Abstract
Purpose
Testicular cancer is the most common carcinoma in 20- to 40-year-old men. Eighty percent of patients with metastases achieve disease-free status with chemotherapy with or without surgical resection. Standard first-line chemotherapy is bleomycin, etoposide, and cisplatin (BEP) for three to four courses or etoposide and cisplatin (EP) for four courses. Forty percent of patients receiving chemotherapy will have permanently reduced sperm counts impairing future fertility. Sperm banking is an effective method of maintaining fertility. This retrospective study was performed to assess utilization and results from sperm banking, as well as the barriers to its use.
Methods
Patients 18 and older who had received chemotherapy were given a five-item questionnaire on follow-up visit. This questionnaire included a mix of quantitative and qualitative questions.
Results
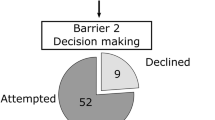
Two hundred patients enrolled in the study, and all 200 completed the questionnaire. Of the two hundred, 139 (70 %) patients chose not to bank sperm; 71 (51 %) of those were not interested, 25 (18 %) declined due to desire to start chemotherapy, 24 (17 %) were not offered, 12 (9 %) declined due to cost, and 7 (5 %) answered “other.” The average age at cancer diagnosis of patients who banked sperm was 28.4 as opposed to 32.6 for patients who did not (p = 0.003). The percentage of patients that had children before their diagnosis was 21 % in the sperm banking group, and 50 % in the group that did not (p = 0.0002). Sixty-one (30 %) chose to bank sperm; 11 of 61 patients (18 %) utilized the banked sperm; 9 of 11 (82 %) patients that utilized were successful; and 3 of 9 (33 %) successes resulted in multiple gestations.
Conclusions
Sperm banking provides the opportunity for paternity in testicular cancer patients with reduced sperm counts following treatment. However, the majority of these patients chose not to bank sperm or were not offered the opportunity. A range of factors such as time, emotional state, patient age, disease stage, prior children, institutional practices, and cost all influence whether banking is offered to patients and taken up. The authors provide recommendations to help clinicians overcome some of these barriers.


Similar content being viewed by others
References
Johnson MD, Cooper AR, Jungheim ES et al (2013) Sperm banking for fertility preservation: a 20-year experience. Eur J Obstet Gynecol Reprod Biol 170:177–182
Stoehr B, Schachtner L, Pichler R et al (2013) Influence of achieved paternity on quality of life in testicular cancer survivors. BJU Int 111:E207–E212
Brennemann W, Stoffel-Wagner B, Helmers A et al (1997) Gonadal function of patients treated with cisplatin based chemotherapy for germ cell cancer. J Urol 158:844–850
Stephenson WT, Poirier SM, Rubin L et al (1995) Evaluation of reproductive capacity in germ cell tumor patients following treatment with cisplatin, etoposide, and bleomycin. J Clin Oncol 13:2278–2280
Matos E, Skrbinc B, Zakotnik B et al (2010) Fertility in patients treated for testicular cancer. J Cancer Surviv 4:274–278
Hinton S, Catalano PJ, Einhorn LH et al (2003) Cisplatin, etoposide and either bleomycin or ifosfamide in the treatment of disseminated germ cell tumors. Cancer 97:1869–1875
Jahnukainen K, Ehmcke J, Hou M et al (2011) Testicular function and fertility preservation in male cancer patients. Best Pract Res Clin Endocrinol Metab 25:287–302
Lampe H, Horwich A, Norman A et al (1997) Fertility after chemotherapy for testicular germ cell cancers. J Clin Oncol 15:239–245
Lee SJ, Schover LR, Partridge AH et al (2006) American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol 24:2917–2931
Schover LR, Brey K, Lichtin A et al (2002) Oncologists’ attitudes and practices regarding banking sperm before cancer treatment. J Clin Oncol 20:1890–1897
Neal MS, Nagel K, Duckworth J et al (2007) Effectiveness of sperm banking in adolescents and young adults with cancer: a regional experience. Cancer 110:1125–1129
Nahata L, Cohen LE, Yu RN et al (2012) Barriers to fertility preservation in male adolescents with cancer: it's time for a multidisciplinary approach that includes urologists. Urology 79:1206–1209
Magelssen H, Haugen T, von During V et al (2005) Twenty years experience with semen cryopreservation in testicular cancer patients: who needs it? Eur Urol 48:779–785
Schover LR, Brey K, Lichtin A et al (2002) Knowledge and experience regarding cancer, infertility, and sperm banking in younger male survivors. J Clin Oncol 20:1880–1889
Acknowledgments
Dr. Einhorn was supported in part by the National Cancer Institute (1 RO1 CA157823) 1A1.
Conflict of interest
The authors declare no conflict of interest and have no disclosures to note.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sonnenburg, D.W., Brames, M.J., Case-Eads, S. et al. Utilization of sperm banking and barriers to its use in testicular cancer patients. Support Care Cancer 23, 2763–2768 (2015). https://doi.org/10.1007/s00520-015-2641-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2641-9