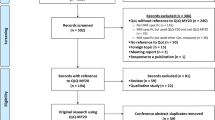
Abstract
Background
Patients with multiple myeloma experience severe symptom burden. Patient participation in self-reporting is essential as medical staff’s assessment of patient symptom severity is often lower than patient self-reporting. This article reviews patient-reported outcome (PRO) assessment tools and their application in the field of multiple myeloma.
Results
The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 (EORTC QLQ-C30) is the universal patient-reported outcome assessment tool most frequently used to evaluate the life quality in people with multiple myeloma. Among the specific patient-reported outcome assessment tools, the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Multiple Myeloma Module (EORTC QLQ-MY20), the Functional Assessment of Cancer Therapy-Multiple Myeloma (FACT-MM), and the M.D. Anderson Symptom Inventory-Multiple Myeloma Module (MDASI-MM) are the most widely used, with some scholars using the EORTC QLQ-MY20 as a calibration correlate for scale development.
Most current assessment instruments were developed using classical measurement theory methods; future researchers could combine classic theory tests and item response theory to create scientific assessment instruments.
In addition, researchers select the appropriate assessment tool based on the purpose of the study. They can translate high-quality assessment tools into different languages and consider applying them more often to assessing multiple myeloma patients. Finally, most existing PROs focus on measuring life quality and symptoms in people with multiple myeloma, with less research on outcomes such as adherence and satisfaction, thus failing to comprehensively evaluate the patient treatment and disease management.
Conclusions
Research has shown that the field of PROs in multiple myeloma is in an exploratory phase. There is still a need to enrich the content of PROs and develop more high-quality PRO scales for multiple myeloma based on the strengths and weaknesses of existing tools. With the successful advancement of information technology, PROs for people with multiple myeloma could be integrated with electronic information systems, allowing patients to report their health status in real time and doctors to track their condition and adjust their treatment, thereby improving patient outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple myeloma, a proliferative clonal malignant plasmocyte disease, is the second most common hematological malignancy [1, 2]. The number of new cases of multiple myeloma in the USA is 35,000 annually, and approximately 588,000 worldwide [3]. Multiple myeloma cases increased by 126% worldwide from 1990 to 2016, and deaths by 94% [4]. Studies have shown that people with multiple myeloma have experienced a more significant symptom burden in recent years than patients with other hematological malignancies [5]. With the development of autologous stem cell transplantation technology and the introduction of new drugs, the survival rate of multiple myeloma has improved. Patients have to cope with ongoing disease symptoms and repeated treatment toxicities. Therefore, it is important to focus on the quality of life as one of the priorities.
Currently, disease assessment relies on objective indicators such as physical examination, laboratory tests, and imaging, which may underestimate the impact of the disease on the individual and overestimate the effectiveness of medical interventions [6]. Patient-reported outcomes (PROs) are derived directly from the patient’s subjective assessment, including reports of their symptoms, health-related quality of life, daily and social functioning, and patient satisfaction, which do not require interpretation by medical staff or any other person [7]. In contrast, PROs provide a patient’s eye view of their condition. Providers can provide patients with timely, personalized medical care based on patient-reported outcomes. Patient-reported outcomes can provide evidence for medical decision-making and health policy development and as a reference indicator for symptom monitoring.
This article reviews the main components, psychometric characteristics, applications, and limitations of commonly used tools for assessing PROs in multiple myeloma. It discusses future directions for PROs in the clinical field, intending to generate helpful evidence.
Multiple myeloma universal patient-report outcome assessment tool
Medical Outcome Study Short Form 36
The Medical Outcome Study Short Form 36 (SF-36) [8] is a brief health questionnaire based on the Medical Outcome Study (MOS) in the USA. It is primarily used in clinical research, health policy evaluation, and general population surveys. The SF-36 is one of the most widely used standardized quality-of-life measurement instruments internationally and has been translated into more than 40 languages. The SF-36 can be collected by self-assessment, another assessor, or telephone questioning and takes about 15 min to complete. However, it has many entries and a significant response burden, so some scholars have developed a shortened form, consisting of 12 and 8 entries for the SF-12 and SF-8, respectively, to shorten the completion time.
