Abstract
Background
Nephrotic syndrome relapse within 6 months is a known risk factor for steroid-dependent nephrotic syndrome/frequently relapsing nephrotic syndrome (SDNS/FRNS), but the risk of early development of SDNS/FRNS and initiation of immunosuppression therapy remains unknown.
Methods
Patients with childhood-onset idiopathic nephrotic syndrome who had the first relapse within 6 months were enrolled. We analyzed the relationship between the time of the first relapse or the time of initial remission and incidence of SDNS/FRNS or initiation of immunosuppression therapy.
Results
Forty-five patients were enrolled. Twenty out of 23 patients (87%) with the first relapse within 30 days after discontinuing initial steroid therapy experienced a second relapse within 30 days after discontinuing steroid therapy. Additionally, most patients in this group (96%) experienced a second relapse within 6 months after the onset and were diagnosed as SDNS/FRNS at this time. In this group, the incidence of SDNS/FRNS development within 6 months was 96%. In contrast, the incidence of SDNS/FRNS development within 6 months was 18% in patients with the first relapse more than 30 days after steroid discontinuation. The incidence of initiation of immunosuppressive agents within 6 months was 83% in the former group and 14% in the latter group.
Conclusions
Most patients with the first relapse within 30 days after discontinuing steroid therapy developed SDNS/FRNS and were administered immunosuppressive agents within 6 months. Thus, it might be reasonable to start immunosuppression therapy in this group without waiting for the second relapse.
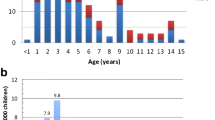
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information




Similar content being viewed by others
Data availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
Noone DG, Iijima K, Parekh R (2018) Idiopathic nephrotic syndrome in children. Lancet 392:61–74. https://doi.org/10.1016/S0140-6736(18)30536-1
Carter SA, Mistry S, Fitzpatrick J, Banh T, Hebert D, Langlois V, Pearl RJ, Chanchlani R, Licht CPB, Radhakrishnan S, Brooke J, Reddon M, Levin L, Aitken-Menezes K, Noone D, Parekh RS (2019) Prediction of short- and long-term outcomes in childhood nephrotic syndrome. Kidney Int Rep 5:426–434. https://doi.org/10.1016/j.ekir.2019.12.015
Sato M, Ishikura K, Ando T, Kikunaga K, Terano C, Hamada R, Ishimori S, Hamasaki Y, Araki Y, Gotoh Y, Nakanishi K, Nakazato H, Matsuyama T, Iijima K, Yoshikawa N, Ito S, Honda M, Japanese Pediatric Survey Holding Information of Nephrotic Syndrome study of the Japanese Study Group of Renal Disease in Children (2021) Prognosis and acute complications at the first onset of idiopathic nephrotic syndrome in children: a nationwide survey in Japan (JP-SHINE study). Nephrol Dial Transplant 36:475–481. https://doi.org/10.1093/ndt/gfz185
Bajeer I, Khatri S, Hashmi S, Lanewala A (2022) Factors predicting short term outcome in children with idiopathic nephrotic syndrome: a prospective cohort study. Cureus 14:e21538. https://doi.org/10.7759/cureus.21538
Gebrehiwot M, Kassa M, Gebrehiwot H, Sibhat M (2020) Time to relapse and its predictors among children with nephrotic syndrome in comprehensive specialized hospitals, Tigray, Ethiopia, 2019. Int J Pediatr 2020:8818953. https://doi.org/10.1155/2020/8818953
Sureshkumar P, Hodson EM, Willis NS, Barzi F, Craig JC (2014) Predictors of remission and relapse in idiopathic nephrotic syndrome: a prospective cohort study. Pediatr Nephrol 29:1039–1046. https://doi.org/10.1007/s00467-013-2736-9
Mishra OP, Abhinay A, Mishra RN, Prasad R, Pohl M (2013) Can we predict relapses in children with idiopathic steroid-sensitive nephrotic syndrome? J Trop Pediatr 59:343–349. https://doi.org/10.1093/tropej/fmt029
Dakshayani B, Lakshmanna M, Premalatha R (2018) Predictors of frequent relapsing and steroid-dependent nephrotic syndrome in children. Turk Pediatri Ars 53:24–30. https://doi.org/10.5152/TurkPediatriArs.2018.5749
Nakanishi K, Iijima K, Ishikura K, Hataya H, Nakazato H, Sasaki S, Honda M, Yoshikawa N, Japanese Study Group of Renal Disease in Children (2013) Two-year outcome of the ISKDC regimen and frequent-relapsing risk in children with idiopathic nephrotic syndrome. Clin J Am Soc Nephrol 8:756–762. https://doi.org/10.2215/CJN.09010912
Letavernier B, Letavernier E, Leroy S, Baudet-Bonneville V, Bensman A, Ulinski T (2008) Prediction of high-degree steroid dependency in pediatric idiopathic nephrotic syndrome. Pediatr Nephrol 23:2221–2226. https://doi.org/10.1007/s00467-008-0914-y
