Abstract
Purpose
To document the risk of skeletal complications in patients with bone metastases from breast cancer (BC), lung cancer (LC), or prostate cancer (PC) in routine clinical practice.
Methods
We used data from two large US health systems to identify patients aged ≥18 years with primary BC, LC, or PC and newly diagnosed bone metastases between January 1, 1995 and December 31, 2009. Beginning with the date of diagnosis of bone metastasis, we estimated the cumulative incidence of skeletal-related events (SREs) (spinal cord compression, pathologic fracture, radiation to bone, bone surgery), based on review of medical records, accounting for death as a competing risk.
Results
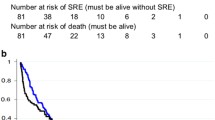
We identified a total of 621 BC, 477 LC, and 721 PC patients with newly diagnosed bone metastases. SREs were present at diagnosis of bone metastasis in 22.4, 22.4, and 10.0 % of BC, LC, and PC patients, respectively. Relatively few LC or PC patients received intravenous bisphosphonates (14.8 and 20.2 %, respectively); use was higher in patients with BC, however (55.8 %). In BC, cumulative incidence of SREs during follow-up was 38.7 % at 6 months, 45.4 % at 12 months, and 54.2 % at 24 months; in LC, it was 41.0, 45.4, and 47.7 %; and in PC, it was 21.5, 30.4, and 41.9 %. More than one half of patients with bone metastases had evidence of SREs (BC: 62.6 %; LC: 58.7 %; PC: 51.7 %), either at diagnosis of bone metastases or subsequently.
Conclusions
SREs are a frequent complication in patients with solid tumors and bone metastases, and are much more common than previously recognized in women with BC.



Similar content being viewed by others
Notes
Primary bone cancer was included in the initial scan of administrative data stores, as the authors have found in prior work that metastatic disease to bone is sometimes miscoded as primary bone cancer.
References
Mundy GR (2002) Metastasis to bone: causes, consequences and therapeutic opportunities. Nat Rev Cancer 2:284–293
Coleman RE (2001) Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev 27:165–176
Weinfurt KP, Castel LD, Li Y, Timbie JW, Glendenning GA, Schulman KA (2004) Health-related quality of life among patients with breast cancer receiving zoledronic acid or pamidronate disodium for metastatic bone lesions. Med Care 42:164–175
Oefelein MG, Ricchiuti V, Conrad W, Resnick MI (2002) Skeletal fractures negatively correlate with overall survival in men with prostate cancer. J Urol 168:1005–1007
Lage MJ, Barber BL, Harrison DJ, Jun S (2008) The cost of treating skeletal-related events in patients with prostate cancer. Am J Managed Care 14:317–322
Delea T, Langer C, McKiernan J, Liss M, Edelsberg J, Brandman J, Sung J, Raut M, Oster G (2004) The cost of treatment of skeletal-related events in patients with bone metastases from lung cancer. Oncology 67:390–396
Rothwell PM (2005) External validity of randomised controlled trials: “to whom do the results of this trial apply?”. Lancet 365:82–93
Hatoum HT, Lin S, Smith MR, Barghout V, Lipton A (2008) Zoledronic acid and skeletal complications in patients with solid tumors and bone metastases. Cancer 113:1438–1445
Nørgaard M, Jensen AØ, Jacobsen JB, Cetin K, Fryzek JP, Sørenson HT (2010) Skeletal related events, bone metastasis and survival of prostate cancer: a population based cohort study in Denmark (1999 to 2007). J Urol 184:162–167
Jensen AØ, Jacobsen JB, Nørgaard M, Yong M, Fryzek JP, Sørenson HT (2011) Incidence of bone metastases and skeletal-related events in breast cancer patients: a population-based cohort study in Denmark. BMC Cancer 11:29
Jensen AØ, Nørgaard M, Yong M, Fryzek JP, Sørensen HT (2009) Validity of the recorded International Classification of Diseases, 10th edition diagnoses codes of bone metastases and skeletal-related events in breast and prostate cancer patients in the Danish National Registry of Patients. Clin Epidemiol 1:101–108
Sun J, Ahn JS, Lee S, Kim JA, Lee J, Park YH, Park HC, Ahn MJ, Ahn YC, Park K (2011) Predictors of skeletal-related events in non-small cell lung cancer patients with bone metastases. Lung Cancer 71:89–93