European Quality-of-Life Five-Dimension Scale
The European Quality-of-Life Five-Dimension Scale (EQ-5D) [9] is a multidimensional health-related quality-of-life scale developed by the European Research Group on Quality of Life in 1990, consisting of 2 components, the Health Description System and the Visual Analogue Scale (EQ-5D Visual Analogue Scale, EQ-VAS). The Health Descriptor System reflects three areas of physical health, social functioning, and mental health and can be completed in 10 min. The EQ-VAS is used to measure the overall health status of the subject. The EQ-5D Scale was used by Plesner et al. [10] to assess the quality of life in a clinical trial of a drug for multiple myeloma. The unique to this tool is that it can be used to estimate quality-adjusted life year (QALY) gains in health economic evaluation and has been used in several countries, including the UK, Germany, and the USA. However, it measures the subject’s condition on the same day, and its retest reliability is low when the retest interval is more than 1 week, so the scale is more suitable for measuring the quality of life in chronic diseases.
Edmonton Symptom Assessment System
In 1991, Canadian researchers Bruera and colleagues developed the Edmonton Symptom Assessment System (ESAS), assessing the incidence and severity of physical and mental symptoms among cancer patients with advanced and palliative diseases [11]. It has nine required symptoms, such as discomfort, tiredness, nausea, and loss of appetite, plus one optional symptom. Chinese academics 2015 revised it and added “itchy skin” to the Chinese translation, which scored 0.72 on Cronbach’s alpha [12]. However, it was not tested for validity. Ebraheem and colleagues explored factors affecting symptoms in multiple myeloma patients receiving autologous stem cell transplants using the ESAS [13]. Despite the scale’s widespread use, Bruera does not specify a timeframe for the assessment, and most scholars use the “last 24 h” for assessment. ESAS is simple, easy to perform, and equally applicable to chronic non-cancer patients with palliative care needs [14].
Furthermore, the assessment results can be translated into symptom trends and accurately determine the severity of a patient’s symptoms. Its limitations are that individual entries are not accurate, and some scholars have revised “appetite” to “loss of appetite” and reordered and regrouped the nine symptoms [15]. The scale is not comprehensive enough as it only contains nine symptoms of cancer patients. Researchers should use this scale in conjunction with other scales to evaluate the full range of symptoms in cancer patients.
Memorial Symptom Assessment Scale
The Memorial Sloan-Kettering Cancer Center in the USA created the Memorial Symptom Assessment Scale (MSAS), which consists of 32 entries, developed in 1994 [16] to assess the physical and psychological symptoms, and global distress index in cancer patients over the past week. Twenty-four entries assess symptoms’ incidence, severity, and distress, while eight entries assess the severity and distress of symptoms. Cheng et al. [17] showed that the internal consistency of the Chinese version of the MSAS was 0.79–0.87, and the content validity was 0.94 in assessing the symptoms of Chinese cancer patients. The scale is comprehensive and covers 32 common cancer symptoms, but it is time-consuming to complete, and the scoring rules are complex.
Based on this, some researchers revised the Memorial Symptom Assessment Scale Short Form (MSAS-SF) and the Condensed Memorial Symptom Assessment Scale (CMSAS), measuring the incidence and distress of 32 and 14 symptoms, respectively [18]. The Chinese versions of the MSAS-SF and CMSAS Cronbach’s alpha coefficients ranged from 0.84 to 0.91 and 0.79 to 0.87, respectively, with good construct validity [19]. Chen et al. used the Chinese version of the MSAS-SF to investigate symptom clusters in outpatients with multiple myeloma. They discovered three symptom clusters: the psychological symptom cluster, the painful dry mouth and sleep difficulty symptom cluster, and the fatigue symptom cluster. There was a link between the symptom clusters and the clinical symptoms [20]. No MSAS-specific module for multiple myeloma is currently available.
