Summary
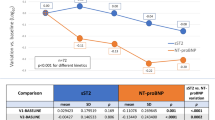
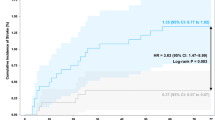
BACKGROUND: Angiotensin-converting enzyme (ACE) inhibitors after acute myocardial infarction (MI) prevent heart failure and recurrent ischemic events. Our aim was to evaluate the effect of ramipril on N-terminal pro-brain natriuretic peptide (NT-proBNP) and on markers of hemostasis, including plasminogen-activator-inhibitor-1 (PAI-1), von Willebrand factor (vWF), factor VIII (FVIII) and fibrinogen, in patients after acute MI, with emphasis on those over 55 years of age. METHODS: In this prospective, single-center, observational study 38 patients were treated with ramipril after the first Q-wave MI. Markers of hemostasis and NT-proBNP were estimated before and two weeks after ramipril treatment. RESULTS: Significant differences were observed in PAI-1 and NT-proBNP levels in patients over 55 years. In this age group the mean PAI-1 level decreased significantly after ramipril therapy (3.6 ± 1.25 U/ml vs. 2.65 ± 1.4 U/ml, P = 0.011) and was significantly lower than in younger (<55 years) patients (2.65 ± 1.4 U/ml vs. 4.39 ± 1.7 U/ml, P = 0.002). In addition, in the older patients the mean baseline NT-proBNP level was significantly higher than in the younger age group (258.35 ± 347.6 pmol/l vs. 17.1 ± 22 pmol/l, P = 0.028) and was also higher after ramipril therapy (240.5 ± 254.3 pmol/l vs. 67.3 ± 75.2 pmol/l, P = 0.034). In the younger patients, mean NT-proBNP after short-term ramipril therapy increased significantly in comparison with baseline (67.3 ± 75.2 pmol/l vs. 17.15 ± 22.0 pmol/l, P = 0.046). CONCLUSION: In acute Q-wave MI, increased PAI-1 levels, but not increased NT-proBNP, respond rapidly to early ACE inhibition by ramipril in patients over 55 years of age but not in younger patients.
Similar content being viewed by others
References
Vaughan DE, Rouleau J-L, Ridker PM, Arnold MO, Menapace FJ, Pfeffer MA; on behalf of the HEART Study Investigators (1997) Effects of ramipril on plasma fibrinolytic balance in patients with acute anterior myocardial infarction. Circulation 96: 442–7
Lopez-Sendon J, Swedberg K, McMurray J, Tamargo J, Maggioni AP, Dargie H, et al (2004) Expert consensus document on angiotensin-converting enzyme inhibitors in cardiovascular disease. The task force on ACE-inhibitors of the European Society of Cardiology. Eur Heart J 25: 1454–70
Boman KO, Jansson J-H, Nyhlen KA, Nilsson TK (2002) Improved fibrinolysis after one year of treatment with enalapril in men and women with uncomplicated myocardial infarction. Throm Haemost 87: 311–6
Shah AD, Arora RR (2005) Tissue angiotensin-converting enzyme inhibitors: are they more effective than serum angiotensin-converting enzyme inhibitors? Clin Cardiol 28: 551–5
Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G (2000) Effect of angiotensin-converting enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcome Prevention Evaluation Study Investigators. N Engl J Med 342: 145–53
Fox KM; EURopean trial on reduction of cardiac events with Perindopril in stable coronary Artery disease Investigators (2003) Efficacy of perindopril in reduction of cardiovascular events among patients with stable coronary artery disease: randomized, double-blind, placebo-controlled, multicenter trial (the EUROPA Study). Lancet 362: 782–8
Omland T, Persson A, Ng L, O'Brien R, Karlsson T, Herlitz J, et al (2002) N-terminal pro-B-type natriuretic peptide and long-term mortality in acute coronary syndromes. Circulation 106: 2913–8
