Abstract
Purpose
Healthcare systems contribute to disparities in breast cancer outcomes. Patient navigation is a widely cited system-based approach to improve outcomes among populations at risk for delays in care. Patient navigation programs exist in all major Boston hospitals, yet disparities in outcomes persist. The objective of this study was to conduct a baseline assessment of navigation processes at six Boston hospitals that provide breast cancer care in preparation for an implementation trial of standardized navigation across the city.
Methods
We conducted a mixed methods study in six hospitals that provide treatment to breast cancer patients in Boston. We administered a web-based survey to clinical champions (n = 7) across six sites to collect information about the structure of navigation programs. We then conducted in-person workflow assessments at each site using a semi-structured interview guide to understand site-specific implementation processes for patient navigation programs. The target population included administrators, supervisors, and patient navigators who provided breast cancer treatment-focused care.
Results
All sites offered patient navigation services to their patients undergoing treatment for breast cancer. We identified wide heterogeneity in terms of how programs were funded/resourced, which patients were targeted for navigation, the type of services provided, and the continuity of those services relative to the patient’s cancer treatment.
Conclusions
The operationalization of patient navigation varies widely across hospitals especially in relation to three core principles in patient navigation: providing patient support across the care continuum, targeting services to those patients most likely to experience delays in care, and systematically screening for and addressing patients’ health-related social needs. Gaps in navigation across the care continuum present opportunities for intervention.
Trial registration
Clinical Trial Registration Number NCT03514433, 5/2/2018

Similar content being viewed by others
References
Byers T (2010) Two decades of declining cancer mortality: progress with disparity. Annu Rev Public Health 31:121–132. https://doi.org/10.1146/annurev.publhealth.121208.131047
DeSantis CE, Ma J, Gaudet MM, Newman LA, Miller KD, Goding Sauer A et al (2019) Breast cancer statistics, 2019. CA Cancer J Clin 69:438–451. https://doi.org/10.3322/caac.21583
Ramirez A, Perez-Stable E, Penedo F, Talavera G, Carrillo JE, Fernández M et al (2014) Reducing time-to-treatment in underserved Latinas with breast cancer: the six cities study. Cancer 120:752–760. https://doi.org/10.1002/cncr.28450
Rodday AM, Parsons SK, Snyder F, Simon MA, Llanos AAM, Warren-Mears V et al (2015) Impact of patient navigation in eliminating economic disparities in cancer care. Cancer 121:4025–4034. https://doi.org/10.1002/cncr.29612
Ko NY, Snyder FR, Raich PC, Paskett ED, Dudley DJ, Lee J-H et al (2016) Racial and ethnic differences in patient navigation: results from the patient navigation research program. Cancer 122:2715–2722. https://doi.org/10.1002/cncr.30109
Rocque GB, Williams CP, Jones MI, Kenzik KM, Williams GR, Azuero A et al (2018) Healthcare utilization, Medicare spending, and sources of patient distress identified during implementation of a lay navigation program for older patients with breast cancer. Breast Cancer Res Treat 167:215–223. https://doi.org/10.1007/s10549-017-4498-8
Hunt BR, Whitman S, Hurlbert MS (2014) Increasing Black:White disparities in breast cancer mortality in the 50 largest cities in the United States. Cancer Epidemiol 38:118–123. https://doi.org/10.1016/j.canep.2013.09.009
Bernardo BM, Zhang X, Hery CMB, Meadows RJ, Paskett ED (2019) The efficacy and cost-effectiveness of patient navigation programs across the cancer continuum: a systematic review. Cancer 125:2747–2761. https://doi.org/10.1002/cncr.32147
Baik SH, Gallo LC, Wells KJ (2016) Patient navigation in breast cancer treatment and survivorship: a systematic review. J Clin Oncol 34:3686–3696. https://doi.org/10.1200/JCO.2016.67.5454
Freeman HP, Rodriguez RL (2011) The history and principles of patient navigation. Cancer 117:3539–3542. https://doi.org/10.1002/cncr.26262
Freund KM, Battaglia TA, Calhoun E, Darnell JS, Dudley DJ, Fiscella K et al (2014) Impact of patient navigation on timely cancer care: the patient navigation research program. J Natl Cancer Inst 106:dju115. https://doi.org/10.1093/jnci/dju115
Braun KL, Kagawa-Singer M, Holden AE, Burhansstipanov L, Tran JH, Seals BF et al (2012) Cancer patient navigator tasks across the cancer care continuum. J Health Care Poor Underserved 23:398–413. https://doi.org/10.1353/hpu.2012.0029