Hematological Malignancy Specific Patient-Reported Outcomes Measure
In 2020, Goswami et al. developed the Hematological Malignancy Specific Patient-Reported Outcomes Measure (HM-PRO) [21] and applied it to all hematological malignancies. The scale contains two subscales, scale A and scale B. Scale A assesses the impact of the disease and associated treatments on the patient’s quality of life. Scale B evaluates the severity of symptoms and side effects of treatment over the previous 3 days.
The HM-PRO is the first universal quality of life and symptom measurement scale for hematological malignancies. It was developed using a combination of classic theory tests and item response theory, and it has excellent reliability and responsiveness. The HM-PRO not only permits early identification of the factors that have the most significant impact on patients during treatment and disease, but also allows for evaluating the effectiveness of treatments and monitoring dynamic changes in patients’ life quality [22]. Due to the late development of the scale, neither domestic nor international research has yet to use it. As a result, its scientific validity can be validated through large-scale studies in the future.
Multiple myeloma-specific patient-reported outcome assessment tool
European Organization for Research and Treatment of Cancer, the Quality-of-Life Questionnaire-Multiple Myeloma Module
In 1999, Stead et al. developed the European Organization for Research and Treatment of Cancer Quality-of-Life Questionnaire-Multiple Myeloma Module (EORTC QLQ-MY24) [23]. The twenty-four items span five dimensions: body image, social support, future perspective, side effects of treatment, and disease symptoms. In 2007, Cocks et al. [24] removed the social support dimension due to its ceiling effect and revised the remaining four dimensions into the EORTC QLQ-MY20, designed to assess the quality-of-life status of people with multiple myeloma over the past week.
Notably, the EORTC QLQ-MY20 is a multiple myeloma-specific scale developed based on The Quality of Life Questionnaire Core 30 (QLQ-C30) [25], which needs to be combined with the EORTC QLQ-C30 to measure the quality of life of people with multiple myeloma. Li et al. [26] applied the EORTC QLQ-MY20 scale to investigate the life quality of Chinese people with multiple myeloma. It showed that people with multiple myeloma have a low quality of life and are closely related to their physical condition and depression and anxiety, disease stage, and whether the diagnosis was made early. The most widely utilized quality-of-life scale in multiple myeloma is the EORTC QLQ-MY20, which is comprehensive, translated, and used in many nations [27,28,29,30]. However, when combined with the QLQ-C30, the number of entries is excessive and may lead to a patient response burden [31]. Future researchers can make the scale more streamlined and optimized to meet our needs.
Functional Assessment of Cancer Therapy-Multiple Myeloma
Wagner et al. developed the Functional Assessment of Cancer Therapy-Multiple Myeloma (FACT-MM) in 2012 [32]. The scale consists of the FACT-General Scale (FACT-G) [33] and multiple myeloma-specific modules designed to assess patients’ health states and life quality during the previous week. The multiple myeloma-specific modules consist of 14 entries, including bone pain, physical pain, fatigue, difficulty walking, and weight gain.
Gupta et al. utilized the FACT-MM to investigate how treatment adherence impacts reported outcomes in patients with multiple myeloma [34]. Due to its comprehensiveness and focus on psychiatric symptoms, the FACT-MM is the most popular quality-of-life instrument for multiple myeloma patients after the EORTC QLQ-MY20. However, the measurement could have been more precise because of the study population’s racial diversity, young age, and the fact that 38% of patients were in remission. To investigate the applicability of the scale to patients with multiple myeloma of various races, ages, and disease stages, in the future, may increase the population.
M.D. Anderson Symptom Inventory-Multiple Myeloma Module
The M.D. Anderson Symptom Inventory-Multiple Myeloma Module (MDASI-MM)[31] is a specific version of the M.D. Anderson Symptom Inventory (MDASI) [35], developed by Jones et al. at the Anderson Cancer Center in 2013 to assess the severity of symptoms and their interference with daily life in the past 24 h in people with multiple myeloma. Several authors [36] have investigated that the MDASI-MM can be a sensitive measure of symptom burden in relapsed or refractory multiple myeloma. Wang et al. [37] used the scale to explore the relationship between inflammatory markers and symptom burden during autologous stem cell transplantation in people with multiple myeloma and confirmed a correlation between the two.
