Abstract
Background
It is thought the therapeutic benefit of per-oral endoscopic myotomy (POEM) in the treatment of esophageal dysmotility disorders is from longitudinal myotomy creation, but it is unknown if the submucosa contributes to the pathophysiology. This study investigates if submucosal tunnel (SMT) dissection alone contributes to POEM’s luminal changes as measured by EndoFLIP.
Methods
A single-center, retrospective review of consecutive POEM cases from June 1, 2011 to September 1, 2022 with intraoperative luminal diameter and distensibility index (DI) data as measured by EndoFLIP. Patients with diagnoses of achalasia or esophagogastric junction outflow obstruction were grouped by those with pre-SMT and post-myotomy measurements (Group 1) and those with a third measurement post-SMT dissection (Group 2). Outcomes and EndoFLIP data were analyzed using descriptive and univariate statistics.
Results
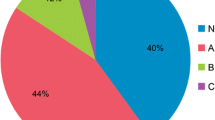
There were 66 patients identified, of whom 57 (86.4%) had achalasia, 32 (48.5%) were female, and median pre-POEM Eckardt score was 7 [IQR: 6–9]. There were 42 (64%) patients in Group 1, and 24 (36%) patients in Group 2, with no differences in baseline characteristics. In Group 2, SMT dissection changed luminal diameter by 2.15 [IQR: 1.75–3.28]cm, which comprised 38% of the median 5.6 [IQR: 4.25–6.3]cm diameter of complete POEM change. Similarly, the median post-SMT change in DI of 1 [IQR: 0.5–1.2]units comprised 30% of the median 3.35 [2.4–3.98]units overall change in DI. Post-SMT diameters and DI were both significantly lower than the full POEM.
Conclusions
Esophageal diameter and DI are significantly affected by SMT dissection alone, though not equaling the magnitude of diameter or DI changes from full POEM. This suggests that the submucosa does play a role in achalasia, presenting a future target for refining POEM and developing alternative treatment strategies.
Graphical abstract










Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- DI:
-
Distensibility index
- EGJ:
-
Esophagogastric junction
- EGJOO:
-
Esophagogastric junction outflow obstruction
- EndoFLIP:
-
Endoluminal functional luminal imaging probe
- IQR :
-
Interquartile range
- LES:
-
Lower esophageal sphincter
- LHM:
-
Laparoscopic Heller myotomy
- NAEDD:
-
Non-achalasia esophageal dysmotility disorders
- POEM:
-
Per-oral endoscopic myotomy
- SMT:
-
Submucosal tunnel
References
Pandolfino JE, Gawron AJ (2015) Achalasia: a systematic review. JAMA 313(18):1841–1852. https://doi.org/10.1001/jama.2015.2996 (PMID: 25965233)
Schlottmann F, Neto RML, Herbella FAM, Patti MG (2018) Esophageal achalasia: pathophysiology, clinical presentation, and diagnostic evaluation. Am Surg 84(4):467–472 (PMID: 29712590)
Yadlapati R, Kahrilas PJ, Fox MR, Bredenoord AJ, Prakash Gyawali C, Roman S, Babaei A, Mittal RK, Rommel N, Savarino E, Sifrim D, Smout A, Vaezi MF, Zerbib F, Akiyama J, Bhatia S, Bor S, Carlson DA, Chen JW, Cisternas D, Cock C, Coss-Adame E, de Bortoli N, Defilippi C, Fass R, Ghoshal UC, Gonlachanvit S, Hani A, Hebbard GS, Wook Jung K, Katz P, Katzka DA, Khan A, Kohn GP, Lazarescu A, Lengliner J, Mittal SK, Omari T, Park MI, Penagini R, Pohl D, Richter JE, Serra J, Sweis R, Tack J, Tatum RP, Tutuian R, Vela MF, Wong RK, Wu JC, Xiao Y, Pandolfino JE (2021) Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0©. Neurogastroenterol Motil. 33(1):e14058. https://doi.org/10.1111/nmo.14058
