Abstract
Introduction
The end-expiratory occlusion test (EEOT) may predict the response to fluid administration in patients undergoing lung-protective ventilation, but arterial catheter insertion is necessary to evaluate changes in stroke volume (SV). The peripheral perfusion index is a potential noninvasive alternative to evaluate SV. The aim of this study is to investigate whether changes in perfusion index during an intraoperative EEOT can predict the response to fluid administration in patients undergoing lung-protective ventilation (tidal volume 7 ml/kg predicted body weight).
Methods
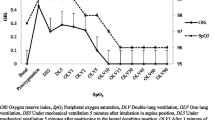
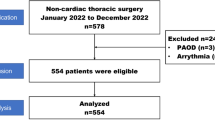
Forty-one elective surgical patients were enrolled. The SV and perfusion index were recorded before (baseline), during a 40-s EEOT and after volume expansion (250 ml of lactated Ringer’s solution over 10 min). Patients with an increase in SV greater than 10% after volume expansion were defined as responders. ΔPI (change in perfusion index between baseline and 20 (ΔPI20) or 40 s (ΔPI40) after the beginning of EEOT were calculated using: ΔPI20 (%) = [(PI at 20 s after EEOT beginning − PIbaseline)/PIbaseline] × 100, ΔPI40 (%) = [(PI at 40 s after EEO beginning − PIbaseline)/PIbaseline] × 100).
Results
Sixteen patients were responders, and 25 were non-responders. The area under the receiver operating characteristics curves generated for ΔPI20 and ΔPI40 to predict response to a fluid challenge were 0.561 (95% CI 0.374–0.749) and 0.688 (95% CI 0.523–0.852), respectively.
Conclusion
Changes in perfusion index during intraoperative EEOT in patients undergoing lung-protective ventilation (7 ml/kg) were unable to predict the response to fluid administration.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Change history
02 December 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00540-022-03147-3
References
Nisanevich V, Felsenstein I, Almogy G, Weissman C, Einav S, Matot I. Effect of intraoperative fluid management on outcome after intraabdominal surgery. Anesthesiology. 2005;103:25–32.
Chappell D, Jacob M, Hofmann-Kiefer K, Conzen P, Rehm M. A rational approach to perioperative fluid management. Anesthesiology. 2008;109:723–40.
Perel A. Using dynamic variables to guide perioperative fluid management. Anesthesiology. 2020;133:929–93.
Monnet X, Marik PE, Teboul JL. Prediction of fluid responsiveness: an update. Ann Intensive Care. 2016. https://doi.org/10.1186/s13613-016-0216-7.
Marik PE, Cavallazzi R, Vasu T, Hirani A. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med. 2009;37:2642–7.
Monnet X, Osman D, Ridel C, Lamia B, Richard C, Teboul JL. Predicting volume responsiveness by using the end-expiratory occlusion in mechanically ventilated intensive care unit patients. Crit Care Med. 2009;37:951–6.
Gavelli F, Teboul JL, Monnet X. The end-expiratory occlusion test: please, let me hold your breath! Crit Care. 2019. https://doi.org/10.1186/s13054-019-2554-y.
Gavelli F, Shi R, Teboul JL, Azzolina D, Monnet X. The end-expiratory occlusion test for detecting preload responsiveness: a systematic review and meta-analysis. Ann Intensive Care. 2020. https://doi.org/10.1186/s13613-020-00682-8.
Young CC, Harris EM, Vacchiano C, Bodnar S, Bukowy B, Elliott RRD, Migliarese J, Ragains C, Trethewey B, Woodward A, de Abreu GM, Girard M, Futier E, Mulier JP, Pelosi P, Sprung J. Lung-protective ventilation for the surgical patient: international expert panel-based consensus recommendations. Br J Anaesth. 2019;123:898–913.
Myatra SN, Prabu NR, Divatia JV, Monnet X, Kulkarni AP, Teboul JL. The changes in pulse pressure variation or stroke volume variation after a “tidal volume challenge” reliably predict fluid responsiveness during low tidal volume ventilation. Crit Care Med. 2017;45:415–21.
Biais M, Larghi M, Henriot J, de Courson H, Sesay M, Nouette-Gaulain K. End-expiratory occlusion test predicts fluid responsiveness in patients with protective ventilation in the operating room. Anesth Analg. 2017;125:1889–95.
Georges D, de Courson H, Lanchon R, Sesay M, Nouette-Gaulain K, Biais M. End-expiratory occlusion maneuver to predict fluid responsiveness in the intensive care unit: an echocardiographic study. Crit Care. 2018. https://doi.org/10.1186/s13054-017-1938-0.
Beurton A, Teboul JL, Gavelli F, Gonzalez FA, Girotto V, Galarza L, Anguel N, Richard C, Monnet X. The effects of passive leg raising may be detected by the plethysmographic oxygen saturation signal in critically ill patients. Crit Care. 2019. https://doi.org/10.1186/s13054-019-2306-z.
Lima AP, Beelen P, Bakker J. Use of a peripheral perfusion index derived from the pulse oximetry signal as a noninvasive indicator of perfusion. Crit Care Med. 2002;30:1210–3.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Weil G, Motamed C, Monnet X, Eghiaian A, Le Maho AL. End-expiratory occlusion test to predict fluid responsiveness is not suitable for laparotomic surgery. Anesth Analg. 2020;130:151–8.
van Lavieren M, Veelenturf J, Hofhuizen C, van der Kolk M, van der Hoeven J, Pickkers P, Lemson J, Lansdorp B. Dynamic preload indicators decrease when the abdomen is opened. BMC Anesthesiol. 2014. https://doi.org/10.1186/1471-2253-14-90.
Jozwiak M, Depret F, Teboul JL, Alphonsine JE, Lai C, Richard C, Monnet X. Predicting fluid responsiveness in critically ill patients by using combined end-expiratory and end-inspiratory occlusions with echocardiography. Crit Care Med. 2017;45:e1131–8.
Messina A, Montagnini C, Cammarota G, De Rosa S, Giuliani F, Muratore L, Della Corte F, Navalesi P, Cecconi M. Tidal volume challenge to predict fluid responsiveness in the operating room: an observational study. Eur J Anaesthesiol. 2019;36:583–91.
Biais M, Lanchon R, Sesay M, Le Gall L, Pereira B, Futier E, Nouette-Gaulain K. Changes in stroke volume induced by lung recruitment maneuver predict fluid responsiveness in mechanically ventilated patients in the operating room. Anesthesiology. 2017;126:260–7.
Ryu KH, Hwang SH, Shim JG, Ahn JH, Cho EA, Lee SH, Byun JH. Comparison of vasodilatory properties between desflurane and sevoflurane using perfusion index: a randomised controlled trial. Br J Anaesth. 2020;125:935–42.
Funding
This study was not financed.
Author information
Authors and Affiliations
Contributions
YI and MS contributed to the conception and design of the study. YI and MS analyzed the data and wrote the manuscript. YI, YO, KY and TN helped with the data collection. MS and AL revised the manuscript critically. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
This study was approved by the institutional Review Board (S20-042). Participants were obtained written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Iizuka, Y., Sanui, M., Otsuka, Y. et al. Changes in peripheral perfusion index during intraoperative end-expiratory occlusion tests do not predict the response to fluid administration in patients undergoing lung protective ventilation. J Anesth 35, 837–843 (2021). https://doi.org/10.1007/s00540-021-02988-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-021-02988-8