Abstract
Purpose
To evaluate the implementation of a web-based system of screening for symptoms and needs in people with diverse cancers in a general hospital in Australia.
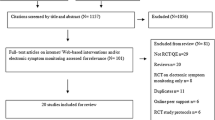
Methods
This was a prospective, single-arm, pragmatic intervention study. After local adaptation of an online portal and training, cancer nurses were asked to register patients to screen via the portal in clinic or at home. Symptoms were scored according to severity, and scores above cut-off were reported to nurses for assessment and management, according to best practice.
Results
Fifteen nurses working across diverse tumour types agreed to approach patients for screening. Of these, 7 nurses approached 68 patients, with 5 approaching more than 1 during the 7-month study period. Forty-seven (69%) patients completed screening, and 22 rescreened at least once. At first screening, 33 (70%) patients reported at least one symptom, most commonly tiredness (n = 27; 57%), reduced wellbeing (n = 24; 51%) and drowsiness (n = 17; 36%). Of the total 75 screens undertaken during the study, 56 (75%) identified at least one symptom, and 22 (29%) identified at least one severe symptom. All patients with a positive first screen were followed up by a nurse assessment and intervention—mostly reassurance (n = 19, 59%) or referral to another health professional (n = 11, 34%).
Conclusion
Screening for symptoms and needs using a web-based portal identified many unmet needs, but the uptake of this intervention by nurses and patients was lower than expected.
Similar content being viewed by others
Background
People with cancer experience high symptom burden [1, 2] which is associated with poorer quality of life, high health service utilisation and shorter survival [3]. Research shows that many symptoms and needs, in particular psychosocial needs, remain undetected and unaddressed [4]. Consequently, guidelines recommend routine screening for symptoms and unmet needs in people with cancer [5].
Patient-reported outcome (PRO) collection using a validated scale, such as the Edmonton Symptom Assessment Scale (ESAS) [6], offers an evidence-based approach to screening for symptom burden that is brief and can be done electronically or in print. Screening with ESAS has been associated with improved patient satisfaction, reduced hospital emergency room presentations and improved survival [6, 7]. But in Australia, as in many countries, neither screening for symptoms and needs nor the use of PROs as a method of systematic screening have been adopted into routine clinical practice [8]. Data on the feasibility and acceptability of these approaches in routine care are required to guide future implementation efforts.
The aim of this study was to evaluate the implementation of a web-based system of screening for symptoms and needs using the ESAS in people with diverse cancers in a tertiary referral hospital in Australia. Specifically, the objectives of the study were to (1) evaluate the feasibility and acceptability of a web-based platform for screening for symptoms and needs in patients across diverse tumour streams and (2) describe the symptoms detected by screening and their management.
Methods
This was a prospective, single-arm, pragmatic intervention study conducted across all tumour streams at a tertiary referral hospital in metropolitan Adelaide, South Australia. The hospital provides comprehensive cancer services to adult patients living in the South of Adelaide and adjacent rural areas, servicing a population of approximately 360,000 people.
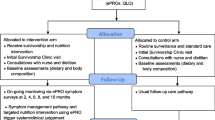
The intervention involved a web-based screening using the ESAS measure to screen for symptoms and needs. The ESAS is a validated instrument developed to rapidly assess nine different symptoms: pain, nausea, reduced appetite, reduced wellbeing, shortness of breath, tiredness, drowsiness, anxiety and depression. Patients are asked to indicate the intensity at which they experience each symptom from 0 (not experiencing the symptom at all) to 10 (worst possible) [9]. ESAS is accompanied by a problem checklist listing potential emotional, information social/family, practical, spiritual and physical concerns that the patient may also identify as an unmet need [10]. Screening was conducted using a purpose-built web portal (iSCREEN) adapted from the online portal developed by the Australian Psycho-Oncology Cooperative Research Group to screen for anxiety and depression using ESAS [11, 12]. Once the patient registered and completed the first screening, subsequent screens were automatically initiated at 3 monthly intervals although the interval could be modified by the nursing staff initiating the screen.