Sadowski DC, Ackah F, Jiang B, Svenson LW (2010) Achalasia: incidence, prevalence and survival: a population-based study. Neurogastroenterol Motil 22(9):e256–e261. https://doi.org/10.1111/j.1365-2982.2010.01511.x (Epub 2010 May 11 PMID: 20465592)
Scherer JR, Kwiatek MA, Soper NJ, Pandolfino JE, Kahrilas PJ (2009) Functional esophagogastric junction obstruction with intact peristalsis: a heterogeneous syndrome sometimes akin to achalasia. J Gastrointest Surg. 13(12):2219–2225. https://doi.org/10.1007/s11605-009-0975-7
Kroch DA, Grimm IS (2018) POEM for achalasia. Am Surg 84(4):489–495 (PMID: 29712594)
Zaninotto G, Bennett C, Boeckxstaens G, Costantini M, Ferguson MK, Pandolfino JE, Patti MG, Ribeiro U Jr, Richter J, Swanstrom L, Tack J, Triadafilopoulos G, Markar SR, Salvador R, Faccio L, Andreollo NA, Cecconello I, Costamagna G, da Rocha JRM, Hungness ES, Fisichella PM, Fuchs KH, Gockel I, Gurski R, Gyawali CP, Herbella FAM, Holloway RH, Hongo M, Jobe BA, Kahrilas PJ, Katzka DA, Dua KS, Liu D, Moonen A, Nasi A, Pasricha PJ, Penagini R, Perretta S, Sallum RAA, Sarnelli G, Savarino E, Schlottmann F, Sifrim D, Soper N, Tatum RP, Vaezi MF, van Herwaarden-Lindeboom M, Vanuytsel T, Vela MF, Watson DI, Zerbib F, Gittens S, Pontillo C, Vermigli S, Inama D, The LDE (2018) ISDE achalasia guidelines. Dis Esophagus. https://doi.org/10.1093/dote/doy071
Eckardt AJ, Eckardt VF (2011) Treatment and surveillance strategies in achalasia: an update. Nat Rev Gastroenterol Hepatol 8(6):311–319. https://doi.org/10.1038/nrgastro.2011.68 (Epub 2011 Apr 26 PMID: 21522116)
Ehlers AP, Oelschlager BK, Pellegrini CA, Wright AS, Saunders MD, Flum DR, He H, Farjah F (2017) Achalasia treatment, outcomes, utilization, and costs: a population-based study from the United States. J Am Coll Surg. 225(3):380–386. https://doi.org/10.1016/j.jamcollsurg.2017.05.014
Horgan S, Hudda K, Eubanks T, McAllister J, Pellegrini CA (1999) Does botulinum toxin injection make esophagomyotomy a more difficult operation? Surg Endosc 13:576–579
Swanström LL (2019) Achalasia: treatment, current status and future advances. Korean J Intern Med 34(6):1173–1180. https://doi.org/10.3904/kjim.2018.439
Cheng JW, Li Y, Xing WQ, Ly HW, Wang HR (2017) Laparoscopic Heller myotomy is not superior to pneumatic dilation in the management of primary achalasia: conclusions of a systematic review and meta-analysis of randomized controlled trials. Medicine 96:e5525
Schlottmann F, Patti MG (2018) Esophageal achalasia: current diagnosis and treatment. Expert Rev Gastroenterol Hepatol 12(7):711–721
Filicori F, Dunst CM, Sharata A, Abdelmoaty WF, Zihni AM, Reavis KM, Demeester SR, Swanström LL (2019) Long-term outcomes following POEM for non-achalasia motility disorders of the esophagus. Surg Endosc 33:1632–1639. https://doi.org/10.1007/s00464-018-6438-z
Bernardot L, Roman S, Barret M, Vitton V, Wallenhorst T, Pioche M, Chaussade S, Gonzalez J-M, Ponchon T, Prat F, Barthet M, Vergniol J, Chabrun E, Zerbib F (2020) Efficacy of per-oral endoscopic myotomy for the treatment of non-achalasia esophageal motor disorders. Surg Endosc 34:5508–5515. https://doi.org/10.1007/s00464-019-07348-y
Khashab MA, Familiari P, Draganov PV, Aridi HD, Cho JY, Ujiki M, Rio Tinto R, Louis H, Desai PN, Velanovich V, Albéniz E, Haji A, Marks J, Costamagna G, Devière J, Perbtani Y, Hedberg M, Estremera F, Martin Del Campo LA, Yang D, Bukhari M, Brewer O, Sanaei O, Fayad L, Agarwal A, Kumbhari V, Chen Y-I (2018) Peroral endoscopic myotomy is effective and safe in non-achalasia esophageal motility disorders: an international multicenter study. Endosc Int Open 6:E1031–E1036. https://doi.org/10.1055/a-0625-6288
