Abstract
Background
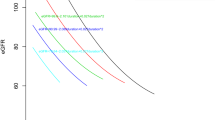
We conducted exploratory analyses to identify distinct trajectories of estimated glomerular filtration rate (eGFR) and their relationship with hyperfiltration, subsequent rapid eGFR decline, and albuminuria in participants with youth-onset type 2 diabetes enrolled in the Treatment Options for type 2 Diabetes in Adolescents and Youth (TODAY) study.
Methods
Annual serum creatinine, cystatin C, urine albumin, and creatinine measurements were obtained from 377 participants followed for ≥ 10 years. Albuminuria and eGFR were calculated. Hyperfiltration peak is the greatest eGFR inflection point during follow-up. Latent class modeling was applied to identify distinct eGFR trajectories.
Results
At baseline, participants’ mean age was 14 years, type 2 diabetes duration was 6 months, mean HbA1c was 6%, and mean eGFR was 120 ml/min/1.73 m2. Five eGFR trajectories associated with different rates of albuminuria were identified, including a “progressive increasing eGFR” group (10%), three “stable eGFR” groups with varying starting mean eGFR, and an “eGFR steady decline” group (1%). Participants who exhibited the greatest peak eGFR also had the highest levels of elevated albuminuria at year 10. This group membership was characterized by a greater proportion of female and Hispanic participants.
Conclusions
Distinct eGFR trajectories that associate with albuminuria risk were identified, with the eGFR trajectory characterized by increasing eGFR over time associating with the highest level of albuminuria. These descriptive data support the current recommendations to estimate GFR annually in young persons with type 2 diabetes and provide insight into eGFR-related factors which may contribute to predictive risk strategies for kidney disease therapies in youth with type 2 diabetes.
Trial registration
ClinicalTrials.gov Identifier: NCT00081328, date registered 2002.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information


Similar content being viewed by others
Data availability
Data collected for the TODAY/TODAY2 studies are available to the public through the NIDDK Repository: https://repository.niddk.nih.gov/studies/today/.
References
Saran R, Robinson B, Abbott KC, Bragg-Gresham J, Chen X, Gipson D, Gu H, Hirth RA, Hutton D, Jin Y, Kapke A, Kurtz V, Li Y, McCullough K, Modi Z, Morgenstern H, Mukhopadhyay P, Pearson J, Pisoni R, Repeck K, Schaubel DE, Shamraj R, Steffick D, Turf M, Woodside KJ, Xiang J, Yin M, Zhang X, Shahinian V (2020) US Renal Data System 2019 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis 75:A6–A7
TODAY Study Group, Bjornstad P, Drews KL, Caprio S, Gubitosi-Klug R, Nathan DM, Tesfaldet B, Tryggestad J, White NH, Zeitler P (2021) Long-term complications in youth-onset type 2 diabetes. N Engl J Med 385:416–426
Bjornstad P, Cherney DZ (2018) Renal hyperfiltration in adolescents with type 2 diabetes: physiology, sex differences, and implications for diabetic kidney disease. Curr Diab Rep 18:22
Stefansson VTN, Nair V, Melsom T, Looker HC, Mariani LH, Fermin D, Eichinger F, Menon R, Subramanian L, Ladd P, Harned R, Harder JL, Hodgin JB, Bjornstad P, Nelson PJ, Eriksen BO, Nelson RG, Kretzler M (2022) Molecular programs associated with glomerular hyperfiltration in early diabetic kidney disease. Kidney Int 102:1345–1358
Oshima M, Shimizu M, Yamanouchi M, Toyama T, Hara A, Furuichi K, Wada T (2021) Trajectories of kidney function in diabetes: a clinicopathological update. Nat Rev Nephrol 17:740–750