Yokomizo A, Koga H, Shinohara N, Miyahara T, Machida N, Tsukino H, Uozumi J, Nishiyama K, Satoh F, Sakai H, Naito S (2010) Skeletal-related events in urological cancer patients with bone metastasis: a multicenter study in Japan. Int J Urol 17:332–336
Plunkett TA, Smith P, Rubens RD (2000) Risk of complications from bone metastases in breast cancer: implications for management. Eur J Cancer 36:476–482
Domchek SM, Younger J, Finkelstein DM, Seiden MV (2000) Predictors of skeletal complications in patients with metastatic breast carcinoma. Cancer 89:363–368
Prentice RL, Kalbfleisch JD (1978) The analysis of failure times in the presence of competing risks. Biometrics 34:541–554
Gaynor JJ, Feuer EJ, Tan CC, Wu DH, Little CR, Straus DJ, Clarkson BD, Brennan MF (1993) On the use of cause-specific failure and conditional failure probabilities: examples from clinical oncology data. J Am Statist Assoc 88:400–409
Pepe MS, Mori M (1993) Kaplan–Meier, marginal or conditional probability curves in summarizing competing risks failure time data. Stat Med 12:737–751
Satagopan JM, Ben-Porat L, Berwick M, Robson M, Kutler D, Auerbach AD (2004) A note on competing risks in survival data analysis. Br J Cancer 91:1229–1235
Gooley TA, Leisenring W, Crowley J, Storer BE (1999) Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med 18:695–706
Saad F, Gleason DM, Murray R, Tchekmedyian S, Venner P, Lacombe L, Chin JL, Vinholes JJ, Goas JA, Chen B, Zoledronic Acid Prostate Cancer Study Group (2002) A randomized, placebo-controlled trial of zoledronic acid in patients with hormone-refractory metastatic prostate carcinoma. J Natl Cancer Inst 94:1458–1468
Fizazi K, Carducci M, Smith M, Damião R, Brown J, Karsh L, Milecki P, Shore N, Rader M, Wang H, Jiang Q, Tadros S, Dansey R, Goessl C (2011) Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet 377:813–822
Rosen LS, Gordon D, Tchekmedyian S, Yanagihara R, Hirsh V, Krzakowski M, Pawlicki M, de Souza P, Zheng M, Urbanowitz G, Reitsma D, Seaman JJ (2003) Zoledronic acid versus placebo in the treatment of skeletal metastases in patients with lung cancer and other solid tumors: a phase III, double-blind, randomized trial—the Zoledronic Acid Lung Cancer and Other Solid Tumors Study Group. J Clin Oncol 21:3150–3157
Stopeck AT, Lipton A, Body JJ, Stegar GG, Tonkin K, de Boer RH, Lichinitser M, Fujiwara Y, Yardley DA, Viniegra M, Fan M, Jiang Q, Dansey R, Jun S, Braun A (2010) Denosumab compared with zoledronic acid for the treatment of bone metastases in patients with advanced breast cancer: a randomized, double-blind study. J Clin Oncol 28:5132–5139
Rosen LS, Gordon DH, Dugan W Jr, Major P, Eisenberg PD, Provencher L, Kaminski M, Simeone J, Seaman J, Chen BL, Coleman RE (2004) Zoledronic acid is superior to pamidronate for the treatment of bone metastases in breast carcinoma patients with at least one osteolytic lesion. Cancer 100:36–43
Acknowledgment
Dr. Oster, Dr. Edelsberg, and Ms. Lopez are employed by Policy Analysis Inc., Brookline, MA, which received study funding from Amgen Inc., Thousand Oaks, CA. Dr. Lamerato and Mr. Wolff are employed by Henry Ford Health System, Detroit, MI, which received study funding from Amgen Inc. Dr. Glass and Dr. Richert-Boe are employed by Kaiser Permanente Northwest Region, Portland, OR, which received study funding from Amgen Inc.; Ms. Dodge was employed by Kaiser Permanente Northwest Region at the time the study was conducted. Dr. Chung, Dr. Balakumaran, and Ms. Richhariya are employed by Amgen Inc., and may own stock or stock options in the company.
PAI has full control of all primary data and would agree to allow Supportive Care in Cancer to review the data, if requested.
Conflict of Interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oster, G., Lamerato, L., Glass, A.G. et al. Natural history of skeletal-related events in patients with breast, lung, or prostate cancer and metastases to bone: a 15-year study in two large US health systems. Support Care Cancer 21, 3279–3286 (2013). https://doi.org/10.1007/s00520-013-1887-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1887-3