Abstract
Background
The reperfused human cadaver is a validated simulator for surgery. We aimed to use it as a colonoscopy simulator.
Methods
Novices, intermediates and skilled participants in gastrointestinal endoscopy were included. They performed one colonoscopy on a reperfused human cadaver and reaching rates, time, and length needed to reach anatomical landmarks were reported for construct validity analysis. We also assessed our model realism (SRS survey), educational content (CVS survey) and task load (NASA-TLX index). Score items were collected and defined as “favorable” when items were rated ≥ 5/7 with an inter-quartile range (IQR) overlapping four, and “very favorable” when rated ≥ 5/7 with an IQR excluding four (neutral).
Primary endpoints were the rectosigmoid junction (RSJ) reaching rate and the descending colon (DC) reaching time. Secondary objectives were SRS, CVS and NASA-TLX questionnaire results.
Results
A total of 11 skilled participants, 5 intermediates and 8 novices were included. Skilled participants reached RSJ more often than novice and intermediary groups, respectively, 100%, 80% and 75% without differing significantly. They reached DC more frequently (100% for skilled, 80% for intermediates and 50% for novices, p = 0.018). The median time to reach RSJ (59, 272 and 686 s for skilled, intermediates and novices group, respectively) and DC (90, 534 and 1360 s for skilled, intermediates and novices) was significantly shorter for skilled participants (both p < .01).
Nineteen out of the 22 items composing the realism survey obtained “very favorable” and “favorable” scores. Educational content was designated as “very favorable”. Mental, physical, and technical demands were gradually higher the lower the initial level of experience.
Conclusions
Reperfused human cadaver model has the potential to be valid simulation tool for diagnostic colonoscopy training.
Similar content being viewed by others
Diagnostic and therapeutic colonoscopy is a cornerstone in the gastroenterologist’s (GE) set of skills. Several years of practice are needed to perform complete, safe and quick procedures. Learning curves have enabled the estimation of a minimal competency threshold recognizing the ability to perform a procedure correctly [1,2,3,4]. Simulation-based training has been widely developed and helps trainees to achieve curriculum fulfilment. It improves endoscopy teaching and trainees’ endoscopic performance, especially in the early stages [5,6,7,8]. Novices can acquire skills in handling, progression, anatomy and more difficult techniques to optimize their valuable time in a caring environment without compromising patients’ safety and comfort [9, 10].
Validated simulators in gastrointestinal endoscopy (GIE) consist of mechanical, animal-based, or virtual reality (VR) models. They all have their advantages and limitations in terms of realism, force feedback, educational feedback or ethical concerns [11, 12]. Unfortunately, their high cost and low accessibility hamper residents’ and fellows’ learning skills. There is a need for an affordable and accessible alternative.
The Human-cadaveric model is a historical simulation tool for surgical training programs due to its high anatomical fidelity and great educational value [13, 14]. Data about the human-cadaveric model in GIE training is inexistent regarding lower gastrointestinal endoscopy. The main objective was to evaluate the feasibility of a human-cadaveric model as a colonoscopy training model. Secondary objectives were to assess realism, effectiveness as a learning tool and task load.
Material and methods
We conducted a monocentric prospective feasibility and validity study. Every simulation was performed at the medical school’s Anatomy Department (Université de Reims Champagne Ardenne) from April to July 2021. The Anatomy Department provides anatomy lessons, dissection lectures, surgical and emergency training on cadavers to its students. Cadavers can be used either fresh or defrosted. All of them were tested negative for COVID-19 (RT-PCR method) and respected the core ethical practice in human dissection (International Federation of Associations of Anatomists, IFAA, 2012). cadavers were individuals who had bequeathed their bodies to scientific research. Anonymity is ensured by the administrative process. We had no access to cadavers’ medical or surgical records. We selected experts in GIE (AR, GC, MB), medical education (AR, IC, CP, GC, MB) and simulation-based training (CP). Regular informal discussions allowed us to conceive a step-by-step reproducible protocol of cadaver preparation and bowel cleansing.