Unlike the EORTC QLQ-MY20 and FACT-MM, which include symptom assessment but were developed based on a framework of health-related quality of life, the MDASI-MM was developed based on a framework of symptom assessment and is an accurate symptom assessment scale. The MDASI-MM has concise entries that capture the most critical symptom issues for patients with minimal response burden and is widely recognized. It is clinically applicable and supports an interactive verbal response system for symptom assessment [37]. It also allows repeated measurement of patient symptom severity [38], providing an additional advantage for longitudinal studies of symptoms. In addition, the MDASI specificity module was developed based on the MDASI core module and facilitated the comparison of symptom incidence and severity across cancers. The sample size could be increased for future multi-center research to address the drawback of the included samples from the same cancer center. Secondly, it could be cross-culturally adapted to allow for accurate symptom assessment of multiple myeloma patients from different countries and ethnicities.
Myeloma Patient Outcome Scale
In 2015, Osborne et al. created the Myeloma Patient Outcome Scale (MyPOS), based on the Palliative Care Outcome Scale, to evaluate the quality of life of multiple myeloma patients in the clinical setting by engaging patients to recall health problems from the past 7 days [39]. Ramsenthaler et al. [40] applied the scale to measure the quality of life trajectories and palliative care issues in 238 people with multiple myeloma and showed that a decline in quality of life was associated with high levels of symptoms, pain, and anxiety and that clinical attention should be paid to patient-reported symptoms and psychosocial health to identify patients with palliative care needs.
Unlike the EORTC QLQ-MY20 and FACT-MM, which are primarily applicable to clinical trials, the MyPOS is the first multiple myeloma scale explicitly developed for clinical care, covering medical support items to assess patient understanding of the disease and satisfaction with treatment. MyPOS had a 91.6% response rate for the sexual functioning items in the original authors’ study. Despite this, low response rates to sexual functioning items may occur due to cultural differences in different countries. In addition, the healthcare support dimension’s low reliability and ceiling effect limit its widespread use, and continued refinement is needed to improve item response rates and reliability. Currently, the scale has only been translated into German [41].
Multiple Myeloma Symptom and Impact Questionnaire
American researchers Gries et al. [42] created the Multiple Myeloma Symptom and Impact Questionnaire (MySIm-Q) in 2021 to assess the symptoms experienced by patients with active multiple myeloma treated with immunological drugs in the past week and their impact on daily life. For the first time, a leg pain entry was added to the pain dimension to assess pain symptoms associated with areas other than the back or legs in people with multiple myeloma. The MySIm-Q does not evaluate the adverse effects of the therapy and only concentrates on the symptoms linked to the disease itself. The MySIm-Q was developed using a combination of classic theory test and item response theory, incorporating ethnically diverse populations as study participants with good content validity. A limitation is that the scale has yet to be reported in other studies, as psychometric properties such as internal consistency and construct validity are being validated. The scale is promising given that it was developed specifically for people with multiple myeloma treated with immunological agents and that the treatment of multiple myeloma is currently in a new era of immunology where new immunotherapeutic approaches are receiving increasing scholarly attention.
Discussion
The SF-36, EQ-5D, and EORTC QLQ-C30 are the universal patient-reported outcome assessment tools most frequently used to evaluate the life quality in people with multiple myeloma. In contrast, the ESAS and MSAS are commonly used to assess symptoms in people with multiple myeloma. The EORTC QLQ-MY20, FACT-MM, and MDASI-MM are the most widely used among the specific patient-reported outcome assessment tools. Some scholars use the EORTC QLQ-MY20 as a calibration correlate for scale development.
Table 1 shows the characteristics and psychometric properties of eight patient-reported outcome assessment tools for multiple myeloma.
