Abstract
Purpose
Instrumentation of the lumbar spine is a common procedure for treating pathologic conditions. Studies have revealed the risks of pathologies in the adjacent segments, with the incidence rate being up to 36.1%. Revision procedures are often required, including extension of the instrumentation by the use of connectors to adjacent levels. The aim of this study was to determine the stiffness of side-to-side and end-to-end connectors for comparison with the use of continuous rods.
Methods
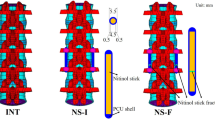
Ten human lumbar spine specimens (L1–S1) were tested about the three axes under pure moment loading of ± 7.5 Nm. Nine conditions were used to investigate the functions of the extensions for different instrumentation lengths (L3–S1 and L2–S1) and different connector levels (L3/4 and L2/3). The intersegmental range of motion (iROM) and intersegmental neutral zone as well as total range of motion (tROM) and total neutral zone (tNZ) were analyzed.
Results
The application of the spinal system significantly decreased the tROMs (− 44 to − 83%) and iROMs in levels L2/3 (− 56 to − 94%) and L3/4 (− 68 to − 99%) in all the tested directions, and the tNZ under flexion/extension (− 63 to − 71%) and axial rotation (− 34 to − 72%). These decreases were independent of the employed configuration (p < 0.05). The only significant changes in the iROM were observed under lateral bending between the continuous rod and the side-to-side connector at level L3/4 (p = 0.006).
Conclusion
From a biomechanical viewpoint, the tested connectors are comparable to continuous rods in terms of ROM and NZ.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.








Similar content being viewed by others
References
Chow DHK, Luk KDK, Evans JH, Leong JCY (1996) Effects of short anterior lumbar interbody fusion on biomechanics of neighboring unfused segments. Spine (Phila Pa 1976) 21:549–555. https://doi.org/10.1097/00007632-199603010-00004
Herkowitz HN, Abraham DJ, Todd JA (1999) Management of degenerative disc disease above an L5–Sl segment requiring arthrodesis. Spine (Phila Pa 1976) 24:1268–1270
Kim YE, Goel VK, Weinstein JN, Lim TH (1991) Effect of disc degeneration at one level on the adjacent level in axial mode. Spine (Phila Pa 1976) 16:331–335
Phillips FM, Reuben J, Wetzel FT (2002) Intervertebral disc degeneration adjacent to a lumbar fusion: an experimental rabbit model. J Bone Joint Surg Br 84:289–294
Weinhoffer SL, Guyer RD, Herbert M, Griffith SL (1995) Intradiscal pressure measurements above an instrumented fusion: a cadaveric study. Spine (Phila Pa 1976) 20:526–531
Ha K-Y, Son J-M, Im J-H, Oh I-S (2013) Risk factors for adjacent segment degeneration after surgical correction of degenerative lumbar scoliosis. Indian J Orthop 47:346–351. https://doi.org/10.4103/0019-5413.114912
Park P, Garton HJ, Gala VC et al (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 29:1938–1944. https://doi.org/10.1097/01.brs.0000137069.88904.03
Wilke H, Wenger K, Claes L (1998) Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur Spine J 7:148–154
Crawford NR, Dickman CA (1997) Construction of local vertebral coordinate systems using a digitizing probe. Technical note. Spine (Phila Pa 1976) 22:559–563. https://doi.org/10.1097/00007632-199703010-00020
Panjabi MM (1988) Biomechanical evaluation of spinal fixation devices: I. A conceptual framework. Spine (Phila Pa 1976) 13:1129–1134
Volkheimer D, Malakoutian M, Oxland TR, Wilke H-J (2015) Limitations of current in vitro test protocols for investigation of instrumented adjacent segment biomechanics: critical analysis of the literature. Eur Spine J 24:1882–1892. https://doi.org/10.1007/s00586-015-4040-9
Wilke HH-J, Wenger K, Claes L (1998) Testing criteria tor spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur Spine J 7:148–154
Burkus JK, Foley K, Haid R, LeHuec J-C (2001) Surgical Interbody Research Group—radiographic assessment of interbody fusion devices: fusion criteria for anterior lumbar interbody surgery. Neurosurg Focus 10:1–9. https://doi.org/10.3171/foc.2001.10.4.12
Booth KC, Bridwell KH, Eisenberg BA et al (1999) Minimum 5-year results of degenerative spondylolisthesis treated with decompression and instrumented posterior fusion. Spine (Phila Pa 1976) 24:1721–1727
