Abstract
Purpose
Propofol is commonly used to induce general anesthesia; however, the pain caused during propofol injection is a disadvantage. This study aimed to assess whether deep breathing attenuates propofol injection pain.
Methods
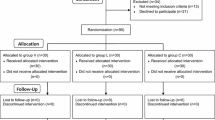
This prospective, single-blind, randomized controlled study included 200 patients who were scheduled to undergo elective surgery under general anesthesia and randomly and equally divided them into group D and group C. The observers were not blinded to the pain-relieving modality, but each patient was blinded. Group D patients were requested to repeatedly take deep breaths throughout general anesthesia induction with propofol. Group C patients were requested to breathe in the usual manner. The intensity of propofol injection pain was evaluated using the visual analog scale (VAS). Furthermore, we recorded the patients’ pain expressions, including grimace or hand-withdrawal, and the recalled pain measured using a VAS in the post-anesthetic care units (PACU).
Results
Compared with patients in group C, those in group D showed significantly reduced VAS scores for propofol injection pain (20 [interquartile range (IQR): 0–48] vs. 37 [IQR 9–65], P = 0.017) and recalled pain in the PACU (16 [IQR 0–32] vs. 26 [IQR 0.5–51], P = 0.031). Further, the grimace incidence was significantly lower in group D (18%) than in group C (45%) (P < 0.001). There was no significant difference in the incidence of pain at induction, recalled pain, or hand-withdrawal.
Conclusions
Deep breathing could be an easy, safe, and inexpensive method for reducing pain during propofol injection.



Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Picard P, Tramer MR. Prevention of pain on injection with propofol: a quantitative systematic review. Anesth Analg. 2000;90:963–9.
Macario A, Weinger M, Truong P, Lee M. Which clinical anesthesia outcomes are both common and important to avoid? The perspective of a panel of expert anesthesiologists. Anesth Analg. 1999;88:1085–91.
Desousa KA. Pain on propofol injection: causes and remedies. Indian J Pharmacol. 2016;48:617–23.
Kwak HJ, Min SK, Kim JS, Kim JY. Prevention of propofol-induced pain in children: combination of alfentanil and lidocaine vs alfentanil or lidocaine alone. Br J Anaesth. 2009;103:410–2.
King SY, Davis FM, Wells JE, Murchison DJ, Pryor PJ. Lidocaine for the prevention of pain due to injection of propofol. Anesth Analg. 1992;74:246–9.
Lee P, Russell WJ. Preventing pain on injection of propofol: A comparison between lignocaine pre-treatment and lignocaine added to propofol. Anaesth Intensive Care. 2004;32:482–4.
Aouad MT, Siddik-Sayyid SM, Al-Alami AA, Baraka AS. Multimodal analgesia to prevent propofol-induced pain: pretreatment with remifentanil and lidocaine versus remifentanil or lidocaine alone. Anesth Analg. 2007;104:1540–4.
Bennett Joel A, Abrams Jonathan T, Van Riper DF, Horrow JC. Difficult or impossible ventilation after sufentanil-induced anesthesia is caused primarily by vocal cord closure. Anesthesiology. 1997;87:1070–4.
Kim KO, Chung S, Lee K, Cho H. Profound bradycardia with lidocaine during anesthesia induction in a silent sick sinus syndrome patient. J Clin Anesth. 2011;23:227–30.
Jalota L, Kalira V, George E, Shi YY, Hornuss C, Radke O, Pace NL, Apfel CC. Prevention of pain on injection of propofol: systematic review and meta-analysis. BMJ. 2011;342: d1110.
McCrirrick A, Hunter S. Pain on injection of propofol: the effect of injectate temperature. Anaesthesia. 1990;45:443–4.
Hwang LK, Nash DW, Yedlin A, Greige N, Larios-Valencia J, Choice C, Pothula A. The effect of vibration on pain during intravenous injection of propofol: a randomized controlled trial. Ann Plast Surg. 2021;87:S36–9.
Kumar S, Khuba S, Agarwal A, Gautam S, Yadav M, Dixit A. Evaluation of efficacy of valsalva maneuver for attenuating propofol injection pain: a prospective, randomized, single blind, placebo controlled study. Korean J Anesthesiol. 2018;71:453–8.
Simkin P, Bolding A. Update on nonpharmacologic approaches to relieve labor pain and prevent suffering. J Midwifery Womens Health. 2004;49:489–504.
Taddio A, Appleton M, Bortolussi R, Chambers C, Dubey V, Halperin S, Hanrahan A, Ipp M, Lockett D, MacDonald N, Midmer D, Mousmanis P, Palda V, Pielak K, Riddell RP, Rieder M, Scott J, Shah V. Reducing the pain of childhood vaccination: an evidence-based clinical practice guideline. CMAJ. 2010;182:E843–55.
French GM, Painter EC, Coury DL. Blowing away shot pain: a technique for pain management during immunization. Pediatrics. 1994;93:384–8.