Reperfused human cadaver colonoscopy simulator (RHCCS)
Cadavers were slowly defrosted at 15 °C 3–5 days before use and were connected to a Pulse for Practice® device (P4P®, Simedys® 2020, Poitiers, France). P4P® system is a specific device allowing pulsatile arterial and venous revascularization by connecting eight catheters infusing 37 °C-heated fake blood in both femoral and common carotid arteries (input) and both femoral and internal jugular veins (output) (Photo 1A). It aims to recolor, reheat organs and tissues and restore an intravascular pressure with a pump to simulate blood circulation [15, 16]. Many parameters are available to enhance realism such as blood pressure in mmHg, percentage of diastole duration, pulse per minute and continuous or pulsating mode. The cadavers in this study could have been used in previous medical or surgical training sessions as long as these excluded digestive surgery exercises modifying colonic anatomy. Cadavers were not embalmed or formalin-fixed, and could be used for 2 days in a row. Each cadaver was used either until excessive damage, such as intestinal perforation, compromised the simulation experience, or until the end of the session.
Bowel preparation
A digital rectal examination was performed to confirm anus presence and extract hard stools from the rectum. A rectal probe or rectally inserted Flexi-Seal® (ConvaTec, Reading, United Kingdom) (Photo 1B) device was used to send cool water into the colon lumen for at least 3 min until clean water emerged to achieve complete colonic defrosting and stool evacuation. After satisfactory stool extraction, a first colonoscopy was performed by one of the investigators (AR, MB) to check colonic anatomy, improve mucosal cleaning using the endoscopic flushing pump and determine the highest reachable point by trainees. Every cadaver with a major colonic resection or at least, left colectomy, was not used.
We used the Olympus® EVIS EXERA III Video Colonoscope (CF-H190L/I) (Olympus Corporation, Tokyo, Japan) (Photo 1C), and the entire set of endoscopy equipment was for sole use of the anatomy department.
Study protocol
All participants were selected among volunteers and spontaneous offers by caregivers (medical students, residents, and medical staff) at the Reims University Medical Center. Each screened participant underwent a basic demographic self-questionnaire (sex, age, dominant hand, job), signed an agreement-of-participation form, and was asked about their manual abilities and endoscopic experience (see Supplementary material). Based on their endoscopy experience, participants were divided into three distinct groups:—novices, who had never performed GIE,—intermediates who had already performed one to ten colonoscopies alone and—skilled participants, who had already performed > 10 complete colonoscopies in complete autonomy.
Several sessions were scheduled. Participants from different group-levels were assigned to a session and started the colonoscopy according to their order of arrival. All included participants received a short 5-min tutorial briefing about gastrointestinal endoscopes and how to use them.
-
(i)
We used objective performance parameters such as time and length to different anatomical landmarks (rectosigmoid junction (RSJ), descending colon (DC), splenic flexure, hepatic flexure, and caecum), including total time of procedure and maximal point of insertion. A maximum of 25 min was allowed for each participant to reach the left colon. Investigators performed a complete supervision including live feedback and a debriefing session an open evaluation of each participant during the colonoscopy.
Each participant’s experience was debriefed, and a multidimensional assessment of participants’ experience was performed at the end of each procedure.
-
(ii)
Skilled participants completed a simulation realism survey (SRS) to evaluate the similarity between the human-cadaver model and human-living endoscopy (face validity). Detailed SRS is available in Supplementary material—Figure S1. Each of these parameters was measured using a Likert scale (1 = strongly disagree, 4 = neutral, 7 = strongly agree). Technical difficulty fidelity (resemblance of technical difficulty to real-life conditions) was also measured with a Likert Scale (1 = easier, 4 = neutral, 7 = harder than human living colonoscopy). Realism was defined as favorable when items were rated over or equal to 5 with an inter-quartile range (IQR) overlapping 4, and very favorable when rated over or equal to 5 with an inter-quartile range (IQR) excluding 4 (neutral). Technical difficulty fidelity was defined as ideal when equalling 4 or overlapping.
-
(iii)
Skilled participants also assessed the educational quality of this model (content validity) using a content validity survey (CVS) designed by Jones et al. [17], based on the GAGES evaluation for endoscopic proficiency [18]. The CVS form is available as supplementary material—Figure S2. It is composed of seven items on a scale from one to seven (1 = strongly disagree, 4 = neutral, 7 = strongly agree). The definition of favorable and very favorable items results was the same as for the SRS.