Morley TJ, Mikulski MF, Rade M, Chalhoub J, Desilets DJ, Romanelli JR (2022) Per-oral endoscopic myotomy for the treatment of non-achalasia esophageal dysmotility disorders: experience from a single high-volume center. Surg Endosc. https://doi.org/10.1007/s00464-022-09596-x
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42:265–271. https://doi.org/10.1055/s-0029-1244080
Inoue H, Sato H, Ikeda H, Onimaru M, Sato C, Minami H, Yokomichi H, Kobayashi Y, Grimes KL, Kudo S (2015) Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg 221:256–264. https://doi.org/10.1016/j.jamcollsurg.2015.03.057
Park CH, Jung DH, Kim DH, Lim C-H, Moon HS, Park JH, Jung H-K, Hong SJ, Choi SC, Lee OY et al (2019) Comparative efficacy of per-oral endoscopic myotomy and Heller myotomy in patients with achalasia: a meta-analysis. Gastrointest Endosc 90:546–558. https://doi.org/10.1016/j.gie.2019.05.046
Sanaka MR, Hayat U, Thota PN, Jegadeesan R, Ray M, Gabbard SL, Wadhwa N, Lopez R, Baker ME, Murthy S, Raja S (2016) Efficacy of peroral endoscopic myotomy vs other achalasia treatments in improving esophageal function. World J Gastroenterol 22:4918–4925. https://doi.org/10.3748/wjg.v22.i20.4918
American Society for Gastrointestinal Endoscopy PIVI Committee, Chandrasekhara V, Desilets D, Falk GW, Inoue H, Romanelli JR, Savides TJ, Stavropoulos SN, Swanstrom LL (2015) The American society for gastrointestinal endoscopy PIVI (preservation and incorporation of valuable endoscopic innovations) on peroral endoscopic myotomy. Gastrointest Endosc 81:1087-1100.e1. https://doi.org/10.1016/j.gie.2014.12.007
Patel K, Abbassi-Ghadi N, Markar S, Kumar S, Jethwa P, Zaninotto G (2016) Peroral endoscopic myotomy for the treatment of esophageal achalasia: systematic review and pooled analysis. Dis Esophagus Off J Int Soc Dis Esophagus 29:807–819. https://doi.org/10.1111/dote.12387
Pandolfino JE, de Ruigh A, Nicodème F, Xiao Y, Boris L, Kahrilas PJ (2013) Distensibility of the esophagogastric junction assessed with the functional lumen imaging probe (FLIP™) in achalasia patients. Neurogastroenterol Motil Off J Eur Gastrointest Motil Soc 25:496–501. https://doi.org/10.1111/nmo.12097
Rieder E, Swanström LL, Perretta S, Lenglinger J, Riegler M, Dunst CM (2013) Intraoperative assessment of esophagogastric junction distensibility during per oral endoscopic myotomy (POEM) for esophageal motility disorders. Surg Endosc 27:400–405. https://doi.org/10.1007/s00464-012-2484-0
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE et al (2015) The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27(2):160–174
Kane ED, Desilets DJ, Wilson D, Leduc M, Budhraja V, Romanelli JR (2018) Treatment of achalasia with per-oral endoscopic myotomy: analysis of 50 consecutive patients. J Laparoendosc Adv Surg Tech A 28:514–525. https://doi.org/10.1089/lap.2017.0588SuB
Callahan ZM, Novak S, Kuchta K, Ujiki MB (2020) Using impedance planimetry (EndoFLIP) to evaluate myotomy and predict outcomes after surgery for achalasia. J Gastrointest Surg Off J Soc Surg Aliment Tract 24:964–971. https://doi.org/10.1007/s11605-020-04513-w
R Core Team (2021) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/.