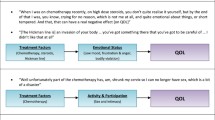
Applications
Most patients with MM require multiple treatment options and have cumulative toxicity and a high symptom burden. In contrast, symptom management is integral to care management, and effective symptom management is essential for improving a patient’s quality of life. Ramsenthaler et al. [43] used MyPOS and EORTC QLQ-C30 and QLQ-MY20 to investigate symptoms and quality of life in patients with multiple myeloma and showed that an average of 7.2 symptoms were present per patient to painful multiple myeloma patients with high symptom burden and low HRQOL in late and early disease. Therefore, the focus in the clinic should be on assessing patient-reported outcomes, enhancing patient symptom management, and improving quality of life. In summary, PROs can investigate patients’ existing symptom problems, monitor changes in symptoms, and help healthcare professionals develop comprehensive interventions to improve the quality of care.
PROs can help healthcare professionals gather health information, such as daily symptoms and drug toxicity reactions, and develop more standardized and personalized treatment protocols through a comprehensive assessment of treatment effectiveness. The introduction of PRO evaluation in clinical trials and practice, and as an endpoint indicator in clinical trials, is advocated in the PROs in Haematology guidelines.
In addition, Dubois scholars found PRO data to be of prognostic value for patient survival when bortezomib was administered to 202 patients with multiple myeloma [44].
Limitations
Most current assessment tools have been developed using classical measurement theory methods, with limitations such as identical test items, dependence on sample size, broad and single-error indicators, and imprecise reliability estimates [45]. Secondly, there are still limitations to using multiple myeloma-specific scales worldwide due to language limitations, with most studies using universal scales. Thirdly, most of these PRO assessment tools were developed before developing newer therapies (e.g., monoclonal antibodies, CAR-T therapies, T cell engagers) with different side effect profiles. Furthermore, patients may have various quality-of-life needs during the maintenance phase of treatment after autologous transplantation, and these tools cannot cover all of them. Finally, most of the available PROs focus on measuring the quality of life and symptoms in patients with multiple myeloma, with less research on outcomes such as adherence and satisfaction, thus failing to assess patient treatment and disease management comprehensively.
Future perspectives
It is recommended that future researchers combine classical test theory and item response theory to develop multiple myeloma-specific scales that cover various dimensions such as physical, psychological, social, satisfaction, and treatment adherence, thereby helping healthcare professionals to assess patients and take targeted measures and care comprehensively. In addition, researchers should select appropriate assessment tools according to the purpose of the study. Existing high-quality assessment tools can be translated into different languages and considered for greater use in assessing patients with multiple myeloma. Finally, researchers can combine advances in information technology and artificial intelligence to develop management systems suitable for patients with multiple myeloma, combining electronic versions of assessment tools with patient management systems to enable the sharing of doctor-patient information and provide a realistic basis for patient participation in treatment decisions and facilitate patient management.
Conclusion
Research has shown that the field of PROs in multiple myeloma is in an exploratory phase. There is still a need to enrich the content of PROs and develop more high-quality PRO scales for multiple myeloma based on the strengths and weaknesses of existing tools. With the successful advancement of information technology, PROs for people with multiple myeloma could be integrated with electronic information systems, allowing patients to report their health status in real time and doctors to track their condition and adjust their treatment, thereby improving patient outcomes.