Nurses working in the role of a cancer care coordinators were invited by their senior managers to use the portal for screening for symptoms and needs as part of their routine clinical care. Adult patients receiving care for cancer at any stage were eligible to be invited by the nurse to be screened using the portal. Patients were not invited to participate if they could not use the portal, e.g. were too unwell, or had literacy or language barriers.
Nurse received one-on-one training from research staff, which included setting up the portal parameters to their individual work requirements. Nurses initiated discussions of screening for symptoms and needs with their patients. As screening was considered the best practice routine care, no patient consent for screening was required. If the patient was willing to be screened, the patient was given an option of consenting to researcher review of medical records to collect any missing data, such as the action taken to address the identified symptom(s). If the patient declined medical record access, the screening could still proceed, but no records were reviewed. Patients and nurses were invited to provide feedback on the portal using a semi-structured interview and questionnaire (nurses only).
The primary outcome was feasibility, defined as the ratio of screened (patients who completed the ESAS using the portal) to registered (patients registered on the portal and sent an invitation to screen), with the feasibility threshold set at 75%. The choice of the 75% cut-off was a pragmatic decision taking into account the need for high adherence to ensure clinical significance as well as expectation of high adherence in the context of a single institution study. Secondary outcomes included the proportion of new patients who had an identified need assessed and required management and the proportion of patients who were rescreened, as well as the prevalence and types of symptoms, needs and referral rates once symptoms were identified, time spent using the portal and acceptability of the process to patients and nurses.
Data management and statistical analyses were performed using Stata version 16.1 (StataCorp LP, College Station, TX, USA). Primary and secondary outcomes were expressed as absolute and relative frequencies for categorical variables. Median and interquartile ranges (IQR) were reported for continuous skewed data/scores. Interviews were audio-recorded and transcribed verbatim. This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Southern Adelaide Local Health Network Human Research Ethics Committee (application 2020/HRE00633).
Results
Fifteen of 16 nurses employed at the hospital in a cancer coordinator role indicated willingness to invite patients for screening with seven (47%) using iSCREEN over the duration of the study. During the period of recruitment from December 2020 to June 2021, 68 patients (median age = 57 years, IQR 51:69) were registered for screening across six tumour streams. Of those, 47 (69%) completed screening. The majority of patients (n = 32; 47%) were registered by the breast cancer stream with 24 (75% of those registered) screened. Twenty-six patients (38% of all registered) were registered by the upper gastrointestinal (GI) tumour stream with 15 (58%) completing screening. The remaining eight patients were screened across prostate, head and neck, lung and cancer survivorship services, with the number of patients screened ranging from one to four.
Of the total of 75 screens undertaken during the study in 47 patients, 56 screens (75%) identified at least one symptom (24% of screens identified severe symptoms) with 33 of 47 patients screened (70%) reporting at least one symptom at first screening. Twenty-eight patients were scheduled for a second screen during the study period, and 22 (79%) completed this second screen. The remaining patients’ second screen, scheduled to take place 3 months from the initial, was due after the study has been completed. For 17 (77%) of those, at least one moderate or severe problem was recorded, and eight (47%) of those were assessed by a nurse. Five patients completed a third screen (of which four reported symptoms) and one screened a fourth time. Overall, 75 screens were performed, of which 54 (72%) identified at least one moderate or severe symptom. Nurses completed assessments and recorded actions to address symptoms or needs for 44 (82%) of the positive screens. The actions taken by nurses in response to symptoms included reassurance (28; 64% of all positive screens reviewed), referral to another professional (n = 11; 25%) or earlier clinic review (9; 20%). For some positive screens, nurses arranged more than one intervention.