-
(iv)
Finally, we used the multidimensional NASA Task Load Index (NASA TLX) to assess perceived mental and physical load (Supplementary material—Figure S3). We added one item (mental disturbance) to the original questionnaire (mental demand, physical demand, temporal demand, performance, technical issue, and frustration) to encompass this dimension. Each item had a scale score from 1 (very low) to 20 (very high), except for the item “performance” where 1 is for “perfect” and 20 for “failure”.
The main objective was to evaluate the feasibility of using a human-cadaveric model as a colonoscopy training model (construct validity). Primary endpoints were RSJ reaching rate and DC reaching time between groups. Secondary objectives were to assess realism (face validity), effectiveness as a learning tool (content validity) and task load using SRS, CVS and NASA-TLX questionnaires, respectively. Every participant signed a written consent before inclusion. No institutional review board approval was needed as this was a non-interventional monocentric study.
Data analysis
Quantitative data were described with their median and IQR (Q1–Q3), and compared with the non-parametric Kruskal–Wallis test. Qualitative data were described using frequencies and percentages and compared with the Chi-square test or Fisher’s exact test when appropriate. No minimum number of participants was required for this study as its main purpose was exploratory. When RSJ was not reached, inserted colonoscope length was not considered and a standard time of 25 min was assigned to the participant. Statistical significance was defined as a p-value < 0.05 for all tests. All statistical analyses were performed using R (R Development Core Team, 2005). All authors and co-authors had access to the study data, reviewed and approved the final manuscript.
Ethical concern
Cadavers had been donated to the Department of Anatomy, Faculty of Medicine and University Hospital, Champagne Ardenne university, for anatomical education and research purposes. As described by the French laws, all the ethical rules concerning work on cadaveric material in our institution (Law 94‐653 of July 29, 1994 relative to the respect of the human body) were followed for this study. The staff supervising cadaver manipulations was trained and ensured the respect of ethical principles.
Results
A total of 31 potential participants volunteered or were invited. Among them, seven refused to take part in the study (four in our medical staff, two third-year gastroenterology residents, and one GIE nurse). Eleven skilled participants (median age of 29, IQR: 27–39), five intermediates (median age of 26, IQR: 25–27), and eight novices (median age of 24, IQR: 23.8–25.5) were included. Included participants’ characteristics are presented in Table 1 and supplementary material—Table S1A and B. One of the novices included was a pneumologist resident who had already performed bronchoscopies on a living patient. A total of six cadavers were used to perform 24 colonoscopies.
Skilled participants were composed of five GE residents and six members of staff with different levels of experiences. Five participants in the intermediary and skilled group had performed simulation-based endoscopy on human cadavers prior to this study.
There was no difference between groups in terms of their dominant hand or practice of activities requiring dexterity (musical instrument or video games).
A video of a simulated colonoscopy is available (Video 1).
-
(i)
Construct validity
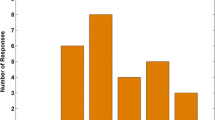
Skilled participants reached RSJ more often than novice and intermediary groups, respectively, 100%, 80% and 75% without significantly differing (Table 2). They also reached other anatomic landmarks more frequently: DC (p = 0.018) and splenic flexure (p < 0.01). The time to reach RSJ and DC was significantly shorter for skilled participants (p < 0.01 and p < 0.01, respectively) (Fig. 1). Furthermore, reaching rates and speed gradually increased according to experience.
No difference was observed in inserted scope length to reach different anatomical landmarks. Colonic perforation occurred twice: once by a novice and once by an expert who mentioned that she had not noticed the typical pre-perforation “red flags”.
-
(ii)
Face validity
Simulator fidelity assessment results by skilled participants are shown in Supplementary Material—Table S2. Level of realism was rated as very favorable in “endoscopic view” (5.0, IQR: 4.5–6.0), “stool look” (5.0, IQR: 4.2–6.0), “colon length” (6.0, IQR: 5.8–7.0), “haustra/folds” (6.0, IQR: 4.5–7.0), “sigmoid angle” (5.0, IQR: 5.0–6.0), “splenic flexure” (5.0, IQR: 5.0–6.0), “hepatic flexure” (5.5, IQR: 5.0–6.0), “resistance to scope advancement” (6.0, IQR: 4.5–6.5), “paradoxical scope motion” (5.0, IQR: 4.5–7.0), “location of paradoxical motion encountered” (6.0, IQR: 5.0–7.0), and “frequency and degree of looping occurrence” (5.0, IQR: 5.0–6.0) items. Seven other items were rated as favorable: “mucosal realism”, “mucosal vascularization”, “response to loop reduction techniques”, “response to abdominal compressive maneuvers”, “occurrence of abdominal distension after excessive insufflation”, “exsufflation quality assessment at the end of the procedure”, and “overall simulation fidelity”. Technical difficulty was comparable to that of a normal colonoscopy (5.0, IQR 4,0 to 5,0).