References
Owens B (2020) Outlook: Multiple myeloma. Nat 587(7835):S55. https://doi.org/10.1038/d41586-020-03223-2
Yan Z, Liya Q, Rui C et al (2022) Identification and emergency care of sudden loss of consciousness in patients with multiple myeloma complicated with myocardial amyloidosis. Chin J Emerg Crit Care Nurs 3(4):335–337. https://doi.org/10.3761/j.issn.2096-7446.2022.04.008
Silberstein J, Tuchman S, Grant SJ (2022) What Is multiple myeloma? Jama 327(5):497. https://doi.org/10.1001/jama.2021.25306
Cowan AJ, Allen C, Barac A et al (2018) Global burden of multiple myeloma: a systematic analysis for the Global Burden of Disease Study 2016. JAMA Oncol 4(9):1221–1227. https://doi.org/10.1001/jamaoncol.2018.2128
Chakraborty R, Hamilton BK, Hashmi SK et al (2018) Health-related quality of life after autologous stem cell transplantation for multiple myeloma. Biol Blood Marrow Transplant 24(8):1546–1553. https://doi.org/10.1016/j.bbmt.2018.03.027
Brundage MD, Crossnohere NL, O’Donnell J et al (2022) Listening to the patient voice adds value to cancer clinical trials. J Natl Cancer Inst 114(10):1323–1332. https://doi.org/10.1093/jnci/djac128
Kaufmann TL, Rocque GB (2021) Pathway to precision patient-reported outcomes. J Clin Oncol 39(34):3770–3772. https://doi.org/10.1200/JCO.21.02163
Brazier JE, Harper R, Jones NM et al (1992) Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 305(6846):160–164. https://doi.org/10.1136/bmj.305.6846.160
Catto J, Downing A, Mason S et al (2021) Quality of Life After bladder cancer: a cross-sectional survey of patient-reported outcomes. Eur Urol 79(5):621–632. https://doi.org/10.1016/j.eururo.2021.01.032
Plesner T,Dimopoulos M A,Oriol A,et al. (2021) Health-related quality of life in patients with relapsed or refractory multiple myeloma: treatment with daratumumab, lenalidomide, and dexamethasone in the phase 3 POLLUX trial. Br J Haematol 194(1):132-139. https://doi.org/10.1111/bjh.17435
Sprague E, Siegert RJ, Medvedev O et al (2018) Rasch analysis of the Edmonton symptom assessment system. J Pain Symptom Manage 55(5):1356–1363. https://doi.org/10.1016/j.jpainsymman.2018.01.016
Dong Y, Chen H, Zheng Y et al (2015) Psychometric validation of the edmonton symptom assessment system in Chinese patients. J Pain Symptom Manage 50(5):712–717. https://doi.org/10.1016/j.jpainsymman.2015.05.018
Ebraheem MS, Seow H, Balitsky AK et al (2021) Trajectory of symptoms in patients undergoing autologous stem cell transplant for multiple myeloma: a population-based cohort study of patient-reported outcomes. Clin Lymphoma Myeloma Leuk 21(9):e714–e721. https://doi.org/10.1016/j.clovemylife.2021.05.002
Quinn KL, Shurrab M, Gitau K et al (2020) Association of receipt of palliative care interventions with health care use, quality of life, and symptom burden among adults with chronic noncancer illness: a systematic review and meta-analysis. JAMA 324(14):1439–1450. https://doi.org/10.1001/jama.2020.14205
Yokomichi N, Morita T, Nitto A et al (2015) Validation of the Japanese Version of the Edmonton Symptom Assessment System-Revised. J Pain Symptom Manage 50(5):718–723. https://doi.org/10.1016/j.jpainsymman.2015.05.014
Maguire R, McCann L, Kotronoulas G et al (2021) Real time remote symptom monitoring during chemotherapy for cancer: European multicentre randomised controlled trial (eSMART). BMJ 374:n1647. https://doi.org/10.1136/bmj.n1647
Cheng KK et al (2009) Measuring the symptom experience of Chinese cancer patients: a validation of the Chinese version of the memorial symptom assessment scale. J Pain Symptom Manage 37(1):44–57. https://doi.org/10.1016/j.jpainsymman.2007.12.019
Llamas-Ramos I, Llamas-Ramos R, Buz J et al (2018) Construct validity of the Spanish versions of the Memorial Symptom Assessment Scale Short Form and Condensed Form: Rasch analysis of responses in oncology outpatients. J Pain Symptom Manage 55(6):1480–1491. https://doi.org/10.1016/j.jpainsymman.2018.02.017