Figures 1 and 2 summarise the symptoms and problems identified at patients’ first screen. A total of 123 moderate or severe symptoms were identified via the ESAS at first screen in 33 patients. Fifteen patients (32%) reported at least one severe symptom. The median number of symptoms reported at first screen was four (IQR 1:5). Three patients (6%) reported only one symptom, 12 (26%) two to three and 18 (38%) four or more. The most common symptoms reported at first screen included tiredness (n = 27; 57%), reduced wellbeing (n = 24; 51%) and drowsiness (n = 17; 36%). At the first screen, the problem checklist identified 216 problems in 38 patients, with the most common including fears and worries (n = 23; 49%), sleep problems (n = 23; 49%), weight problems (n = 18; 38%) and changes in appearance (n = 16; 34%). Over multiple screens, there were improvements in scores for 59 (69%) symptoms identified at first screen, with 16 (19%) remaining unchanged and 10 (12%) worsening. Figure 3 summarises changes in severity of the three most common symptoms (tiredness, reduced wellbeing drowsiness) who screened more than once.
ESAS scores for 3 most prevalent symptoms in participants completing multiple screens. Each line represents scores for an individual patient across multiple screen intervals. Low score = less severe symptom. A Tiredness; B reduced wellbeing; C drowsiness. Red line = median score for each screening occasion
Of the seven nurses who registered patients, five completed questions about time spent using the portal. The median time taken to use the portal was estimated as 23 min per patient (range 13–50 min) with the most time-consuming task being in-clinic screening with the patient. All respondents estimated it took them less than 5 min to assess patients’ eligibility to use the portal and less than 5 min to introduce the portal to patients. Two nurses took less than 5 min to register a patient, two took 5–10 min and one 11–20 min. Two nurses assisted patients to complete screening (other patients completed their screening electronically)—one reported spending 5 min and the other 25 min. All nurses indicated reading email notifications took them less than 5 min.
Seven nurses (five who registered patients for the portal and two who did not) completed questionnaires on acceptability followed by four completing interviews lasting between 10 and 20 min. Three nurses identified limited access to computers as a barrier and were provided with an electronic tablet. Two of these subsequently registered patients, but the third nurse did not. One tumour stream did not have a dedicated nurse coordinator, and the study appointed a senior nurse to fulfil this role in the service 1 day per week for the study period. This approach did not result in any registrations. Of the five nurses who registered patients, three were satisfied with the screening system, one was not, and one was neither satisfied nor dissatisfied. Of the two who did not register patients, one was satisfied and one not satisfied with the portal. Four nurses (three of whom registered patients) found the portal easy to use, but others referred to it as “clunky” and difficult to navigate. Other barriers to nurse-use included lack of time and dedicated private space to introduce the portal and/or assist patients with screening. Nurses perceived that patients may be concerned about data storage on the Internet and difficulties using technology. One nurse felt screening was not within their role/responsibility and another that the screening approach was not appropriate for all patients. Two raised concerns that initial cancer diagnosis was not the right time to screen, as patients would have a lot of symptoms that would resolve without intervention. Two nurses perceived their “typical” patients’ demographics meant they were unlikely to engage with technology and research. Two preferred for a screening tool tailored to the needs of the cancer type they managed. Suggestions for improvements from nurses included automation of registration or registration by clinic administration staff and link to hospital electronic medical record.
Of four patients who completed interviews, two identified no barriers to use, but others highlighted the need for clearer instructions for use. One patient indicated they did not find the portal “particularly attractive or engaging”. Patients valued the portal for the opportunity to provide information without burdening cancer care coordinators, but remaining connected, between appointments. One patient reflected on their difficulty admitting they were struggling and articulating their concerns. Unlike nurse coordinators, patients did not raise concerns about privacy of data.
Discussion
This pragmatic, real-world implementation study of a web-based platform for screening for symptoms and needs in people with cancer did not meet its primary feasibility objective. That is, while 69% of registered patients used the portal for screening, this fell short of the 75% threshold set a priori. It was also notable that only 47% of cancer care coordinators who agreed to participate used the portal. More promisingly, five of the seven nurses who did use the portal did so repeatedly. Nurses were responsive when needs were identified, with 86% of patients with symptoms assessed. Of those patients who used the portal, the majority had symptoms, but most symptoms did not require extensive intervention suggesting that symptoms detected early may be addressed without excessive demand on resources.