-
(iii)
Content validity
Content validity results are presented in Supplementary Material—Table S3. Items “This simulator closely replicates the necessary skills for a real colonoscopy”, “This simulator would be effective to teach residents/fellows scope navigation”, “This simulator would be effective to teach residents/fellows basic maneuvers such as insufflation, suction and retroflexion”, “This simulator would be effective to teach residents/fellows to keep a clear endoscopic field”, and “This simulator would be effective to teach residents/fellows instrumentation (biopsy and snare polypectomy)” scored > 5, without overlapping the neutral score of 4.
-
(iv)
Workload study
Modified NASA-TLX survey showed that mental, physical, and technical demands were gradually higher the lower the level was (Supplementary material—Table S4). Novices were significantly less disturbed working on human cadavers than intermediaries or skilled participants (p = 0.029).
A Time to reach the rectosigmoid junction per group; B Time to reach the descending colon per group; C Total colonoscopy time per group. Participants who did not reach the rectosigmoid junction and descending colon are represented by orange points. Participants who reached the rectosigmoid junction and descending colon are represented by blue points
Discussion
After bowel preparation, re-perfused cadavers offer a reliable simulation model for colonoscopy. In this study, construct, face and content validation were provided to define the RHCCS as a new tool for colonoscopy training.
Traditionally, endoscopy training is based on an apprenticeship model with a student under the direct supervision of an expert, performing endoscopic procedures on a living patient. The European Society of Gastrointestinal Endoscopy and American Society for Gastrointestinal Endoscopy (ESGE and ASGE) developed a list of core technical, non-technical, and cognitive skills to acquire for colonoscopy [4, 19]. ESGE suggests that personal experience of at least 300 upper GIE and/or 300 lower GIE is required to achieve general competence [4]. Training on living patients brings with it ethical concerns as it includes risks of bleeding (2,4/1000) and intestinal perforation (0,3/1000) [20]. Therefore, simulation-based training allows fellows to perform procedures in a safe and stressless environment for patients and for themselves. GIE simulators include mechanical trainers, animal-based models, or virtual reality (VR) tools. Nevertheless, prohibitive costs, restricted accessibility and sometimes low educational quality hinder the integration of simulation-based training into the GIE curriculum [21, 22].
The human cadaver is the historical and gold-standard validated training tool for surgical residents. It provides a high level of realism in terms of technical gesture and feel of human tissue and it mimics the operating conditions perfectly (body positions on the operating table, operating fields, anatomy…) [13, 14]. It increases residents’ confidence and may lead to earlier operative autonomy [23]. Moreover, each cadaver can be reused for different surgical training workshops. Despite its validity in the surgical simulation domain, the human cadaver model has never been validated in GIE. An Indian team have described the use of cadavers to perform upper GIE simulation and endoscopic techniques without face, content and construct validation [18, 24]. This study confirmed that cadavers are usable for upper GIE simulation. However, no colonoscopy has ever been performed previously. With the RHCCS, we reported a reliable tool for colonoscopy simulation on cadavers for the first time.
In France, endoscopic simulation training is based on animal ex-vivo (79%) and VR models (71%) used in 14 workshops around the country [21]. Unfortunately, french residents do not benefit from training with these simulators as they are only exposed to them once or twice during their 5-year programme [21]. In the USA, simulation-based training is represented by computerized (61.5%), mechanical (30.8%) and animal-explanted (7.7%) tools in fewer than half of all training centers [22]. Moreover, a computerized simulator costs between $50,000 and $140,0008. Composite animal simulators may seem cheaper (e.g., $2,200–$2,600 for EASIE-R3® simulator, Endosim, Büchenbach, Germany), but require the purchase of the main unit and single-use prepared porcine organs (from $125 for porcine stomach specimen to $350 for complete porcine explant specimen in Endosim). In French medical schools, cadavers are donations. The cost of a cadaver preparation could be estimated around 160€ (including 70€ of infusion, 50€ of fake blood, 40€ of protection equipment). However, a P4P device costs around 80 000 € but can be used for all simulations (including surgical simulations). The contribution of the P4P device in this setting remains unclear and also needs to be validated. However, this added equipment to the model could play a role in the recoloration of the mucosae. The human cadaver model can be mutualized: it can become a shared simulation device between medical and surgical specialties lowering its economic burden and enhancing the teaching of multidisciplinarity. To be further implemented if validated, every academic center with a cadaver dissection theater would need to be trained to cadaveric bowel cleansing and taking into account the ethical dimension. In our study, we have also shown that colonoscopy on a human cadaver is possible with a simple and thorough bowel preparation in advance. This reproducible bowel cleansing protocol allowed fellows to perform colonoscopies with high fidelity without either disrupting the educational purpose or increasing its cost.