Lam WW, Law CC, Fu YT et al (2008) New insights in symptom assessment: the Chinese Versions of the Memorial Symptom Assessment Scale Short Form (MSAS-SF) and the Condensed MSAS (CMSAS). J Pain Symptom Manage 36(6):584–595. https://doi.org/10.1016/j.jpainsymman.2007.12.008
Chen F, Leng Y, Ni J et al (2022) Symptom clusters and quality of life in ambulatory patients with multiple myeloma. Support Care Cancer 30(6):4961–4970. https://doi.org/10.1007/s00520-022-06896-9
Goswami P, Oliva EN, Ionova T et al (2020) Hematological Malignancy Specific Patient-Reported Outcome Measure (HM-PRO): construct validity study. Front Pharmacol 11:1308. https://doi.org/10.3389/fphar.2020.01308
Goswami P, Oliva EN, Ionova T et al (2020) Development of a Novel Hematological Malignancy Specific Patient-Reported Outcome Measure (HM-PRO): content validity. Front Pharmacol 11:209. https://doi.org/10.3389/fphar.2020.00209
Stead ML, Brown JM, Velikova G et al (1999) Development of an EORTC questionnaire module to be used in health-related quality-of-life assessment for patients with multiple myeloma. European Organization for Research and Treatment of Cancer Study Group on Quality of Life. Br J Haematol 104(3):605–611. https://doi.org/10.1046/j.1365-2141.1999.01206.x
Cocks K, Cohen D, Wisløff F et al (2007) An international field study of the reliability and validity of a disease-specific questionnaire module (the QLQ-MY20) in assessing the quality of life of patients with multiple myeloma. Eur J Cancer 43(11):1670–1678. https://doi.org/10.1016/j.ejca.2007.04.022
Efficace F, Cottone F, Sommer K et al (2019) Validation of the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 Summary Score in Patients With Hematologic Malignancies. Value Health 22(11):1303–1310. https://doi.org/10.1016/j.jval.2019.06.004
Li X, Liu J, Chen M et al (2020) Health-related quality of life of patients with multiple myeloma: a real-world study in China. Cancer Med 9(21):7896–7913. https://doi.org/10.1002/cam4.3391
Ahmedzai SH, Snowden JA, Ashcroft AJ et al (2019) Patient-reported outcome results from the open-label, randomized phase III MYELOMA X Trial evaluating salvage autologous stem-cell transplantation in relapsed multiple myeloma. J Clin Oncol 37(19):1617–1628. https://doi.org/10.1200/JCO.18.01006
Leleu X, Masszi T, Bahlis NJ et al (2018) Patient-reported health-related quality of life from the phase III TOURMALINE-MM1 study of ixazomib-lenalidomide-dexamethasone versus placebo-lenalidomide-dexamethasone in relapsed/refractory multiple myeloma. Am J Hematol 93(8):985–993. https://doi.org/10.1002/ajh.25134
Silveira LP, Menezes DPC, Drummond P et al (2021) Validation of an instrument for measuring adherence to treatment with immunomodulators in patients with multiple myeloma. Front Pharmacol 12:651523. https://doi.org/10.3389/fphar.2021.651523
Selvy M, Kerckhove N, Pereira B et al (2021) Prevalence of chemotherapy-induced peripheral neuropathy in multiple myeloma patients and its impact on quality of life: a single center cross-sectional study. Front Pharmacol 12:637593. https://doi.org/10.3389/fphar.2021.637593
Jones D, Vichaya EG, Wang XS et al (2013) Validation of the M. D. Anderson Symptom Inventory multiple myeloma module. J Hematol Oncol 6:13. https://doi.org/10.1186/1756-8722-6-13
Wagner LI, Robinson DJ, Weiss M et al (2012) Content development for the Functional Assessment of Cancer Therapy-Multiple Myeloma (FACT-MM): use of qualitative and quantitative methods for scale construction. J Pain Symptom Manage 43(6):1094–1104. https://doi.org/10.1016/j.jpainsymman.2011.06.019
Tremblay G, Daniele P, Breeze J et al (2021) Quality of life analyses in patients with multiple myeloma: results from the Selinexor (KPT-330) Treatment of Refractory Myeloma (STORM) phase 2b study. BMC Cancer 21(1):993. https://doi.org/10.1186/s12885-021-08453-9
