Abstract
Purpose
Hemodynamic management during low central venous pressure (L-CVP)-assisted hepatectomy involves fluid restriction during resection and fluid resuscitation after resection. Recently, high stroke volume variation (SVV) has been reported as an alternative to L-CVP for reducing blood loss during a hepatectomy. The current study evaluated the impact of a newly implemented SVV-based goal-directed therapy (GDT) protocol on blood loss during hepatectomy.
Methods
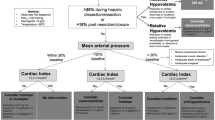
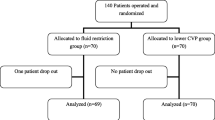
We conducted a before–after comparative study, which included L-CVP-assisted hepatectomy cases (control group) and GDT-assisted hepatectomy cases (intervention group). The GDT protocol included SVV, cardiac index, and mean arterial pressure as hemodynamic parameters. The target SVV ranges were ≥ 13% and ≤ 12% before and after the resection, respectively. The primary endpoint was the proportion of patients whose blood loss was < 400 mL (median of our hepatectomy cases) in the GDT group, and it was compared to a predefined threshold of 50%. We also investigated factors associated with blood loss using multiple regression analysis.
Results
We included 66 patients in the control group and 50 in the GDT group. In the GDT group, the median blood loss was 220 mL and 36 patients (72%) lost < 400 mL blood. This was significantly greater than 50% (P < 0.001). Post-resection GDT-guided fluid optimization reduced positive intraoperative fluid balance compared to that achieved by the conventional fluid therapy used in the control. Multiple regression analysis showed that GDT application, epidural anesthesia, operative time, and hydroxyethyl-starch infusion volume were associated with blood loss.
Conclusion
Compared to conventional management, SVV-guided GDT may reduce blood loss during hepatectomies.



Similar content being viewed by others
References
Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, Corvera C, Weber S, Blumgart LH. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg. 2002;236(4): 397–406 (discussion -7).
Katz SC, Shia J, Liau KH, Gonen M, Ruo L, Jarnagin WR, Fong Y, D'Angelica MI, Blumgart LH, Dematteo RP. Operative blood loss independently predicts recurrence and survival after resection of hepatocellular carcinoma. Ann Surg. 2009;249(4):617–23.
Huntington JT, Royall NA, Schmidt CR. Minimizing blood loss during hepatectomy: a literature review. J Surg Oncol. 2014;109(2):81–8.
Li Z, Sun YM, Wu FX, Yang LQ, Lu ZJ, Yu WF. Controlled low central venous pressure reduces blood loss and transfusion requirements in hepatectomy. World J Gastroenterol. 2014;20(1):303–9.
Hughes MJ, Ventham NT, Harrison EM, Wigmore SJ. Central venous pressure and liver resection: a systematic review and meta-analysis. HPB (Oxford). 2015;17(10):863–71.
Zhang XL, Wang WJ, Wang WJ, Cao N. Effectiveness and safety of controlled venous pressure in liver surgery: a systematic review and network meta-analysis. Biomed Res Int. 2015;2015:290234.
Kato M, Kubota K, Kita J, Shimoda M, Rokkaku K, Sawada T. Effect of infra-hepatic inferior vena cava clamping on bleeding during hepatic dissection: a prospective, randomized, controlled study. World J Surg. 2008;32(6):1082–7.
Choi SS, Jun IG, Cho SS, Kim SK, Hwang GS, Kim YK. Effect of stroke volume variation-directed fluid management on blood loss during living-donor right hepatectomy: a randomised controlled study. Anaesthesia. 2015;70(11):1250–8.
Lee J, Kim WH, Ryu H-G, Lee H-C, Chung E-J, Yang S-M, Jung C-W. Stroke volume variation-guided versus central venous pressure-guided low central venous pressure with milrinone during living donor hepatectomy: a randomized double-blinded clinical trial. Anesth Analg. 2017;125(2):423–30.
Correa-Gallego C, Tan KS, Arslan-Carlon V, Gonen M, Denis SC, Langdon-Embry L, Grant F, Kingham TP, DeMatteo RP, Allen PJ, D'Angelica MI, Jarnagin WR, Fischer M. Goal-directed fluid therapy using stroke volume variation for resuscitation after low central venous pressure-assisted liver resection: a randomized clinical trial. J Am Coll Surg. 2015;221(2):591–601.
KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl. 2012;2:1–138.
Feltracco P, Brezzi ML, Barbieri S, Serra E, Milevoj M, Ori C. Epidural anesthesia and analgesia in liver resection and living donor hepatectomy. Transpl Proc. 2008;40(4):1165–8.
McNally SJ, Revie EJ, Massie LJ, McKeown DW, Parks RW, Garden OJ, Wigmore SJ. Factors in perioperative care that determine blood loss in liver surgery. HPB (Oxford). 2012;14(4):236–41.
Chen JS, Huang JQ, Chen XL, Zhan GF, Feng JT. Risk factors associated with intraoperative major blood loss during resection of hepatocellular carcinoma. Hepatogastroenterology. 2015;62(140):790–3.
Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transpl. 2013;48(3):452–8.
Avellan S, Uhr I, McKelvey D, Sondergaard S. Identifying the position of the right atrium to align pressure transducer for CVP: spirit level or 3D electromagnetic positioning? J Clin Monit Comput. 2017;31(5):943–9.
Dunki-Jacobs EM, Philips P, Scoggins CR, McMasters KM, Martin RC 2nd. Stroke volume variation in hepatic resection: a replacement for standard central venous pressure monitoring. Ann Surg Oncol. 2014;21(2):473–8.
Seo H, Jun I-G, Ha T-Y, Hwang S, Lee S-G, Kim Y-K. High Stroke Volume Variation Method by Mannitol Administration Can Decrease Blood Loss During Donor Hepatectomy. Medicine. 2016;95(2):e2328.
Sun Y, Chai F, Pan C, Romeiser JL, Gan TJ. Effect of perioperative goal-directed hemodynamic therapy on postoperative recovery following major abdominal surgery-a systematic review and meta-analysis of randomized controlled trials. Crit Care. 2017;21(1):141.
Kozek-Langenecker SA. Effects of hydroxyethyl starch solutions on hemostasis. Anesthesiol J Am Soc Anesthesiol. 2005;103(3):654–60.
Oh C-S, Sung T-Y, Kim S-H, Kim D-K, Lim J-A, Woo N-S. Assessment of coagulation with 6% hydroxyethyl starch 130/0.4 in cesarean section. Korean J Anesthesiol. 2012;62(4):337–42.
Acknowledgements
We thank Professor Akinobu Taketomi, Associated Professor Toshiya Kamiyama, and their colleagues of Department of Gastroenterological Surgey I in Hokkkaido University Hospital for their cooperation in perioperative management. We also thank Yoichi Itoh for his advice in setting primary endpoint and statistical analyses.
Funding
None (Self-funding).
Author information
Authors and Affiliations
Contributions
KM contributed to design of study, data analysis, and preparation of the manuscript. He approved the final manuscript. YM helped with design of study and drafting the manuscript and approved the final manuscript. TF, MY, and NT helped with acquisition of original data and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest associated with this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Mizunoya, K., Fujii, T., Yamamoto, M. et al. Two-stage goal-directed therapy protocol for non-donor open hepatectomy: an interventional before–after study. J Anesth 33, 656–664 (2019). https://doi.org/10.1007/s00540-019-02688-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-019-02688-4