The cadaver model was described as very favorable in terms of realism for 11 items, and favorable for eight items over 22. The RHCCS model can accurately replicate the visual and mechanical properties of a colonoscopy on a living patient (e.g., occurrence of paradoxical motion, resistance to scope advancement and intestinal loop). Realism is a fundamental aspect of a validated simulation training tool. In surgery, realism is an essential tool allowing comparison between different laparoscopic training systems [25]. In GIE, several studies have investigated the realism of VR, mechanical and ex-vivo colonoscopy simulators [26]. Mechanical simulators reproduced satisfying mechanical properties and realistic force feedback [11]. Nevertheless, visual realism is not achieved with a score of only 32,69/100 for the Koken Colonoscopy Training Model Type 1-B device, and a score of only 21,77/100 for the Kyoto Kagaku Colonoscope Training Model [27]. These scores were also low for VR devices such as the Endoscopy AccuTouch System, Immersion Medical Corporation, and the Gi Mentor II, Simbionix Corporation, with 50.64/100 and 42.86/100, respectively. Finally, the visual realism of the ex-vivo colonoscopy bovine model obtained a score of 6.0/7 [22]. However, as these studies used different scores with heterogeneous low-numbered populations, no face-to-face comparison seems appropriate. A face-to-face comparison with other simulators is necessary to better investigate the input of this model.
The RHCCS can differentiate between participants based on their endoscopic level thus ensuring a high construct validity. Even if no significant statistical difference in RSJ reaching rate was shown between the three groups, we can observe a gradual increase in reaching rates and speed, according to experience. Construct validity of the RHCCS may be an opportunity for certification in GIE before practicing on a patient.
Moreover, a good endoscopic simulator should be effective for teaching colonoscopy competencies (evidence of content validity). Skilled participants have recognized the educational quality of this model, based on the GAGES criteria for endoscopic proficiency [18]. All items obtained a very favorable score. The model’s educational value needs to be validated in a larger multicentric cohort. The RHCCS is a valid tool regarding content validity.
Finally, the mental, physical and technical load survey based on the modified NASA Task Load Index is a good measurement of each participant’s level. As expected, the lower the level of skills, the more demanding the task. This assessment, although not usually used in validation studies of endoscopic simulation models, highlights the stress that endoscopy can generate for inexperienced students. This confirms that the RHCCS offers realistic conditions for GIE trainees. In the future, comparison with the modified NASA-TLX score in real-life colonoscopies on a living patient could be interesting. With reference to the additional question included in this study, the sight of a cadaver does not seem to be a problem for those who accepted to be included, even for younger or inexperienced participants.
Multimodal evaluation is the mainstay of simulation model validation. It measures the model’s ability to reflect the reality of a simulated situation. In our RHCCS model, we successively showed high visual, mechanical and task load fidelity, capacity to distinguish operators based on their experience, and educational purpose.
Some limitations in our study can be pointed out, however. First, albeit its prospective format, it is a monocentric study with a limited number of participants which results in low statistical power. Secondly, no minimum number of participants was required for this study as the main purpose was exploratory and mainly qualitative. Nevertheless, as it is considered a pilot study, the number of included participants seems acceptable. The limited number of participants per group limits the statistical analysis in its interpretation. The definition of our skilled group could be criticized as we considered participants with > 10 autonomous colonoscopies as being “skilled”. This definition is not in line with the definition of other authors who set the thresholds at > 200 or sometimes > 1000 [28, 29]. Our main objective was designed for initial endoscopic education and essential skill acquisition in a mistake-tolerant environment. For this reason, and to lower ambiguity, we chose to call this group “skilled participants” instead of “experts”. Also, only one colonoscopy per participant may be insufficient to conclude on the validity of the model and more powerful longitudinal studies are required.