These findings offer an insight into the real-world implementation of a practice change with some important lessons. Firstly, the uptake across different services and individual nurses varied with only two services adopting the approach early and integrating it into their regular workflow. The highest uptake by both nurses and patients occurred in breast cancer which has the longest tradition of nurse coordinator roles and a high proportion of motivated and educated patients. It is possible the short duration of the study was not sufficient to impact practice of those nurses who were not early adopters. Furthermore, the study was conducted during the COVID-19 pandemic (with a rapid associated transition to telehealth platforms) and a state-wide roll out of an electronic health record; thus, iSCREEN represented a third simultaneous technology-related service change being implemented adding to nurses’ workload, change-fatigue and perhaps “digital health fatigue”. The study feasibility threshold was set at 75% which may have been set too high and was higher than in evaluations of many other complex interventions in similar patient populations where the acceptable threshold was set at 60% [13, 14].
Nurses identified several barriers to recruitment including time and access to private space. For some barriers, such as access to tablets or dedicated time, additional resources did not significantly increase registrations suggesting that other barriers also need to be addressed. For example, nurses raised the issues of role definition as a barrier to screening, and appropriateness of the screening for their patients at a particular point in time (i.e. when cancer diagnosis had just occurred) as symptoms, especially distress, may be transient and spontaneously resolve. These findings suggest further training on the purpose, and benefits of screening would be required to increase uptake as well as clear clinical pathways clarifying roles and responsibilities and embedding screening into the routine workflow [15]. These observations are similar to the implementation of the ADAPT portal on which the iSCREEN portal was based [16, 17] and other studies investigating PRO use in cancer care [18]. The large variance in the time taken to use the portal by nurses may reflect a range of factors including the digital health literacy of the nurses, familiarity with the screening process and possibly the perception of time spent as the reporting was subjective.
It is worth noting that nearly a third of patients who indicated willingness to screen did not complete screening, and 21% of those contacted for rescreen did not rescreen. There are several potential explanations for low patient engagement. Firstly, patients may not engage if they sense limited endorsement from the clinical service or cancer care coordinators introducing screening. This hypothesis is supported by our observation that the rescreen rate was higher for patients managed by the two services with high rates of registration and screening, where nurses were recommending screening frequently. In this study, nurses took on the role of introducing and coordinating screening for all patients. Perhaps a more whole-of-service approach with endorsement and reinforcement of all members of the cancer care team would have provided additional motivation for patients to screen, by emphasising its importance across multiple encounters. Secondly, it is possible that the portal was not sufficiently user friendly or engaging to patients who indicated their willingness to use it while in clinic but did not follow it up once at home (especially given comments from patients about the need for clearer instructions for portal use). Such instructions could be provided using a range of approaches including written instructions, videos or digital learning modules, depending on user preferences. Similarly, additional training resources could be of value to the nurses. Currently, the portal offers screening only in English, making this approach unavailable for people of non-English speaking backgrounds. This barrier may be overcome by staff assisting patients to screen in clinic, but only three patients were screened with the assistance of the nurse in the present study. Future research needs to focus on how to make self-directed screening acceptable and feasible, especially for those patients with limited health and digital literacy and those with a higher symptom burden for whom completing screening may be more difficult. Other studies using PROs have shown lower use among patients who are more unwell/have higher symptom burden who may benefit from screening more [19, 20], further underscoring the importance of the health care provider support.
Implementation science theory emphasises a multilevel approach to PRO implementation addressing the PRO intervention itself, policy context, implementation climate in the health care setting, clinical teams and the implementation process and the importance of tailored approaches to implementation that are based on local context [21]. Similarly, the emerging concept of a learning health system includes the recognition of multiple elements of such a system and multiple enablers to its use, including workforce, data systems, resources and organisational culture [22]. The findings of the present study are consistent with these theoretical considerations and highlight the complexity of the implementation process with nurses offering suggestions for improvement that related to the intervention itself (such as automation of registration), the team roles (using clinic administration staff to register patients) and the implementation process (using the link to the hospital electronic medical record as a trigger for screening). A recent Delphi study of strategies for implementation conducted with input from patients, clinicians, researchers and technology developers offers an example of steps required to implement patient-reported outcomes in clinical cancer care [23]. In line with these steps, further adoption of the iSCREEN system needs to focus on assessment, and boosting, of readiness for implementation of PRO screening; identification and addressing of barriers to use for patients and health care providers; embedding the screening into the routine workflow; and ongoing monitoring of performance to further refine and adapt.
