Abstract
Purpose
Hypotension and decreased cardiac output (CO) are common adverse effects during anesthesia induction depending on the patient’s pre-anesthetic cardiac condition. The aim of this study was to assess the ability of hydroxyethyl starch (HES) 130/0.4 to prevent hypotension and decreased CO during the induction of general anesthesia.
Methods
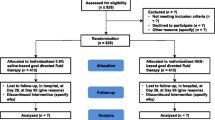
Ninety patients undergoing laparoscopic surgery were randomly divided into a HES group and a crystalloid group. Following the insertion of an intravenous line, fluid was administered to each patient at a rate of 25 ml/min using either crystalloid or HES 130/0.4. Five minutes after the initiation of fluid loading, anesthesia was induced using propofol (1.5 mg/kg), rocuronium (0.9 mg/kg), and remifentanil (0.3 mcg/kg/min). Tracheal intubation was performed 5 min after the induction of anesthesia. Following tracheal intubation, general anesthesia was maintained using remifentanil and sevoflurane. Non-invasive blood pressure (BP) level was measured at 1-min intervals and CO was measured continuously using electrical cardiometry from the start of fluid loading until 5 min after tracheal intubation.
Results
The number of patients with hypotension (systolic BP < 90 mmHg or 80% of baseline) was significantly lower in the HES group (p < 0.001) than in the crystalloid group. Patients in the HES group showed smaller CO decreases than did patients in the crystalloid group (p < 0.001). The Kaplan–Meier method showed a lower incidence and significantly slower onset of hypotension in the HES group (p = 0.009). Multivariate logistic regression models indicated that the use of HES is an independent factor for the prevention of both hypotension and decreased CO (below 85% of baseline; p < 0.005 for both).
Conclusions
Co-loading using HES 130/0.4 prevented hypotension and decreased CO during general anesthesia induction.



Similar content being viewed by others
References
Bijker JB, van Klei WA, Kappen TH, van Wolfswinkel L, Moons KG, Kalkman CJ. Incidence of intraoperative hypotension as a function of the chosen definition: literature definitions applied to a retrospective cohort using automated data collection. Anesthesiology. 2007;107:213–20.
Lima EQ, Zanetta DM, Castro I, Massarollo PC, Mies S, Machado MM, Yu L. Risk factors for development of acute renal failure after liver transplantation. Ren Fail. 2003;25:553–60.
Latson TW, Ashmore TH, Reinhart DJ, Klein KW, Giesecke AH. Autonomic reflex dysfunction in patients presenting for elective surgery is associated with hypotension after anesthesia induction. Anesthesiology. 1994;80:326–37.
Lonjaret L, Lairez O, Minville V, Geeraerts T. Optimal perioperative management of arterial blood pressure. Integr Blood Press Control. 2014;7:49–59.
Lin FQ, Li C, Zhang LJ, Fu SK, Chen GQ, Yang XH, Zhu CY, Li Q. Effect of rapid plasma volume expansion during anesthesia induction on haemodynamics and oxygen balance in patients undergoing gastrointestinal surgery. Int J Med Sci. 2013;10:355–61.
van Waes JA, van Klei WA, Wijeysundera DN, van Wolfswinkel L, Lindsay TF, Beattie WS. Association between intraoperative hypotension and myocardial injury after vascular surgery. Anesthesiology. 2016;124:35–44.
Onuigbo MA, Agbasi N. Association of intraoperative hypotension with acute kidney injury after elective non-cardiac surgery-prevention is better than cure. Ren Fail. 2016;38:168–9.
Bijker JB, van Klei WA, Vergouwe Y, Eleveld DJ, van Wolfswinkel L, Moons KG, Kalkman CJ. Intraoperative hypotension and 1-year mortality after noncardiac surgery. Anesthesiology. 2009;111:1217–26.
Walsh M, Devereaux PJ, Garg AX, Kurz A, Turan A, Rodseth RN, Cywinski J, Thabane L, Sessler DI. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: toward an empirical definition of hypotension. Anesthesiology. 2013;119:507–15.
Lienhart A, Auroy Y, Pequignot F, Benhamou D, Warszawski J, Bovet M, Jougla E. Survey of anesthesia-related mortality in france. Anesthesiology. 2006;105:1087–97.
Lehmann GB, Asskali F, Boll M, Burmeister MA, Marx G, Hilgers R, Forster H. Hes 130/0.42 shows less alteration of pharmacokinetics than HES 200/0.5 when dosed repeatedly. Br J Anaesth. 2007;98:635–44.
