Abstract
Background
Stray energy transfer from monopolar instruments during laparoscopic surgery is a recognized cause of potentially catastrophic complications. There are limited data on stray energy injuries in robotic surgery. We sought to characterize stray energy injury in the form of superficial burns to the skin surrounding laparoscopic and robotic trocar sites. Our hypothesis was that stray energy burns will occur at all laparoscopic and robotic port sites.
Methods
We conducted a prospective, randomized controlled trial of patients undergoing elective unilateral inguinal hernia repair at a VAMC over a 4-year period. Surgery was performed via transabdominal preperitoneal approach either laparoscopic-assisted (TAPP) or robotic-assisted (rTAPP). A monopolar scissor was used to deliver energy at 30W coagulation for all cases. At completion of the procedure, skin biopsies were taken from all the port sites. A picro-Sirius red stain was utilized to identify thermal injury by a blinded pathologist.
Results
Over half (54%, 59/108) of all samples demonstrated thermal injury to the skin. In the laparoscopic group, 49% (25/51) samples showed thermal injury vs. 60% (34/57) in the robotic group (p = 0.548). The camera port was the most frequently involved with 68% (13/19) rTAPP samples showing injury vs. 47% (8/17) in the TAPP group (p = 0.503). There was no difference in the rate of injury at the working port site (rTAPP 53%, 10/19 vs. TAPP 47%, 8/17; p = 0.991) or the assistant port site (rTAPP 58%, 11/19 vs. TAPP 53%, 9/17; p = 0.873).
Conclusions
Stray energy causes thermal injury to the skin at port sites in the majority robotic laparoscopic TAPP inguinal hernia repairs. There is no difference in stray energy transfer between the laparoscopic and robotic platform. This is the first study to confirm in-vivo transfer of stray energy during robotic surgical procedures. More study is needed to determine the clinical significance of these thermal injuries.



Similar content being viewed by others
References
Willson PD, Mcanena OJ, Peters EE (1994) A fatal complication of diathermy in laparoscopic surgery. Minim Invasive Ther Allied Technol. https://doi.org/10.3109/13645709409152989
Guzman C, Forrester JA, Fuchshuber PR, Eakin JL (2019) Estimating the incidence of stray energy burns during laparoscopic surgery based on two statewide databases and retrospective rates: an opportunity to improve patient safety. Surg Technol Int. 34:30–34
Tucker RD (1995) Laparoscopic electrosurgical injuries: survey results and their implications. Surg Laparosc Endosc 5(4):311–317
Jones EL et al (2017) Stray energy transfer during endoscopy. Surg Endosc. https://doi.org/10.1007/s00464-017-5427-y
Overbey DM et al (2015) Surgical energy-based device injuries and fatalities reported to the Food and Drug Administration. J Am Coll Surg 221(1):197–205
Townsend NT et al (2017) Single-incision laparoscopic surgery increases the risk of unintentional thermal injury from the monopolar. Surg Endosc 31:3146–3151
Wikiel KJ et al (2021) Stray energy transfer in single-incision robotic surgery. Surg Endosc 35(6):2981–2985
Wikiel KJ et al (2023) Robotic stray energy with constant-voltage versus constant-power regulating electrosurgical generators. Surg Endosc 37(1):580–586
Fuller A et al (2012) Electrosurgical injuries during robot assisted surgery: insights from the FDA MAUDE database. In: Proceedings of SPIE, vol 8207, p 820714
Mendez-Probst CE et al (2011) Stray electrical currents in laparoscopic instruments used in da Vinci ® robot-assisted surgery: an in vitro study. J Endourol 25(9):1513–1517
Overbey DM et al (2021) Monopolar stray energy in robotic surgery. Surg Endosc 35(5):2084–2090
