Abstract
Background
Metastatic epidural spinal cord compression (MESCC) is a debilitating sequela of cancer that results in pain, disability, and neurologic deficits. Surgical techniques have included open surgical (OS) techniques with anterior and/or posterior decompression and fusion procedures. Further technical evolution has led to minimally invasive spinal (MIS) decompression and fusion. The objective of this study is to compare MIS to OS techniques in the treatment of thoracolumbar MESCC.
Methods
A review of the literature was performed using PubMed database. Inclusion criteria included patients 18 years or older, thoracolumbar MESCC, and surgeries with instrumented fusion. A total of 451 articles met the inclusion criteria and further analysis narrowed them down to 81 articles. Variables collected included blood loss, length of stay, operative time, pre- and postoperative Frankel grade, and complications.
Results
A total of 5726 papers were collected, with a total of 81 papers meeting final inclusion criteria: 26 papers with MIS technique and 55 with OS. A total of 2267 patients were evaluated. They were split into three surgical subtypes of MIS and OS: posterior decompression and fusion, partial corpectomy, and complete corpectomy. Overall, MIS had lower operative time, blood loss, and complications compared to OS. A timeline analysis showed reduction of complication rates in MIS surgery between papers published over a 28-year period.
Conclusion
MESCC carries significant morbidity and mortality. Surgical approaches for palliative treatment should account for this fact. We conclude that MIS techniques offer a viable alternative to traditional OS approaches with lower overall morbidity and complications.



Similar content being viewed by others
References
Klimo P Jr, Schmidt MH (2004) Surgical management of spinal metastases. Oncol 9:188–196. https://doi.org/10.1634/theoncologist.9-2-188
Wong DA, Fornasier VL, MacNab I (1990) Spinal metastases: the obvious, the occult, and the impostors. Spine 15:1–4
Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, Mohiuddin M, Young B (2005) Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet 366:643–648. https://doi.org/10.1016/S0140-6736(05)66954-1
Liu A, Sankey EW, Goodwin CR, Kosztowski TA, Elder BD, Bydon A, Witham TF, Wolinsky JP, Gokaslan ZL, Sciubba DM (2016) Postoperative survival and functional outcomes for patients with metastatic gynecological cancer to the spine: case series and review of the literature. J Neurosurg Spine 24:131–144. https://doi.org/10.3171/2015.3.SPINE15145
Kan P, Schmidt MH (2008) Minimally invasive thoracoscopic approach for anterior decompression and stabilization of metastatic spine disease. Neurosurg Focus 25:E8. https://doi.org/10.3171/FOC/2008/25/8/E8
Kumar N, Malhotra R, Maharajan K, Zaw AS, Wu PH, Makandura MC, Po Liu GK, Thambiah J, Wong HK (2017) Metastatic spine tumor surgery: a comparative study of minimally invasive approach using percutaneous pedicle screws fixation versus open approach. Clin Spine Surg 30:E1015–E1021. https://doi.org/10.1097/BSD.0000000000000400
Lu DC, Chou D, Mummaneni PV (2011) A comparison of mini-open and open approaches for resection of thoracolumbar intradural spinal tumors. J Neurosurg Spine 14:758–764. https://doi.org/10.3171/2011.1.SPINE09860
Uribe JS, Dakwar E, Le TV, Christian G, Serrano S, Smith WD (2010) Minimally invasive surgery treatment for thoracic spine tumor removal: a mini-open, lateral approach. Spine 35:S347–S354. https://doi.org/10.1097/BRS.0b013e3182022d0f
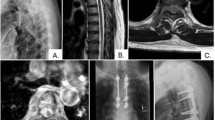
Alshareef MA, Klapthor G, Lowe SR, Barley J, Cachia D, Frankel BM (2020) Strategies for posterior-only minimally invasive surgery in thoracolumbar metastatic epidural spinal cord compression. Surg Neurol Int 11:462. https://doi.org/10.25259/SNI_815_2020
Molina CA, Gokaslan ZL, Sciubba DM (2011) A systematic review of the current role of minimally invasive spine surgery in the management of metastatic spine disease. Int J Surg Oncol 2011:598148. https://doi.org/10.1155/2011/598148
Tokuhashi Y, Uei H, Oshima M, Ajiro Y (2014) Scoring system for prediction of metastatic spine tumor prognosis. World J Orthop 5:262–271. https://doi.org/10.5312/wjo.v5.i3.262
Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T (2001) Surgical strategy for spinal metastases. Spine 26:298–306. https://doi.org/10.1097/00007632-200102010-00016
Binning MJ, Gottfried ON, Klimo P Jr, Schmidt MH (2004) Minimally invasive treatments for metastatic tumors of the spine. Neurosurg Clin N Am. 15:459–465. https://doi.org/10.1016/j.nec.2004.04.010
Keshavarzi S, Park MS, Aryan HE, Newman CB, Amene CS, Gonda D, Taylor WR (2009) Minimally invasive thoracic corpectomy and anterior fusion in a patient with metastatic disease: case report and review of the literature. Minim Invasive Neurosurg 52:141–143. https://doi.org/10.1055/s-0029-1231067
Regan JJ, Yuan H, McAfee PC (1999) Laparoscopic fusion of the lumbar spine: minimally invasive spine surgery. a prospective multicenter study evaluating open and laparoscopic lumbar fusion. Spine 24:402–411. https://doi.org/10.1097/00007632-199902150-00023
Regan JJ, Aronoff RJ, Ohnmeiss DD, Sengupta DK (1999) Laparoscopic approach to L4–L5 for interbody fusion using BAK cages: experience in the first 58 cases. Spine 24:2171–2174. https://doi.org/10.1097/00007632-199910150-00018
Katoh H, Yamashita K, Kokuba Y, Satoh T, Ozawa H, Hatate K, Ihara A, Nakamura T, Onosato W, Watanabe M (2008) Surgical resection of stage IV colorectal cancer and prognosis. World J Surg 32:1130–1137. https://doi.org/10.1007/s00268-008-9535-7
Paulino Pereira NR, Janssen SJ, van Dijk E, Harris MB, Hornicek FJ, Ferrone ML, Schwab JH (2016) Development of a prognostic survival algorithm for patients with metastatic spine disease. J Bone Jt Surg 98:1767–1776. https://doi.org/10.2106/JBJS.15.00975
Funding
There was no funding received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Frankel receives royalties from Orthofix and Stryker.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alshareef, M., Klapthor, G., Alawieh, A. et al. Evaluation of open and minimally invasive spinal surgery for the treatment of thoracolumbar metastatic epidural spinal cord compression: a systematic review. Eur Spine J 30, 2906–2914 (2021). https://doi.org/10.1007/s00586-021-06880-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06880-7