Our study has significant limitations—it was conducted during the COVID-19 pandemic and as a result had an unexpectedly brief recruitment period which made commitment to the study for nurses more difficult. Future implementation of PRO screening in cancer care needs a long-term engagement with stakeholders and clinical teams and embedding of the PRO collection into the existing workflows and communication systems, such as electronic medical record, to reduce the burden of data collection and to ensure changes are supported by users and are sustainable.
In conclusion, screening for symptoms and needs using a web-based PRO collection portal identified a high number of symptoms in patients with diverse cancers which may otherwise have been missed and facilitated referral and care, but the uptake of this intervention by nurses and patients was lower than expected. Our study adds to the body of evidence highlighting the complexity of practice change in the real-world setting and highlights areas requiring further attention to improve future uptake of similar interventions.
Data availability
Data are available from the authors upon reasonable request.
References
Moghaddam N, Coxon H, Nabarro S, Hardy B, Cox K (2016) Unmet care needs in people living with advanced cancer: a systematic review. Support Care Cancer 24(8):3609–3622
Burg MA, Adorno G, Lopez ED, Loerzel V, Stein K, Wallace C et al (2015) Current unmet needs of cancer survivors: analysis of open-ended responses to the American Cancer Society Study of Cancer Survivors II. Cancer 121(4):623–630
Newcomb RA, Nipp RD, Waldman LP et al (2020) Symptom burden in patients with cancer who are experiencing unplanned hospitalization. Cancer 126(12):2924–2933
Skaczkowski G, Sanderson P, Shand M et al (2018) Factors associated with referral offer and acceptance following supportive care problem identification in a comprehensive cancer service. Euro J Cancer Care 27(5):e12869
Carlson LE, Waller A, Mitchell AJ (2012) Screening for distress and unmet needs in patients with cancer: review and recommendations. J Clin Oncol 30(11):1160–1177. https://doi.org/10.1200/JCO.2011.39.5509
Barbera L, Sutradhar R, Seow H, Mittmann N, Howell D, Earle CC et al (2020) The impact of routine Edmonton Symptom Assessment System (ESAS) use on overall survival in cancer patients: results of a population-based retrospective matched cohort analysis. Cancer Med 9(19):7107–7115
Girgis A, Durcinoska I, Levesque JV et al (2017) The PROMPT-Care Program Group eHealth system for collecting and utilizing patient reported outcome measures for personalized treatment and care (PROMPT-Care) among cancer patients: mixed methods approach to evaluate feasibility and acceptability. J Med Internet Res 19(10):e330
Clinical Oncology Society of Australia Patient Reported Outcomes Working G, Koczwara B, Bonnamy J, Briggs P, Brown B, Butow PN et al (2021) Patient-reported outcomes and personalised cancer care. Med J Australia. 214(9):406–8 e1
Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K (1991) The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care. 7(2):6–9
Ashbury FD, Findlay H, Reynolds B, McKerracher K (1998) A Canadian survey of cancer patients’ experiences: are their needs being met? J Pain Symptom Manag 16:298–306
Butow P, Price MA, Shaw JM, Turner J, Clayton JM, Grimison P, Rankin N, Kirsten L (2015) Clinical pathway for the screening, assessment and management of anxiety and depression in adult cancer patients: Australian guidelines. Psychooncology 24:987–1001
Butow P, Shaw J, Shepherd HL, Price M, Masya L, Kelly B, Rankin NM, Girgis A, Hack TF, Beale P, Viney R, Dhillon HM, Coll J, Kelly P, Lovell M, Grimison P, Shaw T, Luckett T, Cuddy J, White F, ADAPT Program Group (2018) Comparison of implementation strategies to influence adherence to the clinical pathway for screening, assessment and management of anxiety and depression in adult cancer patients (ADAPT CP): study protocol of a cluster randomised controlled trial. BMC Cancer. 18(1):1077