We can also notice that one participant in the novice group had a small amount of experience in bronchoscopy, which could have enhanced the novice group’s performance score. Despite this, the skilled group performed significantly faster than the other two groups. The gap between the skilled participants and the other two groups suggests that this model could be a useful tool to make the intermediary progress towards expertise.
We only included participants who had accepted to perform a colonoscopy on a human cadaver. We obtained seven refusals (five in our medical staff, one in intermediaries and one in novices). The acceptability of human cadavers as a simulation model has to be investigated because of personal or religious convictions. Nevertheless, this kind of workshop is commonplace in the medical curriculum (e.g., suture or dissection classes) and the majority of medical students are voluntary and agree to train on human cadavers. Additional measures could be applied to lower the emotional burden of this training (e.g., covering bodies with surgical drapes).
This model could also lack sufficient feedback. Contrary to VR devices, the human cadaveric model does not provide objective quality measurement tools such as patient’s pain level, percentage of mucosa visualized, or amount of air insufflated, which have significant educational value. Supervision by skilled endoscopists seems mandatory to guarantee the educational value of the model. To provide a better level of content validity, future research should compare the ability to perform high-quality GIE depending on the learning device used.
Also, according to skilled participants, the colonic mucosa lacked realism in terms of mucosal color despite reperfusion with a P4P® device. We suggested that colonic mucosal rendering could be improved with the use of a fresh cadaver rather than an defrosted cadaver, and higher blood pressure from the mechanical pump of the P4P® device.
Two intestinal perforations occurred during our study: one by a novice, and one by a skilled participant. Perforation on a human cadaveric model may thus occur more frequently as it seems to show fewer pre-perforation red flags than on a living body (e.g., whitening mucosa, vanishing capillaries).
The RHCCS is a satisfying model in terms of realism and educational value, which can be improved over time. In the future, this model could be used as a way to teach the skill of therapeutic colonoscopy (e.g., snare polypectomy, endoscopic clipping, electrocautery, submucosal injection).
This feasibility study on the reperfused human cadaver model for colonoscopy simulation demonstrated construct, face and content validities. This study calls for more robust studies to definitely validate the use of our human-cadaver simulation model for diagnostic colonoscopy training and evaluation.
Abbreviations
- ASGE:
-
American Society for Gastrointestinal Endoscopy
- CVS:
-
Content Validity Survey
- DC:
-
Descending colon
- ESGE:
-
European Society of Gastrointestinal Endoscopy
- GE:
-
Gastroenterologist
- GIE:
-
Gastrointestinal endoscopy
- IQR:
-
Inter-quartile range
- NASA TLX:
-
NASA Task Load Index
- P4P:
-
Pulse for Practice® device
- RHCCS:
-
Reperfused Human Cadaver Colonoscopy Simulator
- RSJ:
-
Rectosigmoid junction
- SRS:
-
Simulation realism survey
- VR:
-
Virtual reality
References
Ward ST, Hancox A, Mohammed MA et al (2017) The learning curve to achieve satisfactory completion rates in upper GI endoscopy: an analysis of a national training database. Gut 66:1022–1033. https://doi.org/10.1136/gutjnl-2015-310443
Ward ST, Mohammed MA, Walt R et al (2014) An analysis of the learning curve to achieve competency at colonoscopy using the JETS database. Gut 63:1746–1754. https://doi.org/10.1136/gutjnl-2013-305973
Sedlack RE, Coyle WJ, Sedlack RE et al (2016) Assessment of competency in endoscopy: establishing and validating generalizable competency benchmarks for colonoscopy. Gastrointest Endosc 83:516-523.e1. https://doi.org/10.1016/j.gie.2015.04.041
