Abstract
Background: Clinically relevant surgical outcomes are usually monitored by surgeons only for new and/or high-volume procedures. Prospective outcomes audit studies are rarely done on 100% of procedures performed by a single surgeon, a surgical practice, or an institution. Therefore, we set out to determine the resource utilization and accuracy of a well-validated system at its introduction into a North American university surgical practice.
Methods: The Otago Surgical Audit, which has been validated in a wide spectrum of surgical practices in Australasia, was applied to a university practice in general and laparoscopic surgery. Data were recorded by the surgeon on the day of operation, at discharge, and during any subsequent readmission. Resource utilization was determined by timing the important steps in data acquisition and computer entry. Data accuracy was assessed by an independent chart review of 22% of all records. Case capture was audited by reviewing operating room case logs.
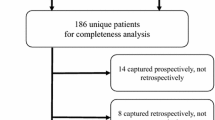
Results: Over 1 year, from October 1, 1996 to September 30, 1997, 338 procedures were performed. Data recording and coding by the surgeon required 2 min per form, or a total of 676 min (11.3 h) annually. Data entry required 2.11 min per form, or a total of 713 min (11.9 h) for the year. Eight percent of cases were returned to the surgeon for additional information. In the medical record audit, no additional mortality or readmissions were discovered, and one minor complication was recorded in the hospital record but not the outcomes audit. One complication and three operations recorded in the audit database were omitted from operating room records. Two minor procedures on the operating room log were omitted from the audit database. Operating time reported by the surgeon averaged 19 min less than recorded in the operative log. Data accuracy and coding accuracy improved significantly between the 1st month (month 4) and the 2nd month audited (month 12), (p < .01).
Conclusions: It is possible to perform a 100% clinical outcome audit with the use of minimal resources. When the surgeon is involved with data acquisition and coding, the accuracy and completeness of the log may outstrip the medical record, but a learning curve of 4–6 months may be required to achieve this goal.
Similar content being viewed by others
Author information
Authors and Affiliations
Additional information
Received: 15 May 1998/Accepted: 12 February 1999
Rights and permissions
About this article
Cite this article
Hunter, J., Lyon, C., Galloway, K. et al. Complete clinical outcomes audit. Surg Endosc 13, 699–704 (1999). https://doi.org/10.1007/s004649901076
Published:
Issue Date:
DOI: https://doi.org/10.1007/s004649901076