Abstract
Introduction
Pre-operative evaluation of patients with gastroesophageal reflux disease (GERD) includes assessment of esophageal motility. High-resolution manometry (HRM) is the gold standard; endoscopic impedance planimetry (IP) with Endoflip 2.0 is increasingly utilized in esophageal disorders of motility. We hypothesized that normal IP motility would correlate with normal HRM motility and tested this in a prospective cohort study.
Methods
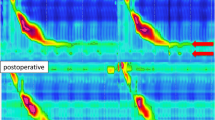
Patients presenting for surgical evaluation of GERD between 9/2020 and 10/2021 were prospectively enrolled under an IRB-approved protocol. Patients with prior esophageal/gastric surgery, known motility disorders, or large paraesophageal hernias were excluded. All underwent HRM and IP, with normal motility defined by Chicago 3.0 classification for HRM and the presence of repetitive antegrade contractions for IP. Logistic regression and t test were used to analyze the data; p value < 0.05 was considered significant.
Results
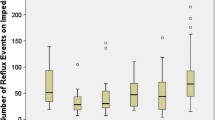
Of 63 patients enrolled, 48 completed both IP and HRM testing. The cohort was 50% male with a median age of 52.5 [42.0, 66.0] years, mostly ASA class 1–2 (75.1%, n = 36) and had an average BMI of 31.4 ± 6.3 kg/m2. Normal motility tracings were in 62.5% of IP and 75% of HRM tests. Using HRM as the gold standard, IP detected normal motility with a sensitivity of 65.8% and a specificity of 50% (positive predictive value 83.3%, negative predictive value 27.8%). Normal IP was not statistically significant in predicting normal HRM (OR 3.182, 95% CI 0.826–12.262, p = 0.0926). Tolerability of IP was significantly better than HRM with lower rates of discomfort (10.9% vs. 93.4%, p < 0.0001) and higher willingness to repeat testing (100% vs. 47.8%, p < 0.0001).
Conclusion
Esophageal motility testing with Endoflip 2.0 is well tolerated by patients. The low specificity (50%), poor negative predictive value (27.8%), and lack of statistically significant concordance between IP and HRM raises concern for the reliability of this test as a stand-alone replacement for HRM in the pre-operative evaluation for GERD.
Graphical abstract


Similar content being viewed by others
References
Schlottmann F, Herbella FA, Allaix ME, Rebecchi F, Patti MG (2017) Surgical treatment of gastroesophageal reflux disease. World J Surg 41(7):1685–1690. https://doi.org/10.1007/s00268-017-3955-1
Rettura F, Bronzini F, Campigotto M et al (2021) Refractory gastroesophageal reflux disease: a management update. Front Med 8:765061. https://doi.org/10.3389/fmed.2021.765061
Rohof WOA, Bredenoord AJ (2017) Chicago classification of esophageal motility disorders: lessons learned. Curr Gastroenterol Rep 19(8):37. https://doi.org/10.1007/s11894-017-0576-7
Yadlapati R, Furuta GT, Menard-Katcher P (2019) New developments in esophageal motility testing. Curr Treat Options Gastroenterol 17(1):76–88. https://doi.org/10.1007/s11938-019-00218-5
Carlson DA, Lin Z, Rogers MC, Lin CY, Kahrilas PJ, Pandolfino JE (2015) Utilizing functional lumen imaging probe topography to evaluate esophageal contractility during volumetric distention: a pilot study. Neurogastroenterol Motil 27(7):981–989. https://doi.org/10.1111/nmo.12572
Smeets FGM, Keszthelyi D, Bouvy ND, Masclee AAM, Conchillo JM (2015) Does measurement of esophagogastric junction distensibility by Endoflip predict therapy-responsiveness to endoluminal fundoplication in patients with gastroesophageal reflux disease? J Neurogastroenterol Motil 21(2):255–264. https://doi.org/10.5056/jnm14111
Carlson DA (2016) Functional lumen imaging probe: the FLIP side of esophageal disease. Curr Opin Gastroenterol 32(4):310–318. https://doi.org/10.1097/MOG.0000000000000272
Chen HM, Li BW, Li LY et al (2019) Functional lumen imaging probe in gastrointestinal motility diseases. J Dig Dis 20(11):572–577. https://doi.org/10.1111/1751-2980.12818
Campagna RAJ, Carlson DA, Hungness ES et al (2020) Intraoperative assessment of esophageal motility using FLIP during myotomy for achalasia. Surg Endosc 34(6):2593–2600. https://doi.org/10.1007/s00464-019-07028-x