Dekker E, Houwen BBSL, Puig I et al (2020) Curriculum for optical diagnosis training in Europe: European Society of Gastrointestinal Endoscopy (ESGE) position statement. Endoscopy 52:899–923. https://doi.org/10.1055/a-1231-5123
Singh S, Sedlack RE, Cook DA (2014) Effects of simulation-based training in gastrointestinal endoscopy: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 12:1611-1623.e4. https://doi.org/10.1016/j.cgh.2014.01.037
Khan R, Plahouras J, Johnston BC et al (2019) Virtual reality simulation training in endoscopy: a Cochrane review and meta-analysis. Endoscopy 51:653–664. https://doi.org/10.1055/a-0894-4400
Ekkelenkamp VE, Koch AD, de Man RA, Kuipers EJ (2016) Training and competence assessment in GI endoscopy: a systematic review. Gut 65:607–615. https://doi.org/10.1136/gutjnl-2014-307173
Technology Committee ASGE, Goodman AJ, Melson J, Aslanian HR, Bhutani MS, Krishnan K, Lichtenstein DR, Navaneethan U, Pannala R, Parsi MA, Schulman AR, Sethi A, Sullivan SA, Thosani N, Trikudanathan G, Trindade AJ, Watson RR, Maple JT (2019) Endoscopic simulators. Gastrointest Endosc 90:1–12. https://doi.org/10.1016/j.gie.2018.10.037
Sedlack RE, Kolars JC, Alexander JA (2004) Computer simulation training enhances patient comfort during endoscopy. Clin Gastroenterol Hepatol 2:348–352. https://doi.org/10.1016/S1542-3565(04)00067-9
Ahlberg G, Hultcrantz R, Jaramillo E et al (2005) Virtual reality colonoscopy simulation: a compulsory practice for the future colonoscopist? Endoscopy 37:1198–1204. https://doi.org/10.1055/s-2005-921049
Finocchiaro M, Cortegoso Valdivia P, Hernansanz A et al (2021) Training simulators for gastrointestinal endoscopy: current and future perspectives. Cancers 13:1427. https://doi.org/10.3390/cancers13061427
King N, Kunac A, Merchant AM (2016) A review of endoscopic simulation: current evidence on simulators and curricula. J Surg Educ 73:12–23. https://doi.org/10.1016/j.jsurg.2015.09.001
Ahmed K, Aydin A, Dasgupta P et al (2015) A novel cadaveric simulation program in urology. J Surg Educ 72:556–565. https://doi.org/10.1016/j.jsurg.2015.01.005
Wyles SM, Miskovic D, Ni Z et al (2011) Analysis of laboratory-based laparoscopic colorectal surgery workshops within the English national training programme. Surg Endosc 25:1559–1566. https://doi.org/10.1007/s00464-010-1434-y
Danion J, Breque C, Oriot D et al (2020) La technologie SimLife® dans la formation du chirurgien. J Chir Viscérale 157:S119–S124. https://doi.org/10.1016/j.jchirv.2020.02.005
Faure JP, Breque C, Danion J et al (2017) SIM Life: a new surgical simulation device using a human perfused cadaver. Surg Radiol Anat 39:211–217. https://doi.org/10.1007/s00276-016-1715-9
Jones MW, Deere MJ, Harris JR et al (2017) Fabrication of an inexpensive but effective colonoscopic simulator. JSLS 21:e2017.00002. https://doi.org/10.4293/JSLS.2017.00002
Gages: a valid measurment tool for technical skills in flexible endoscopy—SAGES abstract archives. SAGES. Im Internet: https://www.sages.org/meetings/annual-meeting/abstracts-archive/gages-a-valid-measurment-tool-for-technical-skills-in-flexible-endoscopy/; Stand: 10.10.2021
Walsh C, Umar S, Ghassemi S et al (2020) Colonoscopy core curriculum. Gastrointest Endosc. https://doi.org/10.1016/j.gie.2020.06.054
Reumkens A, Rondagh EJA, Bakker CM et al (2016) Post-colonoscopy complications: a systematic review, time trends, and meta-analysis of population-based studies. Am J Gastroenterol 111:1092–1101. https://doi.org/10.1038/ajg.2016.234
Camus M, Jacques J, Mouel JL et al (2019) L’offre de formation initiale en simulation en endoscopie digestive en France. In Endoscopy. Georg Thieme Verlag KG, p. 000535
Jirapinyo P, Thompson CC (2015) Current status of endoscopic simulation in gastroenterology fellowship training programs. Surg Endosc 29:1913–1919. https://doi.org/10.1007/s00464-014-3884-0
Kim SC, Fisher JG, Delman KA et al (2016) Cadaver-based simulation increases resident confidence, initial exposure to fundamental techniques, and may augment operative autonomy. J Surg Educ 73:e33–e41. https://doi.org/10.1016/j.jsurg.2016.06.014