Gupta S, Abouzaid S, Liebert R et al (2018) Assessing the effect of adherence on patient-reported outcomes and out of pocket costs among patients with multiple myeloma. Clin Lymphoma Myeloma Leuk 18(3):210–218. https://doi.org/10.1016/j.clml.2018.01.006
Chan CW, Lee PH, Molassiotis A et al (2020) Symptom clusters in postchemotherapy neutropenic fever in hematological malignancy: associations among sickness behavior symptom cluster, inflammatory biomarkers of procalcitonin and c-reactive protein, and febrile measures. J Pain Symptom Manage 59(6):1204–1211. https://doi.org/10.1016/j.jpainsymman.2019.12.372
Kamal M, Wang XS, Shi Q et al (2021) Symptom burden and its functional impact in patients with “symptomatic” relapsed or refractory multiple myeloma. Support Care Cancer 29(1):467–475. https://doi.org/10.1007/s00520-020-05493-y
Wang XS, Shi Q, Shah ND et al (2014) Inflammatory markers and development of symptom burden in patients with multiple myeloma during autologous stem cell transplantation. Clin Cancer Res 20(5):1366–1374. https://doi.org/10.1158/1078-0432.CCR-13-2442
Cleeland CS, Mendoza TR, Wang XS et al (2000) Assessing symptom distress in cancer patients: the M.D. Anderson Symptom Inventory. Cancer 89(7):1634–1646. https://doi.org/10.1002/1097-0142(20001001)89:7<1634::aid-cncr29>3.0.co;2-v
Osborne TR, Ramsenthaler C, Schey SA et al (2015) Improving the assessment of quality of life in the clinical care of myeloma patients: the development and validation of the Myeloma Patient Outcome Scale (MyPOS). BMC Cancer 15:280. https://doi.org/10.1186/s12885-015-1261-6
Ramsenthaler C, Gao W, Siegert RJ et al (2019) Symptoms and anxiety predict declining health-related quality of life in multiple myeloma: a prospective, multi-centre longitudinal study. Palliat Med 33(5):541–551. https://doi.org/10.1177/0269216319833588
Gerlach C, Taylor K, Ferner M et al (2020) Challenges in the cultural adaptation of the German Myeloma Patient Outcome Scale (MyPOS): an outcome measure to support routine symptom assessment in myeloma care. BMC Cancer 20(1):245. https://doi.org/10.1186/s12885-020-06730-7
Gries KS, Fastenau J, Seo C et al (2021) Development of the Multiple Myeloma Symptom and Impact Questionnaire: a new patient-reported outcome instrument to assess symptom and impacts in patients with multiple myeloma. Value Health 24(12):1807–1819. https://doi.org/10.1016/j.jval.2021.06.010
Ramsenthaler C et al (2016) The impact of disease-related symptoms and palliative care concerns on health-related quality of life in multiple myeloma: a multi-centre study. BMC Cancer 16:427. https://doi.org/10.1186/s12885-016-2410-2
Dubois D et al (2006) Descriptive and prognostic value of patient-reported outcomes: the bortezomib experience in relapsed and refractory multiple myeloma. J Clin Oncol 24(6):976–982. https://doi.org/10.1200/JCO.2005.04.0824
Nguyen TH, Lee CS, Kim MT (2022) Using item response theory to develop and refine patient-reported outcome measures. Eur J Cardiovasc Nurs 21(5):509–515. https://doi.org/10.1093/eurjcn/zvac020
Funding
This work was supported by the Zhejiang Provincial Medical and Health Science and Technology Plan Innovative Talent Project [2021RC011] and the Zhejiang Provincial Medical and Health Science and Technology Program [2023KY789].
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Ting Wang performed data collection and analysis, and Qin Lu, LeiWen Tang, and Ting Wang completed the funding acquisition. Ting Wang wrote the first draft of the manuscript, and all authors commented on previous versions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, T., Lu, Q. & Tang, L. Assessment tools for patient-reported outcomes in multiple myeloma. Support Care Cancer 31, 431 (2023). https://doi.org/10.1007/s00520-023-07902-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07902-4