Carlson DA, Kou W, Lin Z et al (2019) Normal values of esophageal distensibility and distension-induced contractility measured by functional luminal imaging probe panometry. Clin Gastroenterol Hepatol 17(4):674–681.e1. https://doi.org/10.1016/j.cgh.2018.07.042
Carlson DA, Gyawali CP, Kahrilas PJ et al (2019) Esophageal motility classification can be established at the time of endoscopy: a study evaluating real-time functional luminal imaging probe panometry. Gastrointest Endosc 90(6):915–923.e1. https://doi.org/10.1016/j.gie.2019.06.039
Carlson DA, Kathpalia P, Craft J et al (2018) The relationship between esophageal acid exposure and the esophageal response to volumetric distention. Neurogastroenterol Motil. https://doi.org/10.1111/nmo.13240
Velanovich V, Vallance SR, Gusz JR, Tapia FV, Harkabus MA (1996) Quality of life scale for gastroesophageal reflux disease. J Am Coll Surg 183(3):217–224
Allen CJ, Parameswaran K, Belda J, Anvari M (2000) Reproducibility, validity, and responsiveness of a disease-specific symptom questionnaire for gastroesophageal reflux disease. Dis Esophagus 13(4):265–270. https://doi.org/10.1046/j.1442-2050.2000.00129.x
Kahrilas PJ, Bredenoord AJ, Fox M et al (2015) The Chicago classification of esophageal motility disorders. Neurogastroenterol Motil 27(2):160–174. https://doi.org/10.1111/nmo.12477
Carlson DA, Kou W, Pandolfino JE (2020) The rhythm and rate of distension-induced esophageal contractility: a physiomarker of esophageal function. Neurogastroenterol Motil 32(5):e13794. https://doi.org/10.1111/nmo.13794
Ayazi S, DeMeester SR, Hagen JA et al (2019) Clinical significance of esophageal outflow resistance imposed by a Nissen fundoplication. J Am Coll Surg 229(2):210–216. https://doi.org/10.1016/j.jamcollsurg.2019.03.024
Fanous M, Wei W (2022) The outcomes of performing partial fundoplication based on Endoflip versus manometric findings. Am Surg 88(5):908–914. https://doi.org/10.1177/00031348211054565
Kim MP, Meisenbach LM, Chan EY (2018) Tailored fundoplication with endoluminal functional lumen imaging probe allows for successful minimally invasive hiatal hernia repair. Surg Laparosc Endosc Percutan Tech 28(3):178–182. https://doi.org/10.1097/SLE.0000000000000527
Shah A, Nguyen DT, Meisenbach LM et al (2022) A novel EndoFLIP marker during hiatal hernia repair is associated with short-term postoperative dysphagia. Surg Endosc 36(7):4764–4770. https://doi.org/10.1007/s00464-021-08817-z
Nwokedi U, Nguyen DT, Meisenbach LM et al (2021) Short-term outcome of routine use of EndoFLIP during hiatal hernia repair. Surg Endosc 35(7):3840–3849. https://doi.org/10.1007/s00464-020-07788-x
Turner B, Helm M, Hetzel E, Gould JC (2020) Is that “floppy” fundoplication tight enough? Surg Endosc 34(4):1823–1828. https://doi.org/10.1007/s00464-019-06947-z
Hodges MM, DeSouza ML, Reavis KM, Davila Bradley D, Dunst CM (2022) Abnormal response after multiple rapid swallow provocation is not predictive of post-operative dysphagia following a tailored fundoplication approach. Surg Endosc. https://doi.org/10.1007/s00464-022-09507-0
Kapadia S, Osler T, Lee A, Borrazzo E (2018) The role of preoperative high resolution manometry in predicting dysphagia after laparoscopic Nissen fundoplication. Surg Endosc 32(5):2365–2372. https://doi.org/10.1007/s00464-017-5932-z
Acknowledgements
None.
Funding
Funding was provided by Society of American Gastrointestinal Surgeons (SAGES) 2020 Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Theresa Wang, Jennifer Underhill, Robert Tamer, Kyle Perry, and Kelly Haisley have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Meeting Presentation: SAGES 2023—Montreal, Canada.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, T.N., Underhill, J., Tamer, R. et al. Endoscopic impedance planimetry versus high-resolution manometry (HRM) for pre-operative motility evaluation in anti-reflux surgery. Surg Endosc 38, 377–383 (2024). https://doi.org/10.1007/s00464-023-10418-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10418-x