Jones EL et al (2013) Blend mode reduces unintended thermal injury by laparoscopic monopolar instruments: a randomized controlled trial. Surg Endosc 27(11):4016–4020
Asiyo-Vogel MN et al (1997) Histologic analysis of thermal effects of laser thermokeratoplasty and corneal ablation using Sirius-red polarization microscopy. J Cataract Refract Surg 23(4):515–526. https://doi.org/10.1016/s0886-3350(97)80208-8
Tang J et al (2000) Laser irradiative tissue probed in situ by collagen 380-nm fluorescence imaging. Lasers Surg Med 27:158–164. https://doi.org/10.1002/1096-9101(2000)27:2%3c158::AID-LSM7%3e3.0.CO;2-I
The R Foundation - R: The R Project for Statistical Computing https://www.r-project.org/foundation
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47(11):1245–1251. https://doi.org/10.1016/0895-4356(94)90129-5
Charlson ME et al (2008) The Charlson comorbidity index is adapted to predict costs of chronic disease in primary care patients. J Clin Epidemiol 61(12):1234–1240
Ek S, Meyer AC, Hedström M, Modig K (2022) Comorbidity and the association with 1-year mortality in hip fracture patients: can the ASA score and the Charlson Comorbidity Index be used interchangeably? Aging Clin Exp Res 34(1):129–136. https://doi.org/10.1007/s40520-021-01896-x
Karacan T et al (2018) Comparison of the thermal spread of three different electrosurgical generators on rat uterus: a preliminary experimental study. Gynecol Obstet Invest 83(4):388–396. https://doi.org/10.1159/000488675
Montero PN et al (2010) Insulation failure in laparoscopic instruments. Surg Endosc 24(2):462–465
Espada M, Munoz R, Noble BN et al (2011) Insulation failure in robotic and laparoscopic instrumentation: a prospective evaluation. Am J Obstet Gynecol 205(2):121
Jones EL, Mikami DJ (2018) Ch 19—Surgical energy. In: Fischer JE (ed) Fischer’s mastery of surgery, 7th edn. Wilkins, Philadelphia, pp 273–282
Voyles CR, Tucker RD (1992) Education and engineering solutions for potential problems with laparoscopic monopolar electrosurgery. Am J Surg 164(1):57–62
Robinson TN et al (2010) Surgeon-controlled factors that reduce monopolar electrosurgery capacitive coupling during laparoscopy. Surg Laparosc Endosc Percutan Tech 20(5):317–320
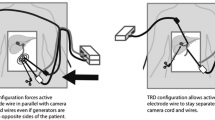
Robinson TN et al (2015) Separating the laparoscopic camera cord from the monopolar “bovie” cord reduces unintended thermal injury from antenna coupling: a randomized controlled trial. Ann Surg 261(6):1056–1060. https://doi.org/10.1097/SLA.0000000000000841
Hulka JF, Levy BS, Parker WH, Phillips JM (1997) Laparoscopic assisted vaginal hysterectomy: American Association of Gynecologic Laparoscopists’ 1995 Membership Survey. J Am Assoc Gynecol Laparosc 4:167–171
Nduka CC, Super PA, Monson JR, Darzi AW (1994) Cause and prevention of electrosurgical injuries in laparoscopy. J Am Coll Surg 179:161–170
Feldman LS et al (2012) FUSE (Fundamental Use of Surgical Energy™) Task Force. Surgeons don’t know what they don’t know about the safe use of energy in surgery. Surg Endosc 26(10):2735–2739. https://doi.org/10.1007/s00464-012-2263-y
Funding
Funding was provided by Society of American Gastrointestinal and Endoscopic Surgeons.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
This study was funded by SAGES Robotic Surgery Grant (2018). The authors, Drs. Wikiel, Bollinger, Montero, T. Jones, Robinson, and E. Jones have no other conflicts or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wikiel, K.J., Bollinger, D., Montero, P.M. et al. Stray energy injury during robotic versus laparoscopic inguinal hernia repair: a randomized controlled trial. Surg Endosc 37, 8771–8777 (2023). https://doi.org/10.1007/s00464-023-10331-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10331-3