Medina-Jaudes N (2017) Patient navigation effectiveness on improving cancer screening rates: a meta-analysis of randomized controlled trials
Battaglia TA, Bak SM, Heeren T, Chen CA, Kalish R, Tringale S et al (2012) Boston patient navigation research program: the impact of navigation on time to diagnostic resolution after abnormal cancer screening. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 21:1645–1654. https://doi.org/10.1158/1055-9965.EPI-12-0532
Freund KM, Battaglia TA, Calhoun E, Dudley DJ, Fiscella K, Paskett E et al (2008) National Cancer Institute Patient Navigation Research Program: methods, protocol, and measures - PubMed. Cancer 113:3391–3399
Gunn CM, Clark JA, Battaglia TA, Freund KM, Parker VA (2014) An assessment of patient navigator activities in breast cancer patient navigation programs using a nine-principle framework. Health Serv Res 49:1555–1577. https://doi.org/10.1111/1475-6773.12184
Whitley EM, Raich PC, Dudley DJ, Freund KM, Paskett ED, Patierno SR et al (2017) Relation of comorbidities and patient navigation with the time to diagnostic resolution after abnormal cancer screening. Cancer 123:312–318. https://doi.org/10.1002/cncr.30316
Ko NY, Darnell JS, Calhoun E, Freund KM, Kristin J (2014) Wells, Shapiro CL, et al. Can patient navigation improve receipt of recommended breast cancer care? Evidence From the National Patient Navigation Research Program. J Clin Oncol 32:2758–2764
Freeman HP (2006) Patient navigation: a community centered approach to reducing cancer mortality. J Cancer Educ Off J Am Assoc Cancer Educ 21:S11–S14. https://doi.org/10.1207/s15430154jce2101s_4
Commission on Cancer (2016) Cancer Program Standards: Ensuring Patient-Centered Care. American College of Surgeons, Chicago
Oncology Nursing Society (2017) Oncology nurse navigator core competencies. Oncol Nurs Forum 45:283. https://doi.org/10.1188/18.ONF.283
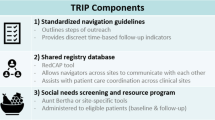
Battaglia TA, Freund KM, Haas JS, Casanova N, Bak S, Cabral H et al (2020) Translating research into practice: protocol for a community-engaged, stepped wedge randomized trial to reduce disparities in breast cancer treatment through a regional patient navigation collaborative. Contemp Clin Trials 93:106007. https://doi.org/10.1016/j.cct.2020.106007
Freund KM, Haas JS, Lemon SC, White KB, Casanova N, Dominici LS et al (2019) Standardized activities for lay patient navigators in breast cancer care: recommendations from a citywide implementation study. Cancer 125:4532–4540. https://doi.org/10.1002/cncr.32432
Boston Breast Cancer Equity Coalition. Boston Breast Cancer Equity Coalition. n.d. URL: https://bostonbcec.org (Accessed 28 April 2021).
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC (2009) Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 4:50. https://doi.org/10.1186/1748-5908-4-50
Casanova NL, LeClair AM, Xiao V, Mullikin KR, Lemon SC, Freund KM, et al. (In press) Development of a workflow process mapping protocol to inform the implementation of patient navigation programs in breast oncology. Cancer
Agency for Healthcare Research and Quality (2014) Chapter 3. Care coordination measurement framework. URL: https://www.ahrq.gov/ncepcr/care/coordination/atlas/chapter3.html (Accessed 27 January 2021)
Gunn C, Battaglia TA, Parker VA, Clark JA, Paskett ED, Calhoun E et al (2017) What makes patient navigation most effective: defining useful tasks and networks. J Health Care Poor Underserved 28:663–676. https://doi.org/10.1353/hpu.2017.0066
American College of Surgeons (2021) Optimal resources for cancer care: 2020 Standards
Garg A, Byhoff E, Wexler MG (2020) Implementation considerations for social determinants of health screening and referral interventions. JAMA Netw Open 3:e200693. https://doi.org/10.1001/jamanetworkopen.2020.0693
Page-Reeves J, Kaufman W, Bleecker M, Norris J, McCalmont K, Ianakieva V et al (2016) Addressing social determinants of health in a clinic setting: the WellRx pilot in Albuquerque, New Mexico. J Am Board Fam Med 29:414–418. https://doi.org/10.3122/jabfm.2016.03.150272
Gottlieb LM, Hessler D, Long D, Laves E, Burns AR, Amaya A et al (2016) Effects of social needs screening and in-person service navigation on child health: a randomized clinical trial. JAMA Pediatr 170:e162521–e162521. https://doi.org/10.1001/jamapediatrics.2016.2521
Association of Community Cancer Centers (2009) Cancer care patient navigation: a practical guide for community cancer centers. Assoc Community Cancer Cent.
