Summary
Background and aims
Single-nucleotide-polymorphisms in PNPLA3-rs738409 and the TM6SF2-rs58542926, associated with metabolic-dysfunction-associated fatty liver disease (MAFLD), have been discussed as potentially protective for cardiovascular diseases. Therefore, we aimed to study the associations of PNPLA3/TM6SF2 variants with MAFLD and cardiovascular risk in a population-based sample of asymptomatic patients.
Methods
The study cohort comprised 1742 patients of European decent aged 45–80 years from a registry study undergoing screening colonoscopy for colorectal cancer between 2010 and 2014. SCORE2 and Framingham risk score calculated to assess cardiovascular risk. Data on survival were obtained from the national death registry
Results
Half of included patients were male (52%, 59 ± 10 years), 819 (47%) carried PNPLA3‑G and 278 (16%) TM6SF2-T-alleles. MAFLD (PNPLA3‑G-allele: 46% vs. 41%, p = 0.041; TM6SF2‑T-allele: 54% vs. 42%, p < 0.001) was more frequent in patients harbouring risk alleles with both showing independent associations with MAFLD on multivariable binary logistic regression analysis. While median Framingham risk score was lower in PNPLA3‑G-allele carriers (10 vs. 8, p = 0.011), SCORE2 and established cardiovascular diseases were similar across carriers vs. non-carriers of the respective risk-alleles. During a median follow-up of 9.1 years, neither PNPLA3‑G-allele nor TM6SF2‑T-allele was associated with overall nor with cardiovascular mortality.
Conclusion
Carriage of PNPLA3/TM6SF2 risk alleles could not be identified as significant factor for all-cause or cardiovascular mortality in asymptomatic middle-aged individuals undergoing screening colonoscopy.

Similar content being viewed by others
Abbreviations
- 95%CI:
-
95% confidence interval
- BMI:
-
body mass index
- CVD:
-
cardiovascular disease
- GWAS:
-
genome-wide association studies
- HDL‑C:
-
high-density lipoprotein cholesterol
- HOMA-IR:
-
Homeostatic Model Assessment for Insulin Resistance
- IQR:
-
interquartile range
- LDL:
-
low-density lipoprotein
- MAFLD:
-
metabolic (dysfunction) associated fatty liver disease
- NAFLD:
-
non-alcoholic fatty liver disease
- PNPLA3:
-
patatin-like phospholipase domain-containing protein 3
- SD:
-
standard deviation
- SNP:
-
single nucleotide polymorphisms
- TM6SF2:
-
transmembrane 6 superfamily 2
References
Jonas W, Schürmann A. Genetic and epigenetic factors determining NAFLD risk. Mol Metab. 2021;50:101111.
Speliotes EK, et al. Genome-wide association analysis identifies variants associated with nonalcoholic fatty liver disease that have distinct effects on metabolic traits. PLoS Genet. 2011;7(3):e1001324.
Balcar L, et al. PNPLA3 is the dominant SNP linked to liver disease severity at time of first referral to a tertiary center. Dig Liver Dis. 2022;54(1):84–90.
Unalp-Arida A, Ruhl CE. Patatin-like phospholipase domain-containing protein 3 I148M and liver fat and fibrosis scores predict liver disease mortality in the U.S. population. Hepatology. 2020;71(3):820–34.
Abul-Husn NS, et al. A protein-truncating HSD17B13 variant and protection from chronic liver disease. N Engl J Med. 2018;378(12):1096–106.
Liu YL, et al. TM6SF2 rs58542926 influences hepatic fibrosis progression in patients with non-alcoholic fatty liver disease. Nat Commun. 2014;5:4309.
Mancina RM, et al. The MBOAT7-TMC4 variant rs641738 increases risk of nonalcoholic fatty liver disease in individuals of European descent. Gastroenterology. 2016;150(5):1219–1230e6.
Strnad P, et al. Heterozygous carriage of the alpha1-antitrypsin Pi*Z variant increases the risk to develop liver cirrhosis. Gut. 2019;68(6):1099–107.
Holmen OL, et al. Systematic evaluation of coding variation identifies a candidate causal variant in TM6SF2 influencing total cholesterol and myocardial infarction risk. Nat Genet. 2014;46(4):345–51.
Kahali B, et al. TM6SF2: catch-22 in the fight against nonalcoholic fatty liver disease and cardiovascular disease? Gastroenterology. 2015;148(4):679–84.
Dongiovanni P, et al. Transmembrane 6 superfamily member 2 gene variant disentangles nonalcoholic steatohepatitis from cardiovascular disease. Hepatology. 2015;61(2):506–14.
Liu DJ, et al. Exome-wide association study of plasma lipids in 〉300,000 individuals. Nat Genet. 2017;49(12):1758–66.
Simons N, et al. PNPLA3, TM6SF2, and MBOAT7 genotypes and coronary artery disease. Gastroenterology. 2017;152(4):912–3.