De Lemos JA, Morrow DA, Bentley JH, Omland T, Sabatine MS, McCabe C, et al (2001) The prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. N Engl J Med 345: 1014–21
Nordt TK, Peter K, Ruef J, Kübler W, Bode C (1999) Plasminogen activator inhibitor type-1 (PAI-1) and its role in cardiovascular disease. Thromb Haemost 82[Suppl 1]: 14–8
Vaughan DE (2005) PAI-1 and atherothrombosis. J Thromb Haemost 3: 1879–83
Agirbasli M (2005) Pivotal role of plasminogen-activator inhibitor 1 in vascular disease. Int J Clin Pract 59: 102–106
Trost S, Pratley R, Sobel B (2006) Impaired fibrinolysis and risk for cardiovascular disease in the metabolic syndrome and type 2 diabetes. Curr Diab Rep 6: 47–54
Smith A, Patterson C, Yarnell J, Rumley A, Ben-Shlomo Y, Lowe G (2005) Which hemostatic markers add to the predictive value of conventional risk factors for coronary heart disease and ischemic stroke? The Caerphilly Study. Circulation 112: 3080–7
Sinkovic A, Pogacar V (2004) Risk stratification in patients with unstable angina and/or non-ST-elevation myocardial infarction by Troponin T and plasminogen-activator-inhibitor-1 (PAI-1). Thromb Res 114: 251–7
von Eyben FE, Mouritsen E, Holm J, Montvilas P, Dimcevski G, Suciu G, et al (2005) Plasminogen activator inhibitor 1 activity and other coronary risk factors. Clin Appl Thromb Hemost 11: 55–61
Cooney MT, Dudina AL, O'Callaghan P, Graham IM (2007) von Willebrand factor in CHD and stroke: relationships and therapeutic implications. Curr Treat Options Cardiovasc Med 9: 180–90
Matsukawa M, Kaikita K, Soejima K, Fuchigami S, Nakamura Y, Honda T, et al (2007) Serial changes in von Willebrand factor-cleaving protease (ADAMTS13) and prognosis after acute myocardial infarction. Am J Cardiol 100: 758–63
Pilote L, Abrahamowicz M, Rodrigues E, Eisenberg MJ, Rahme E (2004) Mortality rates in elderly patients who take different angiotensin-converting enzyme inhibitors after acute myocardial infarction: a class effect? Ann Intern Med 141: 102–12
Tofler GH, Massaro J, Levy D, Mittleman M, Sutherland P, Lipinska I, et al (2005) Relation of the prothrombotic state to increasing age (from the Framingham Offspring Study). Am J Cardiol 96: 1280–3
Van de Werf F, Ardissino D, Betriu A, Cokkinos DV, Falk E, Fox KA, et al (2003) Management of acute myocardial infarction in patients presenting with ST-segment elevation. The task force on the management of acute myocardial infarction of the European Society of cardiology. Eur Heart J 24: 28–66
Hamsten A, Wiman B, de Faire U, Blomback M (1985) Increased plasma levels of a rapid inhibitor of tissue plasminogen activator in young survivors of myocardial infarction. N Engl J Med 313: 1557–63
Dagenais GR, Pogue J, Fox K, Simoons ML, Yusuf S (2006) Angiotensin-converting-enzyme inhibitors in stable vascular disease without left ventricular systolic dysfunction or heart failure: a combined analysis of three trials. Lancet 368: 581–8
Flather MD, Yusuf S, Køber L, Pfeffer M, Hall A, Murray G, et al (2000) Long-term ACE-inhibitor therapy in patients with heart failure or left-ventricular dysfunction: a systematic overview of data from individual patients. ACE-Inhibitor Myocardial Infarction Collaborative Group. Lancet 355: 1575–81
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sinkovič, A. Age-related short-term effect of ramipril on N-terminal pro-brain natriuretic peptide and markers of hemostasis in patients after acute myocardial infarction. Wien Klin Wochenschr 122 (Suppl 2), 74–78 (2010). https://doi.org/10.1007/s00508-010-1342-0
Issue Date:
DOI: https://doi.org/10.1007/s00508-010-1342-0