Abstract
Purpose
The purpose of this study was to find out additional indications for multi-positional MRI in cervical degenerative spondylosis (CDS) patients.
Material and methods
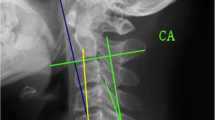
A total of 63 patients with cervical spondylotic myelopathy that underwent multi-positional MRI and X-ray were included. Muhle’s grade, C2-7 angle, and C7 slope were measured. Patients were assigned to the stenosis group (Group S) when Muhle’s grades were increased by more than two or maximum grade was reached. Other patients were assigned to the maintenance group (Group M). Receiver operating characteristic (ROC) analysis was performed. Statistical significance was accepted for p values of < 0.05.
Results
A total of 24 patients were assigned to the S group and 39 patients to the M group. Mean C2-7 angle difference in extension (eC27A) between S and M groups was 10.97° (p = 0.002). The mean inter-group difference between C2-7 angle in extension and neutral positions (e-nC27A) was 14.39° (p = 0.000). Mean C7 slope difference in neutral position was − 6.53° (p = 0.002). Based on areas under ROC curves (AUCs), e-nC27A, eC27A, and negative C7 slope had AUCs of 0.934 (95% CI 0.876–0.992), 0.752 (95% CI 0.624–0.880), and 0.720 (95% CI 0.588–0.851), respectively. The optimal cutoff value of e-nC27A was 15.4 degrees, which had a diagnostic accuracy of 88.9%.
Conclusion
Multi-positional MRI helps to find dynamic cord compressive lesion in CDS patients. The higher eC27A, e-nC27A values and smaller C7 slope were found to increase the likelihood of cervical dynamic stenosis. Among other factors, we recommend multi-positional MRI before surgery especially when a patient’s e-nC27A is > 15.4 degrees.
Level of evidence I
Diagnostic: individual cross-sectional studies with the consistently applied reference standard and blinding.






Similar content being viewed by others
References
Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG (2015) Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine 40:E675-693. https://doi.org/10.1097/brs.0000000000000913
Lee HJ, Kim IS, Sung JH, Lee SW, Hong JT (2016) Significance of multimodal intraoperative monitoring for the posterior cervical spine surgery. ClinNeurolNeurosurg 143:9–14. https://doi.org/10.1016/j.clineuro.2016.02.007
Kim JY, Kwon JY, Kim MS, Lee JJ, Kim IS, Hong JT (2018) Comparison of morphological characteristics of the subaxial cervical spine between athetoid cerebral palsy and normal control. J Korean NeurosurgSoc 61:243–250. https://doi.org/10.3340/jkns.2017.0303.011
Lee HJ, Kim JH, Kim IS, Hong JT (2018) Anatomical evaluation of the vertebral artery (V2) and its influence in cervical spine surgery. ClinNeurolNeurosurg 174:80–85. https://doi.org/10.1016/j.clineuro.2018.09.002
Lee HJ, Kim JH, Kim IS, Hong JT (2019) Physiologic cervical alignment change between whole spine radiographs and normal standing cervical radiographs. World Neurosurg 122:e1222–e1227. https://doi.org/10.1016/j.wneu.2018.11.019
Lee JB, Kim IS, Kwon JY, Lee JJ, Park JH, Cho CB, Yang SH, Sung JH, Hong JT (2018) Difference of dynamic morphometric changes between in patients with ossification of posterior longitudinal ligament and patients with cervical spondylosis: assessment by cervical dynamic magnetic resonance imaging. World Neurosurg. https://doi.org/10.1016/j.wneu.2018.11.213