Wernly S, et al. A sex-specific propensity-adjusted analysis of colonic adenoma detection rates in a screening cohort. Sci Rep. 2021;11(1):17785.
Semmler G, et al. Nut consumption and the prevalence and severity of non-alcoholic fatty liver disease. PLoS ONE. 2020;15(12):e244514.
Eslam M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020; https://doi.org/10.1016/j.jhep.2020.03.039.
Wilson PW, et al. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–47.
group, S.w., E.C.r. collaboration. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021;42(25):2439–54.
Kedenko L, et al. Genetic polymorphisms at SIRT1 and FOXO1 are associated with carotid atherosclerosis in the SAPHIR cohort. BMC Med Genet. 2014;15:112.
Rodriguez S, Gaunt TR, Day IN. Hardy-Weinberg equilibrium testing of biological ascertainment for Mendelian randomization studies. Am J Epidemiol. 2009;169(4):505–14.
Krawczyk M, Liebe R, Lammert F. Toward genetic prediction of nonalcoholic fatty liver disease trajectories: PNPLA3 and beyond. Gastroenterology. 2020;158(7):1865–1880.e1.
Rüschenbaum S, et al. Patatin-like phospholipase domain containing 3 variants differentially impact metabolic traits in individuals at high risk for cardiovascular events. Hepatol Commun. 2018;2(7):798–806.
Wijarnpreecha K, et al. PNPLA3 gene polymorphism and overall and cardiovascular mortality in the United States. J Gastroenterol Hepatol. 2020;35(10):1789–94.
BasuRay S, et al. Accumulation of PNPLA3 on lipid droplets is the basis of associated hepatic steatosis. Proc Natl Acad Sci USA. 2019;116(19):9521–6.
Scorletti E, Carr RM. A new perspective on NAFLD: focusing on lipid droplets. J Hepatol. 2022;76(4):934–45.
Luo F, Oldoni F, Das A. TM6SF2: a novel genetic player in nonalcoholic fatty liver and cardiovascular disease. Hepatol Commun. 2022;6(3):448–60.
Pirola CJ, Sookoian S. The dual and opposite role of the TM6SF2-rs58542926 variant in protecting against cardiovascular disease and conferring risk for nonalcoholic fatty liver: A meta-analysis. Hepatology. 2015;62(6):1742–56.
Stojkovic IA, et al. The PNPLA3 Ile148Met interacts with overweight and dietary intakes on fasting triglyceride levels. Genes Nutr. 2014;9(2):388–388.
Krarup NT, et al. The PNPLA3 rs738409 G‑allele associates with reduced fasting serum triglyceride and serum cholesterol in danes with impaired glucose regulation. PLoS ONE. 2012;7(7):e40376.
Krawczyk M, et al. The common adiponutrin variant p.I148M does not confer gallstone risk but affects fasting glucose and triglyceride levels. J Physiol Pharmacol. 2011;62(3):369–75.
Kantartzis K, et al. Dissociation between fatty liver and insulin resistance in humans carrying a variant of the patatin-like phospholipase 3 gene. Diabetes. 2009;58(11):2616–23.
Valenti L, et al. Homozygosity for the patatin-like phospholipase-3/adiponutrin I148M polymorphism influences liver fibrosis in patients with nonalcoholic fatty liver disease. Hepatology. 2010;51(4):1209–17.
Author information
Authors and Affiliations
Contributions
Study concept and design (G.S., L.B., C.D.), acquisition of data (all authors), analysis and interpretation of data (G.S., L.B., C.D.), drafting of the manuscript (G.S., L.B., C.D.), critical revision of the manuscript for important intellectual content (all authors).
Corresponding author
Ethics declarations
Conflict of interest
G. Semmler, L. Balcar, S. Wernly, L. Datz, M. Semmler, L. Rosenstatter, F. Stickel, E. Aigner, B. Wernly and C. Datz declare that they have no competing interests.
Ethical standards
All patients provided written informed consent, and the study was approved by the local ethics committee (approval no. 415-E/1262/2-2010).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Authors Georg Semmler and Lorenz Balcar share co-first authorship.
Data sharing Statement:
Data are available from the corresponding author upon reasonable request.
Supplementary Information
508_2023_2196_MOESM1_ESM.docx
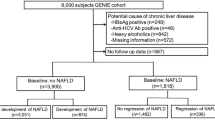
Supplementary data including Supplementary methods for the definition of the metabolic syndrome, and supplementary results including data on reasons for death, comparison of patient characteristics between PNPLA3 C/C vs. G/C vs. G/G, the patient flow-chart, and Kaplan-Meier curves cardiovascular mortality
Rights and permissions
About this article
Cite this article
Semmler, G., Balcar, L., Wernly, S. et al. No association of NAFLD-related polymorphisms in PNPLA3 and TM6SF2 with all-cause and cardiovascular mortality in an Austrian population study. Wien Klin Wochenschr (2023). https://doi.org/10.1007/s00508-023-02196-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00508-023-02196-2