Frymoyer JW, Hanley EN, Howe J et al (1979) A comparison of radiographic findings in fusion and nonfusion patients ten or more years following lumbar disc surgery. Spine (Phila Pa 1976) 4:435–440
Ghiselli G, Wang JC, Bhatia NN et al (2004) Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am 86-A:1497–1503
Kanayama M, Hashimoto T, Shigenobu K et al (2001) Adjacent-segment morbidity after Graf ligamentoplasty compared with posterolateral lumbar fusion. J Neurosurg 95:5–10
Tinetti M, Kumar C (2010) The patient who falls:“It’s always a trade-off”. JAMA 303:258–266. https://doi.org/10.1001/jama.2009.2024.The
Kuslich SD, Danielson G, Dowdle JD et al (2000) Four-year follow-up results of lumbar spine arthrodesis using the Bagby and Kuslich lumbar fusion cage. Spine (Phila Pa 1976) 25:2656–2662
Guigui P, Lambert P, Lassale B, Deburge A (1997) Long-term outcome at adjacent levels of lumbar arthrodesis. Rev Chir Orthop Reparatrice Appar Mot 83:685–696
Ren C, Song Y, Liu L, Xue Y (2014) Adjacent segment degeneration and disease after lumbar fusion compared with motion-preserving procedures: a meta-analysis. Eur J Orthop Surg Traumatol 24:245–253. https://doi.org/10.1007/s00590-014-1445-9
Sears WR, Sergides IG, Kazemi N et al (2011) Incidence and prevalence of surgery at segments adjacent to a previous posterior lumbar arthrodesis. Spine J 11:11–20. https://doi.org/10.1016/j.spinee.2010.09.026
Keck J, Krüger S, Rauschmann M et al. (2016) Biomechanical comparison of different rod-to-rod connectors to a conventional rod system. Eur Spine J 25(11):3792. https://doi.org/10.1007/s00586-016-4801-0
Scheer JK, Tang JA, Deviren V et al (2011) Biomechanical analysis of revision strategies for rod fracture in pedicle subtraction osteotomy. Neurosurgery 69:164–172. https://doi.org/10.1227/NEU.0b013e31820f362a
Senatus P, Chinthakunta SR, Vazifeh P, Khalil S (2013) Biomechanical evaluation of a novel posterior integrated clamp that attaches to an existing posterior instrumentation for use in thoracolumbar revision. Asian Spine J 7:1–7. https://doi.org/10.4184/asj.2013.7.1.1
Penta M, Sandhu A, Fraser RD (1995) Magnetic resonance imaging assessment of disc degeneration 10 years after anterior lumbar interbody fusion. Spine (Phila Pa 1976) 20:743–747
Wai EK, Santos ERG, Morcom RA, Fraser RD (2006) Magnetic resonance imaging 20 years after anterior lumbar interbody fusion. Spine (Phila Pa 1976) 31:1952–1956. https://doi.org/10.1097/01.brs.0000228849.37321.a8
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 4:190–194. https://doi.org/10.1016/j.spinee.2004.07.007
Lund T, Oxland TR (2011) Adjacent level disk disease—is it really a fusion disease? Orthop Clin North Am 42:529–541. https://doi.org/10.1016/j.ocl.2011.07.006
Malakoutian M, Volkheimer D, Street J et al (2015) Do in vivo kinematic studies provide insight into adjacent segment degeneration? A qualitative systematic literature review. Eur Spine J 24:1865–1881. https://doi.org/10.1007/s00586-015-3992-0
Smith JS, Shaffrey CI, Ames CP et al (2012) Assessment of symptomatic rod fracture after posterior instrumented fusion for adult spinal deformity. Neurosurgery 71:862–867. https://doi.org/10.1227/NEU.0b013e3182672aab
Panjabi MM (2007) Hybrid multidirectional test method to evaluate spinal adjacent-level effects. Clin Biomech 22:257–265. https://doi.org/10.1016/j.clinbiomech.2006.08.006
Crawford NR (2007) Does the “hybrid multidirectional test method” generate quality data or paradoxical data? Clin Biomech (Bristol, Avon). https://doi.org/10.1016/j.clinbiomech.2007.04.005
Panjabi M (2007) Reply. Clin Biomech 22:863–864. https://doi.org/10.1016/j.clinbiomech.2007.04.001
Acknowledgements
The authors thank Medtronic Inc. for providing the implants and instrumentations used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Welke, B., Schwarze, M., Hurschler, C. et al. In vitro investigation of two connector types for continuous rod construct to extend lumbar spinal instrumentation. Eur Spine J 27, 1895–1904 (2018). https://doi.org/10.1007/s00586-018-5664-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5664-3