Nigro L, Donnarumma P, Tarantino R, Rullo M, Santoro A, Delfini R (2017) Static and dynamic cervical MRI: two useful exams in cervical myelopathy. J Spine Surg 3:212–216. https://doi.org/10.21037/jss.2017.06.01
Hong JT, Sung JH, Son BC, Lee SW, Park CK (2008) Significance of laminar screw fixation in the subaxial cervical spine. Spine 33:1739–1743. https://doi.org/10.1097/BRS.0b013e31817d2aa2
Hong JT, Kim IS, Kim JY, Lee HJ, Kwon JY, Kim MS, Sung JH (2016) Risk factor analysis and decision-making of surgical strategy for V3 segment anomaly: significance of preoperative CT angiography for posterior C1 instrumentation. Spine J 16:1055–1061. https://doi.org/10.1016/j.spinee.2016.04.019
Kim IS, Hong JT, Lee JJ, Lee JB, Cho CB, Yang SH, Sung JH (2018) A novel technique for cervical laminoplasty fusion: simultaneously enhancing stabilization and decompression in various cervical myelopathies: a technical note and outcomes. World Neurosurg 111:361–366. https://doi.org/10.1016/j.wneu.2018.01.018
Kim IS, Hong JT, Jang WY, Yang SH, Sung JH, Son BC, Lee SW (2011) Surgical treatment of osodontoideum. J ClinNeurosci 18:481–484. https://doi.org/10.1016/j.jocn.2010.07.114
Muhle C, Metzner J, Weinert D, Falliner A, Brinkmann G, Mehdorn MH, Heller M, Resnick D (1998) Classification system based on kinematic MR imaging in cervical spondylitic myelopathy. AJNR Am J Neuroradiol 19:1763–1771
Hyun SJ, Kim KJ, Jahng TA, Kim HJ (2016) Relationship between T1 slope and cervical alignment following multilevel posterior cervical fusion surgery: impact of T1 slope minus cervical lordosis. Spine 41:E396-402. https://doi.org/10.1097/brs.0000000000001264
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36. https://doi.org/10.1148/radiology.143.1.7063747
Simundic AM (2009) Measures of diagnostic accuracy: basic definitions. Ejifcc 19:203–211
Nagata K, Yoshimura N, Hashizume H, Muraki S, Ishimoto Y, Yamada H, Takiguchi N, Nakagawa Y, Minamide A, Oka H, Kawaguchi H, Nakamura K, Akune T, Yoshida M (2014) The prevalence of cervical myelopathy among subjects with narrow cervical spinal canal in a population-based magnetic resonance imaging study: the Wakayama Spine Study. Spine J 14:2811–2817. https://doi.org/10.1016/j.spinee.2014.03.051
Lee JB, Kim IS, Kwon JY, Lee JJ, Park JH, Cho CB, Yang SH, Sung JH, Hong JT (2019) Difference of dynamic morphometric changes between in patients with ossification of posterior longitudinal ligament and patients with cervical spondylosis: assessment by cervical dynamic magnetic resonance imaging. World Neurosurg 123:e566–e573. https://doi.org/10.1016/j.wneu.2018.11.213
Tykocki T, du Plessis J, Wynne-Jones G (2018) Correlation between the severity of myelopathy and cervical morphometric parameters on dynamic magnetic resonance imaging. ActaNeurochir (Wien) 160:1251–1258. https://doi.org/10.1007/s00701-018-3540-x
Kolcun JP, Chieng LO, Madhavan K, Wang MY (2017) The role of dynamic magnetic resonance imaging in cervical spondylotic myelopathy. Asian Spine J 11:1008–1015. https://doi.org/10.4184/asj.2017.11.6.1008
Badhiwala JH, Wilson JR (2018) The Natural history of degenerative cervical myelopathy. NeurosurgClin N Am 29:21–32. https://doi.org/10.1016/j.nec.2017.09.002
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, J.B., Park, J.H., Lee, J.J. et al. Influence of dynamic neck motion on the clinical usefulness of multi-positional MRI in cervical degenerative spondylosis. Eur Spine J 30, 1542–1550 (2021). https://doi.org/10.1007/s00586-021-06760-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06760-0