Busch V, Magerl W, Kern U, Haas J, Hajak G, Eichhammer P. The effect of deep and slow breathing on pain perception, autonomic activity, and mood processing—an experimental study. Pain Med. 2012;13:215–28.
Helander EM, Menard BL, Harmon CM, Homra BK, Allain AV, Bordelon GJ, Wyche MQ, Padnos IW, Lavrova A, Kaye AD. Multimodal analgesia, current concepts, and acute pain considerations. Curr Pain Headache Rep. 2017;21:3.
Chalaye P, Goffaux P, Lafrenaye S, Marchand S. Respiratory effects on experimental heat pain and cardiac activity. Pain Med. 2009;10:1334–40.
Jafari H, Courtois I, Van den Bergh O, Vlaeyen JWS, Van Diest I. Pain and respiration: a systematic review. Pain. 2017;158:995–1006.
Matta JA, Cornett PM, Miyares RL, Abe K, Sahibzada N, Ahern GP. General anesthetics activate a nociceptive ion channel to enhance pain and inflammation. Proc Natl Acad Sci USA. 2008;105:8784–9.
Earley S. Trpa1 channels in the vasculature. Br J Pharmacol. 2012;167:13–22.
Nilius B, Appendino G, Owsianik G. The transient receptor potential channel trpa1: from gene to pathophysiology. Pflugers Arch. 2012;464:425–58.
Scott RPF, Saunders DA, Norman J. Propofol: Clinical strategies for preventing the pain of injection. Anaesthesia. 1988;43:492–4.
Zamboni P, Menegatti E, Pomidori L, Morovic S, Taibi A, Malagoni AM, Cogo AL, Gambaccini M. Does thoracic pump influence the cerebral venous return? J Appl Physiol. 2012;112:904–10.
Cohen LL. Behavioral approaches to anxiety and pain management for pediatric venous access. Pediatrics. 2008;122:S134–9.
Kleiber C, Harper DC. Effects of distraction on children’s pain and distress during medical procedures: a meta-analysis. Nurs Res. 1999;48:44–9.
Nishimura RA, Tajik AJ. The valsalva maneuver and response revisited. Mayo Clin Proc. 1986;61:211–7.
Nimmagadda U, Chiravuri SD, Ramez Salem M, Joseph NJ, Wafai Y, Crystal GJ, El-Orbany MI. Preoxygenation with tidal volume and deep breathing techniques: the impact of duration of breathing and fresh gas flow. Anesth Analg. 2001;92:1337–41.
Marhofer P. Regional blocks carried out during general anesthesia or deep sedation: myths and facts. Curr Opin Anaesthesiol. 2017;30:621–6.
Wang W, Wu L, Zhang C, Sun L. Is propofol injection pain really important to patients? BMC Anesthesiol. 2017;17:24.
Dedic A, Adam S, Gommers D, Van Bommel J. Propofol injection pain: Is it still an issue? The effect of premedication. Minerva Anestesiol. 2010;76:720–4.
Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med. 2001;8:1153–7.
Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Breivik Hals EK, Kvarstein G, Stubhaug A. Assessment of pain. Br J Anaesth. 2008;101:17–24.
Agarwal A, Ansari MF, Gupta D, Pandey R, Raza M, Singh PK, Shiopriye DS, Singh U. Pretreatment with thiopental for prevention of pain associated with propofol injection. Anesth Analg. 2004;98:683–6.
Fedorov V, Mannino F, Zhang R. Consequences of dichotomization. Pharm Stat. 2009;8:50–61.
Singh A, Sharma G, Gupta R, Kumari A, Tikko D. Efficacy of tramadol and butorphanol pretreatment in reducing pain on propofol injection: a placebo-controlled randomized study. J Anaesthesiol Clin Pharmacol. 2016;32:89–93.
Moon YE, Lee MY, Kim DH. Preventive effect of a vapocoolant spray on propofol-induced pain: a prospective, double-blind, randomized study. J Anesth. 2017;31:703–8.
Lee JR, Jung CW, Lee YH. Reduction of pain during induction with target-controlled propofol and remifentanil. Br J Anaesth. 2007;99:876–80.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Contributions
KT: methodology, validation, formal analysis, data curation, writing—original draft, project administration. YY: conceptualization, data curation, visualization, writing—review and editing. TH: investigation, data curation, visualization, writing—review and editing. KN: validation, writing—review and editing, supervision. TM: validation, writing—review and editing, supervision. All authors were involved in the study design and data interpretation. All authors revised the manuscript, approved the manuscript for publication, and agree to be accountable for all aspects of the work in ensuring that the questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Tanaka, K., Yoshizumi, Y., Hamada, T. et al. Deep breathing alleviates propofol-induced pain: a prospective, randomized, single-blind study. J Anesth 37, 97–103 (2023). https://doi.org/10.1007/s00540-022-03136-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-022-03136-6