Abstract
Background
High-resolution manometry (HRM) is the gold standard for diagnosing esophageal motility disorders (EMDs); however, it requires specialized equipment. The development of more accessible screening examinations is expected. We evaluated the utility of barium esophagography (BE) screening using two novel findings to diagnose EMDs.
Methods
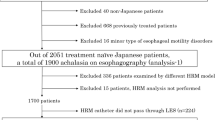
Between January 2013 and October 2020, 244 patients with suspected EMDs who underwent both HRM and BE were analyzed. The EMD diagnosis was based on HRM findings using Chicago Classification version 3.0. BE was performed using sequential esophagography with barium sulfate. Three conventional BE findings (air-fluid level, rosary-bead/corkscrew appearance, and absent/weak peristalsis) and two novel BE findings (wave appearance and supra-junctional ballooning) were used for diagnosis.
Results
The sensitivity and specificity of BE screening using the two novel findings and conventional findings to diagnose EMDs were 79.4% and 88%, respectively [area under the receiver-operating characteristic curve (AUC) = 0.837]. Without these novel findings, they were 63.9% and 96%, respectively (AUC = 0.800), respectively. Achalasia was highly correlated with the air-fluid level (88.7%). Absent contractility was highly correlated with absent/weak peristalsis (85.7%). Relatively high correlations were observed between distal esophageal spasm and rosary-bead/corkscrew appearance (60%), and between achalasia and wave appearance (59.7%). The intra-observer reproducibility and inter-observer agreement for individual BE findings were 84.4% and 75%, respectively. Wave appearance was associated with higher integrated relaxation pressure (IRP) and shorter distal latency. Supra-junctional ballooning was associated with higher IRP.
Conclusions
BE screening using two additional novel findings to diagnose EMDs could be useful in general practice.




Similar content being viewed by others
Data availability
No additional data are available.
References
Katz PO, Dalton CB, Richter JE, et al. Esophageal testing of patients with noncardiac chest pain or dysphagia. Results of three years’ experience with 1161 patients. Ann Intern Med. 1987;106:593–7.
Pandolfino JE, Fox MR, Bredenoord AJ, et al. High-resolution manometry in clinical practice: utilizing pressure topography to classify oesophageal motility abnormalities. Neurogastroenterol Motil. 2009;21:796–806.
Inoue H, Sato H, Ikeda H, et al. Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg. 2015;221:256–64.
Yadlapati R, Kahrilas PJ, Fox MR, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0((c)). Neurogastroenterol Motil. 2021;33:e14058.
Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–74.
Kraft C, Kathpalia P, Baumgardner JM, et al. How to incorporate esophageal manometry teaching in your fellowship program. Gastroenterology. 2019;156:2120–3.
Carroll TL, Werner A, Nahikian K, et al. Rethinking the laryngopharyngeal reflux treatment algorithm: evaluating an alternate empiric dosing regimen and considering up-front, pH-impedance, and manometry testing to minimize cost in treating suspect laryngopharyngeal reflux disease. Laryngoscope. 2017;127(Suppl 6):S1-s13.
Ott DJ, Richter JE, Chen YM, et al. Esophageal radiography and manometry: correlation in 172 patients with dysphagia. AJR Am J Roentgenol. 1987;149:307–11.
Schima W, Stacher G, Pokieser P, et al. Esophageal motor disorders: videofluoroscopic and manometric evaluation–prospective study in 88 symptomatic patients. Radiology. 1992;185:487–91.
O’Rourke AK, Lazar A, Murphy B, et al. Utility of esophagram versus high-resolution manometry in the detection of esophageal dysmotility. Otolaryngol Head Neck Surg. 2016;154:888–91.
Eckardt VF, Aignherr C, Bernhard G. Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology. 1992;103:1732–8.
Fleiss JLLB, Paik MC. Statistical methods for rates and proportions. 3rd ed. Hoboken: John Wiley & Sons Inc.; 2003.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Schlottmann F, Neto RML, Herbella FAM, et al. Esophageal achalasia: pathophysiology, clinical presentation, and diagnostic evaluation. Am Surg. 2018;84:467–72.
Van Hoeij FB, Ponds FA, Smout AJ, et al. Incidence and costs of achalasia in The Netherlands. Neurogastroenterol Motil. 2018;30:e13195.
Hamada S, Ihara E, Ikeda H, et al. Clinical characterization of vonoprazan-refractory gastroesophageal reflux disease. Digestion. 2021;102:197–204.
Kuo P, Holloway RH, Nguyen NQ. Current and future techniques in the evaluation of dysphagia. J Gastroenterol Hepatol. 2012;27:873–81.
Schlottmann F, Herbella FA, Patti MG. Understanding the Chicago classification: from tracings to patients. J Neurogastroenterol Motil. 2017;23:487–94.
Balko RA, Codipilly DC, Ravi K. Minor esophageal functional disorders: are they relevant? Curr Treat Options Gastroenterol. 2020;18:82–96.
Stiennon OA. On the cause of tertiary contractions and related disturbances of the esophagus. Am J Roentgenol Radium Ther Nucl Med. 1968;104:617–24.
Blonski W, Kumar A, Feldman J, et al. Timed barium swallow: diagnostic role and predictive value in untreated achalasia, esophagogastric junction outflow obstruction, and non-achalasia dysphagia. Am J Gastroenterol. 2018;113:196–203.
Hamada S, Ihara E, Muta K, et al. Onigiri esophagography as a screening test for esophageal motility disorders. J Neurogastroenterol Motil. 2022;28:43–52.
Acknowledgements
The authors would like to thank Junji Kishimoto (Center for Clinical and Translational Research at Kyushu University Hospital) for reviewing the statistical methods of this study. The authors would like to thank Editage for English language editing.
Funding
This study was partially supported by the Japan Society for the Promotion of Science KAKENHI (20K08334).
Author information
Authors and Affiliations
Contributions
YH, EI, and HO contributed to the study conception and design. Material preparation and data collection were performed by YH, MW, HT, KM, XB, YT, and RS. YM and ME performed statistical analysis. YH and EI mainly wrote the manuscript. TC and YO supervised this study and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
E.I. belongs to an endowed course supported by companies including Ono Pharmaceutical Co., Ltd., Miyarisan Pharmaceutical Co., Ltd., Sanwa Kagaku Kenkyusho Co., Ltd., Otsuka Pharmaceutical Factory, Inc., Fujifilm Medical Co., Ltd., Terumo Corporation, FANCL Corporation, Ohga Pharmacy, and Abbott Japan, LLC. E.I. receives a lecture honorarium from Takeda Pharmaceutical Company. Y.O. conducts collaborative research with Fujifilm Medical Co., Ltd. and FANCL Corporation. The other authors have no conflicts of interest to declare in relation to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hata, Y., Ihara, E., Wada, M. et al. Improved esophagography screening for esophageal motility disorders using wave appearance and supra-junctional ballooning. J Gastroenterol 57, 838–847 (2022). https://doi.org/10.1007/s00535-022-01913-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-022-01913-4