Eakin EG, Reeves MM, Goode AD et al (2020) Translating research into practice: outcomes from the Healthy Living after Cancer partnership project. BMC Cancer 20:963
Crockett C, Gomes F, Faivre-Finn C, Howell S, Kasipandian V, Smith E, Thomson D, Yorke J, Price J (2021) The routine clinical implementation of electronic patient-reported outcome measures (ePROMs) at the christie NHS foundation trust. Clin Oncol (R Coll Radiol) 33(12):761–764
Butow PN, Shepherd HL, Cuddy J, Harris M, He S, Masya L, Rankin NM, Grimison P, Girgis A, Shaw JM (2021) The ADAPT Program Group from ideal to actual practice: tailoring a clinical pathway to address anxiety or depression in patients with cancer and planning its implementation across individual clinical services. J Psychosocial Oncol Res Pract 3(4):e061
Masya L, Shepherd HL, Butow P, Geerligs L, Allison KC, Dolan C, Prest G (2021) The ADAPT Program Group, Shaw J Impact of individual, organizational, and technological factors on the implementation of an online portal to support a clinical pathway addressing psycho-oncology care: mixed methods study JMIR. Hum Factors 8(2):e26390
Rankin NM, Butow PN, Thein T, Robinson T, Shaw JM, Price MA et al (2015) Everybody wants it done but nobody wants to do it: an exploration of the barrier and enablers of critical components towards creating a clinical pathway for anxiety and depression in cancer. BMC Health Serv Res 15:28
Graupner C, Kimman ML, Mul S et al (2021) Patient outcomes, patient experiences and process indicators associated with the routine use of patient-reported outcome measures (PROMs) in cancer care: a systematic review. Support Care Cancer 29:573–593
Nielsen AS, Kidholm K, Kayser L (2020) Patients’ reasons for non-use of digital patient-reported outcome concepts: A scoping review. Health Informatics J 26(4):2811–2833. https://doi.org/10.1177/1460458220942649
Agarwal V, Corsini N, Eckert MC et al (2021) A pilot study of population-based, patient-reported outcome collection in cancer survivors. Support Care Cancer 9(8):4239–4247
Stover AM, Haverman L, van Oers HA, Greenhalgh J, Potter CM (2021) ISOQOL PROMs/PREMs in clinical practice implementation science work group. Using an implementation science approach to implement and evaluate patient-reported outcome measures (PROM) initiatives in routine care settings. Qual Life Res 30(11):3015–3033
Easterling D, Perry AC, Woodside R, Patel T, Gesell SB (2021) Clarifying the concept of a learning health system for healthcare delivery organizations: Implications from a qualitative analysis of the scientific literature. Learn Health Syst 6(2):e10287
Mazariego C, Jefford M, Chan RJ, Roberts N, Millar L, Anazodo A, Hayes S, Brown B, Saunders C, Webber K, Vardy J, Girgis A, Koczwara B (2022) COSA PRO working group. Priority recommendations for the implementation of patient-reported outcomes in clinical cancer care: a Delphi study. J Cancer Surviv 16(1):33–43
Funding
This work was supported by the Hospital Research Foundation Grant.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Reegan Knowles and Shahid Ullah. The first draft of the manuscript was written by Bogda Koczwara, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Approval was granted by the Southern Adelaide Local Health Network Human Research Ethics Committee (application 2020/HRE00633).
Consent to participate
As screening was considered the best practice routine care, no patient consent for screening was required. If the patient was willing to be screened, the patient was given an option of consenting to researcher review of medical records to collect any missing data, such as the action taken to address the identified symptom(s). If the patient declined medical record access, the screening could still proceed, but no records were reviewed.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Koczwara, B., Knowles, R., Beatty, L. et al. Implementing a web-based system of screening for symptoms and needs using patient-reported outcomes in people with cancer. Support Care Cancer 31, 69 (2023). https://doi.org/10.1007/s00520-022-07547-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-022-07547-9