji Y, Urushibara M, Matsuoka Y, Takamatsu T, Murata K, Konishi T, Yamauchi H, Endo H, Yamamoto K (2021) Long-term outcomes following lumbar microendoscopic decompression for lumbar spinal stenosis with and without degenerative spondylolisthesis: minimum 10-year follow-up. World Neurosurg 146:e1219–e1225. https://doi.org/10.1016/j.wneu.2020.11.131
Mekhail N, Costandi S, Nageeb G, Ekladios C, Saied O (2021) The durability of minimally invasive lumbar decompression procedure in patients with symptomatic lumbar spinal stenosis: long-term follow-up. Pain Pract 21:826–835. https://doi.org/10.1111/papr.13020
Regev GJ, Leor G, Ankori R, Hochberg U, Ofir D, Khashan M, Kedem R, Lidar Z, Salame K (2021) Long-term pain characteristics and management following minimally invasive spinal decompression and open laminectomy and fusion for spinal stenosis. Medicina (Kaunas). https://doi.org/10.3390/medicina57101125
Rompe JD, Eysel P, Zollner J, Nafe B, Heine J (1999) Degenerative lumbar spinal stenosis. Long-term results after undercutting decompression compared with decompressive laminectomy alone or with instrumented fusion. Neurosurg Rev 22:102–106. https://doi.org/10.1007/s101430050040
Scholler K, Steingruber T, Stein M, Vogt N, Muller T, Pons-Kuhnemann J, Uhl E (2016) Microsurgical unilateral laminotomy for decompression of lumbar spinal stenosis: long-term results and predictive factors. Acta Neurochir (Wien) 158:1103–1113. https://doi.org/10.1007/s00701-016-2804-6
Yuce I, Kahyaoglu O, Cavusoglu HA, Cavusoglu H, Aydin Y (2019) Long-term clinical outcome and reoperation rate for microsurgical bilateral decompression via unilateral approach of lumbar spinal stenosis. World Neurosurg 125:e465–e472. https://doi.org/10.1016/j.wneu.2019.01.105
Austevoll IM, Hermansen E, Fagerland MW, Storheim K, Brox JI, Solberg T, Rekeland F, Franssen E, Weber C, Brisby H, Grundnes O, Algaard KRH, Boker T, Banitalebi H, Indrekvam K, Hellum C, Investigators N-D (2021) Decompression with or without fusion in degenerative lumbar spondylolisthesis. N Engl J Med 385:526–538. https://doi.org/10.1056/NEJMoa2100990
Bovonratwet P, Samuel AM, Mok JK, Vaishnav AS, Morse KW, Song J, Steinhaus ME, Jordan YJ, Gang CH, Qureshi SA (2022) Minimally invasive lumbar decompression versus minimally invasive transforaminal lumbar interbody fusion for treatment of low-grade lumbar degenerative spondylolisthesis. Spine 47:1505–1514. https://doi.org/10.1097/BRS.0000000000004432
Ghogawala Z, Dziura J, Butler WE, Dai F, Terrin N, Magge SN, Coumans JV, Harrington JF, Amin-Hanjani S, Schwartz JS, Sonntag VK, Barker FG 2nd, Benzel EC (2016) Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med 374:1424–1434. https://doi.org/10.1056/NEJMoa1508788
Shen Z, Guan X, Wang R, Xue Q, Zhang D, Zong Y, Ma W, Zhuge R, Liu Z, He C, Guo L, Yin F (2022) Effectiveness and safety of decompression alone versus decompression plus fusion for lumbar spinal stenosis with degenerative spondylolisthesis: a systematic review and meta-analysis. Ann Transl Med 10:664. https://doi.org/10.21037/atm-22-2208
Wang M, Luo XJ, Ye YJ, Zhang Z (2019) Does concomitant degenerative spondylolisthesis influence the outcome of decompression alone in degenerative lumbar spinal stenosis? A meta-analysis of comparative studies. World Neurosurg 123:226–238. https://doi.org/10.1016/j.wneu.2018.11.246
Wei FL, Zhou CP, Gao QY, Du MR, Gao HR, Zhu KL, Li T, Qian JX, Yan XD (2022) Decompression alone or decompression and fusion in degenerative lumbar spondylolisthesis. EClinicalMedicine 51:101559. https://doi.org/10.1016/j.eclinm.2022.101559
Author information
Authors and Affiliations
Contributions
WK and VK initiated the study. KMML and WK collected and analyzed data. KP helped to analyze data and drafted the manuscript. All authors helped to draft and approve the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kesornsak, W., Kuansongtham, V., Lwin, K.M.M. et al. Pain improvement and reoperation rate after full-endoscopic decompression for lateral recess stenosis: a 10-year follow-up. Eur Spine J 32, 2882–2888 (2023). https://doi.org/10.1007/s00586-023-07801-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07801-6