Gandhi SD, Weiskopf RB, Jungheinrich C, Koorn R, Miller D, Shangraw RE, Prough DS, Baus D, Bepperling F, Warltier DC. Volume replacement therapy during major orthopedic surgery using Voluven (hydroxyethyl starch 130/0.4) or Hetastarch. Anesthesiology. 2007;106:1120–7.
Teoh WH, Sia AT. Colloid preload versus coload for spinal anesthesia for cesarean delivery: the effects on maternal cardiac output. Anesth Analg. 2009;108:1592–8.
Mercier FJ, Diemunsch P, Ducloy-Bouthors AS, Mignon A, Fischler M, Malinovsky JM, Bolandard F, Aya AG, Raucoules-Aime M, Chassard D, Keita H, Le Rigouzzo A, Gouez A, Group CW. 6% hydroxyethyl starch (130/0.4) vs Ringer’s lactate preloading before spinal anaesthesia for caesarean delivery: the randomized, double-blind, multicentre caesar trial. Br J Anaesth. 2014;113:459–67.
Arora P, Singh RM, Kundra S, Gautam PL. Fluid administration before caesarean delivery: Does type and timing matter? J Clin Diagn Res 2015; 9: UC01-4.
Verheij J, van Lingen A, Beishuizen A, Christiaans HM, de Jong JR, Girbes AR, Wisselink W, Rauwerda JA, Huybregts MA, Groeneveld AB. Cardiac response is greater for colloid than saline fluid loading after cardiac or vascular surgery. Intensiv Care Med. 2006;32:1030–8.
Hartog CS, Bauer M, Reinhart K. The efficacy and safety of colloid resuscitation in the critically ill. Anesth Analg. 2011;112:156–64.
Hung MH, Zou C, Lin FS, Lin CJ, Chan KC, Chen Y. New 6% hydroxyethyl starch 130/0.4 does not increase blood loss during major abdominal surgery—a randomized, controlled trial. J Formos Med Assoc. 2014;113:429–35.
Feldheiser A, Pavlova V, Bonomo T, Jones A, Fotopoulou C, Sehouli J, Wernecke KD, Spies C. Balanced crystalloid compared with balanced colloid solution using a goal-directed haemodynamic algorithm. Br J Anaesth. 2013;110:231–40.
Alimian M, Mohseni M, Safaeian R, Faiz SH, Majedi MA. Comparison of hydroxyethyl starch 6% and crystalloids for preloading in elective caesarean section under spinal anesthesia. Med Arch. 2014;68:279–81.
Farag E, Argalious M, O’Hara J, Doyle DJ. Safety of HES 130/0.4 not yet settled. Anesth Analg. 2013;117:528–9.
Chappell D, Jacob M, Hofmann-Kiefer K, Conzen P, Rehm M. A rational approach to perioperative fluid management. Anesthesiology. 2008;109:723–40.
Rehm M, Orth V, Kreimeier U, Thiel M, Haller M, Brechtelsbauer H, Finsterer U. Changes in intravascular volume during acute normovolemic hemodilution and intraoperative retransfusion in patients with radical hysterectomy. Anesthesiology. 2000;92:657–64.
Rehm M, Haller M, Orth V, Kreimeier U, Jacob M, Dressel H, Mayer S, Brechtelsbauer H, Finsterer U. Changes in blood volume and hematocrit during acute preoperative volume loading with 5% albumin or 6% hetastarch solutions in patients before radical hysterectomy. Anesthesiology. 2001;95:849–56.
Banerjee A, Stocche RM, Angle P, Halpern SH. Preload or coload for spinal anesthesia for elective cesarean delivery: a meta-analysis. Can J Anaesth. 2010;57:24–31.
Suehiro K, Joosten A, Murphy LS, Desebbe O, Alexander B, Kim SH, Cannesson M. Accuracy and precision of minimally-invasive cardiac output monitoring in children: a systematic review and meta-analysis. J Clin Monit Comput. 2016;30:603–20.
Liu YH, Dhakal BP, Keesakul C, Kacmarek RM, Lewis GD, Jiang Y. Continuous non-invasive cardiac output monitoring during exercise: validation of electrical cardiometry with fick and thermodilution methods. Br J Anaesth. 2016;117:129–31.
Gillies MA, Habicher M, Jhanji S, Sander M, Mythen M, Hamilton M, Pearse RM. Incidence of postoperative death and acute kidney injury associated with i.V. 6% hydroxyethyl starch use: systematic review and meta-analysis. Br J Anaesth. 2014;112:25–34.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Juri, T., Suehiro, K., Kuwata, S. et al. Hydroxyethyl starch 130/0.4 versus crystalloid co-loading during general anesthesia induction: a randomized controlled trial. J Anesth 31, 878–884 (2017). https://doi.org/10.1007/s00540-017-2416-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-017-2416-1