Noer MS (2005) Predictors of relapse in steroid-sensitive nephrotic syndrome. Southeast Asian J Trop Med Public Health 36:1313–1320
Yoshikawa N, Nakanishi K, Sako M, Oba MS, Mori R, Ota E, Ishikura K, Hataya H, Honda M, Ito S, Shima Y, Kaito H, Nozu K, Nakamura H, Igarashi T, Ohashi Y, Iijima K (2015) A multicenter randomized trial indicates initial prednisolone treatment for childhood nephrotic syndrome for two months is not inferior to six-month treatment. Kidney Int 87:225–232. https://doi.org/10.1038/ki.2014.260
The Japanese Society of Pediatric Nephrology (2020) Clinical guideline for pediatric idiopathic nephrotic syndrome 2020. Shindan To Chiryo-sha, Tokyo, pp 5–6, 26 (Japanese only)
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK, Gidding SS, Goodwin C, Leu MG, Powers ME, Rea C, Samuels J, Simasek M, Thaker VV, Urbina EM (2017) Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140:e20171904. https://doi.org/10.1542/peds.2017-1904
Weinreb RN, Grajewski A, Papadopoulos M, Grigg J, Freedman S (2013) Childhood glaucoma: the 9th Consensus Report of the World Glaucoma Association. Kugler Publications, Amsterdam
Tarshish P, Tobin JN, Bernstein J, Edelmann CM Jr (1997) Prognostic significance of the early course of minimal change nephrotic syndrome: report of the International Study of Kidney Disease in Children. J Am Soc Nephrol 8:769–776. https://doi.org/10.1681/ASN.V85769
Fujinaga S, Hirano D, Nishizaki N (2011) Early identification of steroid dependency in Japanese children with steroid-sensitive nephrotic syndrome undergoing short-term initial steroid therapy. Pediatr Nephrol 26:485–486. https://doi.org/10.1007/s00467-010-1642-7
Vivarelli M, Moscaritolo E, Tsalkidis A, Massella L, Emma F (2010) Time for initial response to steroids is a major prognostic factor in idiopathic nephrotic syndrome. J Pediatr 156:965–971. https://doi.org/10.1016/j.jpeds.2009.12.020
Yap HK, Han EJ, Heng CK, Gong WK (2001) Risk factors for steroid dependency in children with idiopathic nephrotic syndrome. Pediatr Nephrol 16:1049–1052. https://doi.org/10.1007/s004670100024
Abdel-Hafez MA, Abou-El-Hana NM, Erfan AA, El-Gamasy M, Abdel-Nabi H (2017) Predictive risk factors of steroid dependent nephrotic syndrome in children. J Nephropathol 6:180–186. https://doi.org/10.15171/jnp.2017.31
Watts AJB, Keller KH, Lerner G, Rosales I, Collins AB, Sekulic M, Waikar SS, Chandraker A, Riella LV, Alexander MP, Troost JP, Chen J, Fermin D, Yee JL, Sampson MG, Beck LH Jr, Henderson JM, Greka A, Rennke HG, Weins A (2022) Discovery of autoantibodies targeting nephrin in minimal change disease supports a novel autoimmune etiology. J Am Soc Nephrol 33:238–252. https://doi.org/10.1681/ASN.2021060794
Author information
Authors and Affiliations
Contributions
All authors were physicians who treated the patients in this study. YI conducted the study, collected the clinical and laboratory data, and wrote the manuscript. KN, KO, TK, MA, MS, and MO reviewed and edited the manuscript. KK supervised the work and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Ethics Committee of the National Center for Child Health and Development (approval no. 2022–210). It was conducted according to the principles of the Declaration of Helsinki and the ethics guidelines of the Japanese Ministry of Health, Labor and Welfare.
Consent to participate
Due to the retrospective nature of this study, informed consent for participation was waived.
Consent for publication
Due to the retrospective nature of this study, informed consent to publish was waived.
Competing interests
Koichi Kamei has obtained research funding from the Public Foundation of Vaccination Research Center, the Terumo Foundation for Life Sciences and Arts, and the Taiju Life Social Welfare Foundation; donations from Chugai Pharmaceutical Co. Ltd., Astellas Pharma Inc., Ono Pharmaceutical Co. Ltd., Teijin Pharma Ltd., Shionogi Co. Ltd., and Otsuka Pharmaceutical Co. Ltd.; and lecture fees from Tanabe Mitsubishi Pharma, Baxter Ltd., and Zenyaku Kogyo Co. Ltd. All other authors have no potential conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Inoki, Y., Nishi, K., Osaka, K. et al. Association between the time of initial relapse and subsequent relapses in patients with childhood-onset idiopathic nephrotic syndrome. Pediatr Nephrol (2024). https://doi.org/10.1007/s00467-024-06286-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00467-024-06286-9