Acknowledgements
The authors would like to acknowledge the partnership of TRIP’s stakeholders and community organizations: Boston Patient Navigator Network, Boston Breast Cancer Equity Coalition, Boston Public Health Commission: Pink & Black, Massachusetts Department of Public Health: Office of Community Health Workers; The National Center to Advance Translational Science, the Boston University Clinical and Translational Science Institute (CTSI), University of Massachusetts CTSI, the Harvard CTSI, Tufts CTSI; our partner institutions Boston Medical Center, Brigham and Women’s Faulkner Hospital, Massachusetts General Hospital, Tufts Medical Center, Beth Israel Deaconess Medical Center, and Dana Farber Cancer Institute; and finally the TRIP Consortium and our patient navigators.
Translating Research Into Practice (TRIP) Consortium
-
Beth Israel Deaconess Medical Center (Ted A. James MD, Susan McCauley RN, Ellen Ohrenberger RN BSN, JoEllen Ross RN BSN, Leo Magrini BS)
-
Boston Breast Cancer Equity Coalition Steering Committee (Susan T. Gershman MS MPH PhD CTR, Mark Kennedy MBA, Anne Levine MEd MBA, Erica T. Warner ScD MPH)
-
Brigham and Women’s Hospital (Cheryl R. Clark MD ScD)
-
Boston Medical Center (William G. Adams MD, Sharon Bak MPH, Nicole Casanova BA, Katie Finn BA, Christine Gunn PhD, Naomi Y. Ko MD, Ariel Maschke MA, Katelyn Mullikin BA, Laura Ochoa BA, Christopher W. Shanahan MD MPH, Samantha Steil BA, Tracy A. Battaglia MD MPH, Victoria Xiao BS)
-
Boston University (Howard J. Cabral PhD MPH, Clara Chen MHS, Carolyn Finney BA, Christine Lloyd-Travaglini MPH, Stephanie Loo MSc)
-
Dana-Farber Cancer Institute (Magnolia Contreras MSW MBA, Rachel A. Freedman MD MPH, Yoscairy Raymond BSW CCHW, Deborah Toffler MSW LCSW)
-
Dana-Farber/Harvard Cancer Center (Karen Burns White MS)
-
Equal Hope (Anne Marie Murphy PhD)
-
Massachusetts General Hospital (Carmen Benjamin MSW, Beverly Moy MD, Jennifer S. Haas MD MPH, Caylin Marotta MPH, Aileen Navarrete BA, Sanja Percac-Lima MD PhD, Emma Whited BA, Amy J Wint MSc)
-
Tufts Medical Center (Karen M. Freund MD MPH, William F. Harvey MD MSc, Danielle Krzyszczyk BA, Amy M. LeClair PhD MPhil, Susan K. Parsons MD MRP, Feng Qing Wang BA)
-
University of Massachusetts Lowell (Serena Rajabiun MA MPH PhD)
-
University of Massachusetts Medical School (Stephenie C. Lemon PhD)
NOGA
-
Award Number U01TR002070
-
The National Center For Advancing Translational Sciences
-
The Office of Behavioral and Social Sciences Research of the National Institutes of Health
-
NIH CTSA Awards
-
Harvard: UL1TR002541
-
Tufts: ULTR002544
-
Boston University: UL1TR001430
-
University of Massachusetts Medical School: UL1TR001453
American Cancer Society #CRP-17-112-06-COUN
Funding
Research reported in this publication was supported by the National Center for Advancing Translational Sciences and the Office of Behavioral and Social Sciences Research of the National Institutes of Health under Award Number U01TR002070. Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under the Harvard University CTSA Award Number UL1TR002541, Tufts University CTSA Award Number UL1TR002544, Boston University CTSA Award Number 1UL1TR001430, and University of Massachusetts CTSA Award Number UL1 TR001453-03.
Author information
Authors and Affiliations
Contributions
Amy M. LeClair: Conceptualization, methodology, writing-original draft, writing-review, editing, project administration
Tracy A. Battaglia: Conceptualization, funding acquisition, methodology, project administration, resources, supervision, validation, writing-review, editing
Nicole L. Casanova: Conceptualization, methodology, writing-original draft, writing-review, editing, project administration
Jennifer S. Haas: Conceptualization, funding acquisition, methodology, project administration, resources, supervision, validation, writing-review, editing
Karen M. Freund: Conceptualization, funding acquisition, methodology, project administration, resources, supervision, validation, writing-review, editing
Beverly Moy: Conceptualization, resources, validation, final review
Susan K. Parsons: Conceptualization, resources, validation, final review
Naomi Y. Ko: Conceptualization, resources, validation, final review
JoEllen Ross: Investigation, writing-review, editing
Ellen Ohrenberger: Investigation, writing-review, editing
Katelyn R. Mullikin: Writing-review, editing
Stephenie C. Lemon: Conceptualization, funding acquisition, methodology, project administration, resources, supervision, validation, writing-review, editing
Corresponding author
Ethics declarations
Ethics approval
The present study received institutional review board approval from the Boston University Medical Center/Boston Medical Center Institutional Review Board (IRB# H-37314). The study’s formative work, described in this paper, was given a Non-Human Subjects Research designation, as the goal was to create a generalizable protocol for navigation process planning and improvement.