TODAY Study Group (2021) Effects of metabolic factors, race-ethnicity, and sex on the development of nephropathy in adolescents and young adults with type 2 diabetes: results from the TODAY Study. Diabetes Care 45:1056–1064
Zeitler P, Epstein L, Grey M, Hirst K, Kaufman F, Tamborlane W, Wilfley D; TODAY Study Group (2007) Treatment options for type 2 diabetes in adolescents and youth: a study of the comparative efficacy of metformin alone or in combination with rosiglitazone or lifestyle intervention in adolescents with type 2 diabetes. Pediatr Diabetes 8:74–87
TODAY Study Group (2013) Rapid rise in hypertension and nephropathy in youth with type 2 diabetes: the TODAY clinical trial. Diabetes Care 36:1735–1741
Pottel H, Delanaye P, Schaeffner E, Dubourg L, Eriksen BO, Melsom T, Lamb EJ, Rule AD, Turner ST, Glassock RJ, De Souza V, Selistre L, Goffin K, Pauwels S, Mariat C, Flamant M, Ebert N (2017) Estimating glomerular filtration rate for the full age spectrum from serum creatinine and cystatin C. Nephrol Dial Transplant 32:497–507
Nagin D (2005) Group-based modeling of development. Harvard University Press, Boston
Nagin DS, Odgers CL (2010) Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol 6:109–138
Twisk J, Hoekstra T (2012) Classifying developmental trajectories over time should be done with great caution: a comparison between methods. J Clin Epidemiol 65:1078–1087
Jones B. Traj: group-based modeling of longitudinal data. http://www.andrew.cmu.edu/user/bjones/index.htm. Accessed April 2022
Brenner BM, Hostetter TH, Olson JL, Rennke HG, Venkatachalam MA (1981) The role of glomerular hyperfiltration in the initiation and progression of diabetic nephropathy. Acta Endocrinol Suppl (Copenh) 242:7–10
Ruggenenti P, Porrini EL, Gaspari F, Motterlini N, Cannata A, Carrara F, Cella C, Ferrari S, Stucchi N, Parvanova A, Iliev I, Dodesini AR, Trevisan R, Bossi A, Zaletel J, Remuzzi G, GFR Study Investigators (2012) Glomerular hyperfiltration and renal disease progression in type 2 diabetes. Diabetes Care 35:2061–2068
Nelson RG, Bennett PH, Beck GJ, Tan M, Knowler WC, Mitch WE, Hirschman GH, Myers BD (1996) Development and progression of renal disease in Pima Indians with non-insulin-dependent diabetes mellitus. Diabetic Renal Disease Study Group. N Engl J Med 335:1636–1642
Park M, Yoon E, Lim YH, Kim H, Choi J, Yoon HJ (2015) Renal hyperfiltration as a novel marker of all-cause mortality. J Am Soc Nephrol 26:1426–1433
Pagtalunan ME, Miller PL, Jumping-Eagle S, Nelson RG, Myers BD, Rennke HG, Coplon NS, Sun L, Meyer TW (1997) Podocyte loss and progressive glomerular injury in type II diabetes. J Clin Invest 99:342–348
Looker HC, Mauer M, Saulnier P-J, Harder JL, Nair V, Boustany-Kari CM, Guarnieri P, Hill J, Esplin CA, Kretzler M, Nelson RG, Najafian B (2019) Changes in albuminuria but not GFR are associated with early changes in kidney structure in type 2 diabetes. J Am Soc Nephrol 30:1049–1059
Denic A, Mathew J, Lerman LO, Lieske JC, Larson JJ, Alexander MP, Poggio E, Glassock RJ, Rule AD (2017) Single-nephron glomerular filtration rate in healthy adults. N Engl J Med 376:2349–2357
Piani F, Melena I, Tommerdahl KL, Nokoff N, Nelson RG, Pavkov ME, van Raalte DH, Cherney DZ, Johnson RJ, Nadeau KJ, Bjornstad P (2021) Sex-related differences in diabetic kidney disease: a review on the mechanisms and potential therapeutic implications. J Diabetes Complicat 35:107841
Lewko B, Stepinski J (2009) Hyperglycemia and mechanical stress: targeting the renal podocyte. J Cell Physiol 221:288–295
Veelken R, Hilgers KF, Hartner A, Haas A, Bohmer KP, Sterzel RB (2000) Nitric oxide synthase isoforms and glomerular hyperfiltration in early diabetic nephropathy. J Am Soc Nephrol 11:71–79