Jain AS, Carlson DA, Triggs J, Tye M, Kou W, Campagna R, Hungness E, Kim D, Kahrilas PJ, Pandolfino JE (2019) Esophagogastric junction distensibility on functional lumen imaging probe topography predicts treatment response in achalasia-anatomy matters! Am J Gastroenterol 114(9):1455–1463. https://doi.org/10.14309/ajg.0000000000000137.PMID:30741739;PMCID:PMC6682473
Teitelbaum EN, Soper NJ, Pandolfino JE, Kahrilas PJ, Hirano I, Boris L, Nicodème F, Lin Z, Hungness ES (2015) Esophagogastric junction distensibility measurements during Heller myotomy and POEM for achalasia predict postoperative symptomatic outcomes. Surg Endosc. 29(3):522–528. https://doi.org/10.1007/s00464-014-3733-1
Teitelbaum EN, Soper NJ, Pandolfino JE, Kahrilas PJ, Boris L, Nicodème F, Lin Z, Hungness ES (2014) An extended proximal esophageal myotomy is necessary to normalize EGJ distensibility during Heller myotomy for achalasia, but not POEM. Surg Endosc. 28(10):2840–2847. https://doi.org/10.1007/s00464-014-3563-1
Knowles TB, Jackson AS, Chang SC, Schembre DB, Farivar AS, Aye RW, Louie BE (2022) Changes in distensibility index during an incremental POEM myotomy. J Gastrointest Surg 26(6):1140–1146. https://doi.org/10.1007/s11605-022-05278-0 (Epub 2022 Mar 1 PMID: 35233701)
Holmstrom AL, Campagna RAJ, Alhalel J, Carlson DA, Pandolfino JE, Hungness ES, Teitelbaum EN (2021) Intraoperative FLIP distensibility during POEM varies according to achalasia subtype. Surg Endosc 35(6):3097–3103. https://doi.org/10.1007/s00464-020-07740-z (Epub 2020 Jun 29 PMID: 32601759)
Fujiyoshi Y, Inoue H, Fujiyoshi MRA, de Rodriguez Santiago E, Nishikawa Y, Toshimori A, Tanabe M, Shimamura Y, Sumi K, Ono M, Shiwaku H, Ikeda H, Onimaru M (2023) Learning curve for peroral endoscopic myotomy in therapeutic endoscopy experts and nonexperts: large single-center experience. Dig Endosc. 35(3):323–331. https://doi.org/10.1111/den.14435
Lv H, Zhao N, Zheng Z, Wang T, Yang F, Jiang X, Lin L, Sun C, Wang B (2017) Analysis of the learning curve for peroral endoscopic myotomy for esophageal achalasia: single-center, two-operator experience. Dig Endosc 29(3):299–306. https://doi.org/10.1111/den.12763 (Epub 2017 Jan 12 PMID: 27859721)
Acknowledgements
None.
Funding
There was no internal or external funding for this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
John R. Romanelli receives research funding from Davol, and consulting fees from New View Surgical. Timothy J. Morley, Matthew F. Mikulski, Alicja Zalewski, and David J. Desilets report no conflicts of interests or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previous presentation: Data from this work was accepted for presentation at the Society of American Gastrointestinal and Endoscopic Surgeons 2023 Annual Meeting, Montreal, QC, Canada, March 2023.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morley, T.J., Mikulski, M.F., Zalewski, A. et al. What role does the submucosa play in the pathophysiology and treatment of achalasia? An analysis of impedance planimetry during POEM. Surg Endosc 37, 7923–7932 (2023). https://doi.org/10.1007/s00464-023-10260-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10260-1