Consent to participate
The study’s formative work was given a Non-Human Subjects Research designation, and therefore, participants were not required to be consented.
Consent for publication
The study’s formative work was given a Non-Human Subjects Research designation, and therefore participants, were not required to be consented.
Conflict of interest
Author Karen M. Freund received funding from the American Cancer Society: American Cancer Society #CRP-17-112-06-COUN. The authors have no other funding or conflicts of interest to report.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix A. Clinical Advisory Panel Survey about Navigation Program
Appendix A. Clinical Advisory Panel Survey about Navigation Program
Name
Institution
Patient Navigation
-
1.
Does your hospital provide patient navigation for any patients with breast cancer care during active treatment?
Navigators
-
2.
Are there different navigators at different phases of care (e.g. screening, diagnostic care, cancer care?)
-
3.
About how many clinical FTE patient navigators are focused specifically on breast cancer patients undergoing active treatment
-
4.
What is the educational background of the navigator(s) at your practice involved with breast cancer patients?
-
5.
What criteria are used to determine which patients are offered patient navigators?
-
6.
Which is the most common point of the patient's care process when navigators are brought into care?
-
7.
How are the navigators at your practice assigned patients during active cancer treatment?
-
8.
What is the most common way navigators are assigned patients?
-
a.
By referral of clinicians (physicians, nurses, SW)
-
b.
From a list of new patients or referrals
-
c.
Tumor board
-
d.
Other
-
a.
-
9.
How many patients does each navigator typically follow?
-
10.
What is the most common method by which patients are contacted?
-
11.
Who supervises the navigators?
-
12.
Supervisor's background
-
13.
What department is the navigator appointed under?
-
14.
What funding sources pay for breast cancer navigators at your practice?
Navigation tools
-
15.
What tools do navigators use to keep track of who/what they are navigating?
-
16.
What tools do navigators use to decide which patient to work with on a day to day basis?
-
17.
What tools do navigators use to identify when a patient has not kept a scheduled appointment or test?
-
18.
Does anyone else (besides the patient navigator) track patients to make sure they return for care?
-
19.
How do navigators decide that a patient no longer needs navigation?
-
20.
How does your practice determine if patients have left your practice and transferred care to another health care system?
-
21.
Has your hospital implement sending ADT information on the Mass Information highway?
-
22.
Is there a timeline planned for implementing this?
Social Determinants of Health
-
23.
Do any breast cancer providers routinely screen for social determinants of health?
-
24.
Who does the screening for social determinants of health among breast cancer patients?
-
25.
Which patients are screened?
-
26.
When are patients screened?
-
27.
How often are patients screened?
-
28.
Which domains are patients screened for?
-
29.
How does your practice perform the screening?
-
30.
Which electronic platform/EMR/website does your practice use?
-
31.
Are referrals made based on these screenings?
-
32.
Which domains are prioritized?
-
a.
Employee assistance
-
b.
Child/elder are assistance/parenting
-
c.
Transportation
-
d.
Mental Health
-
e.
Domestic Violence
-
a.
-
33.
How does your practice refer patients for social determinants of health?
-
34.
How is the decision made on where to refer patients?
-
35.
Where does your practice get a list of resources for potential referrals?
-
36.
Do you have a system to track whether a patient has connected with a referral or needs further assistance?
-
37.
Who follows up with the patient after they are referred?
-
38.
If your practice is not currently screening, does your practice have any plans to start systematic screening in the next 12 months?
-
39.
Which domains do you plan to prioritize? Please rank the top 5 domains based on priority?
-
a.
Housing instability
-
b.
Education/literacy
-
c.
Child/elder care assistance/parenting
-
d.
Transportation
-
e.
Immigration
-
f.
Legal
-
g.
Physical Activity
-
h.
Addiction and recovery
-
i.
Mental Health
-
j.
Health insurance
-
k.
Domestic Violence
-
l.
Community Violence
-
m.
Food instability
-
a.
-
40.
How does your practice plan to perform the screening?
-
41.
Where does your practice plan to get a list of resources for potential referrals?
-
42.
Will you have a system to track whether a woman has connected with a referral or needs further assistance?
-
43.
Who will follow up with the patient after they are referred?
-
44.
Any other comments or features about your clinical setting or patient navigation program that you think might be relevant to the current project to implement a standard patient navigation process across all Boston hospitals?
Rights and permissions
About this article
Cite this article
LeClair, A.M., Battaglia, T.A., Casanova, N.L. et al. Assessment of patient navigation programs for breast cancer patients across the city of Boston. Support Care Cancer 30, 2435–2443 (2022). https://doi.org/10.1007/s00520-021-06675-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06675-y