Fioretto P, Zambon A, Rossato M, Busetto L, Vettor R (2016) SGLT2 inhibitors and the diabetic kidney. Diabetes Care 39(Suppl 2):S165–S171
Helal I, Fick-Brosnahan GM, Reed-Gitomer B, Schrier RW (2012) Glomerular hyperfiltration: definitions, mechanisms and clinical implications. Nat Rev Nephrol 8:293–300
Kriz W, Lemley KV (2015) A potential role for mechanical forces in the detachment of podocytes and the progression of CKD. J Am Soc Nephrol 26:258–269
Giandalia A, Giuffrida AE, Gembillo G, Cucinotta D, Squadrito G, Santoro D, Russo GT (2021) Gender differences in diabetic kidney disease: focus on hormonal, genetic and clinical factors. Int J Mol Sci 22:5808
Vikse BE, Irgens LM, Leivestad T, Hallan S, Iversen BM (2008) Low birth weight increases risk for end-stage renal disease. J Am Soc Nephrol 19:151–157
Luyckx VA, Brenner BM (2010) The clinical importance of nephron mass. J Am Soc Nephrol 21:898–910
Amri K, Freund N, Vilar J, Merlet-Bénichou C, Lelièvre-Pégorier M (1999) Adverse effects of hyperglycemia on kidney development in rats: in vivo and in vitro studies. Diabetes 48:2240–2245
Edwards M (2017) The Barker Hypothesis. In: Preedy V, Patel V (eds) Handbook of famine, starvation, and nutrient deprivation. Springer, Cham
Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group (2020) KDIGO 2020 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int 98:S1–S115
Acknowledgements
We thank all the members of the TODAY Study Group not included among the authors. A complete list of individuals can be found at https://www.nejm.org/doi/suppl/10.1056/NEJMoa2100165/suppl_file/nejmoa2100165_appendix.pdf. The TODAY Study Group thanks the following companies for donations in support of the study’s efforts: Becton, Dickinson and Company; Bristol-Myers Squibb; Eli Lilly and Company; GlaxoSmithKline; LifeScan, Inc.; Pfizer; and Sanofi Aventis. We also gratefully acknowledge the participation and guidance of the American Indian partners associated with the clinical center located at the University of Oklahoma Health Sciences Center, including members of the Absentee Shawnee Tribe, Cherokee Nation, Chickasaw Nation, Choctaw Nation of Oklahoma, and Oklahoma City Area Indian Health Service; the opinions expressed in this paper are those of the authors and do not necessarily reflect the views of the respective Tribes and the Indian Health Service.
Funding
This work was completed with funding from NIDDK and the NIH Office of the Director through grants U01-DK61212, U01-DK61230, U01-DK61239, U01-DK61242, and U01-DK61254. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The NIDDK project office was involved in all aspects of the study, including design and conduct; collection, management, analysis, and interpretation of the data; review and approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Consortia
Contributions
L. E., J. L., and P. B. designed the analyses and wrote the manuscript. L. E. and W. H. conducted the statistical analyses and prepared the tables and figures. D. U., M. W. H., K. H., K. K., L. L., S. T., and E. N. E. contributed to interpretation of the data and reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jane Lynch and Petter Bjornstad contributed equally to this work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
El ghormli, L., Wen, H., Uschner, D. et al. Trajectories of eGFR and risk of albuminuria in youth with type 2 diabetes: results from the TODAY cohort study. Pediatr Nephrol 38, 4137–4144 (2023). https://doi.org/10.1007/s00467-023-06044-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-06044-3