Balekuduru A, Appaji A (2021) Therapeutic endoscopic procedures on a human cadaver—a pilot feasibility study. J Dig Endosc 12:036–042. https://doi.org/10.1055/s-0041-1728223
Liu W, Zheng X, Wu R et al (2018) Novel laparoscopic training system with continuously perfused ex-vivo porcine liver for hepatobiliary surgery. Surg Endosc 32:743–750. https://doi.org/10.1007/s00464-017-5731-6
Ansell J, Mason J, Warren N et al (2012) Systematic review of validity testing in colonoscopy simulation. Surg Endosc 26:3040–3052. https://doi.org/10.1007/s00464-012-2332-2
Hill A, Horswill MS, Plooy AM, Watson MO, Karamatic R, Basit TA, Wallis GM, Riek S, Burgess-Limerick R, Hewett DG (2012) Assessing the realism of colonoscopy simulation: the development of an instrument and systematic comparison of 4 simulators. Gastrointest Endosc 75:631–640. https://doi.org/10.1016/j.gie.2011.10.030
Koch AD, Haringsma J, Schoon EJ et al (2008) A second-generation virtual reality simulator for colonoscopy: validation and initial experience. Endoscopy 40:735–738. https://doi.org/10.1055/s-2008-1077508
Moorthy K, Munz Y, Orchard TR, Gould S, Rockall T, Darzi A (2004) An innovative method for the assessment of skills in lower gastrointestinal endoscopy. Surg Endosc 18:1613–1619. https://doi.org/10.1007/s00464-004-9002-y
Acknowledgements
The investigators would like to thank the Université de Reims Champagne Ardenne for its intellectual support and the Anatomy Laboratory staff for their kindness and availability. The authors would also like to thank Daniela Pellot of the SERRA at Reims Faculty of Medicine for assistance with English language editing. All of the authors would like to sincerely thank the donors and their families.
Funding
None.
Author information
Authors and Affiliations
Contributions
AR: Conceptualization, Validation, Investigation, Resources, Data Curation, Writing—Original Draft, Writing—Review & Editing, Visualization, Project administration; CP: Conceptualization, Methodology, Validation, Writing—Review & Editing; AP: Validation, Writing—Review & Editing; IC: Validation, Writing—Review & Editing; ML: Writing—Review & Editing, YR: Conceptualization, Writing—Review & Editing; GC: Conceptualization, Validation, Resources, Writing—Review & Editing; MB: Conceptualization, Validation, Formal Analysis, Investigation, Resources, Data Curation, Writing—Original Draft, Writing—Review & Editing, Visualization, Supervision, Project administration.
Corresponding author
Ethics declarations
Disclosures
Cyril Perrenot received honoraria as a consultant for Medtronic, BD and Hartmann SA unrelated to this work. All other authors (Amélie Rohr, Anaïs Pitta, Isabelle Celerier, Marc Labrousse, Yohann Renard, Guillaume Cadiot, Mathias Brugel) have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
464_2022_9763_MOESM1_ESM.docx
Table 1A. Sociodemographic characteristics of the included population (extra)Abbreviations: n: number of participants, IQR: Interquartile range, h: hours
Table 1B. Previous experience of the included populationAbbreviations: n: number of participants, IQR: Interquartile range, GE: gastroenterology, h: hours, VR: virtual reality** Apprehension is assessed using a Likert scale from 1: strongly disagree to 7: strongly agree.
Table 2. Simulation realism survey (SRS) median item score for skilled participants. Scores are expressed as median (IQR). Abbreviations: IQR: Interquartile rangeEach of these parameters was measured using a Likert scale (1= strongly disagree, 4= neutral, 7= strongly agree). Technical difficulty fidelity was also measured with a Likert Scale (1= easier, 4= neutral, 7= harder than human living colonoscopy). Realism was defined as favorable when items were rated over or equal to 5 with an inter-quartile range (IQR) overlapping 4, and very favorable when rated over or equal to 5 with an inter-quartile range (IQR) excluding 4 (neutral). Technical difficulty fidelity was defined as ideal when equalling 4 or overlapping.
Table 3. Content validity survey (CVS) median item score for skilled participants. Scores are expressed as median (IQR). Abbreviations: IQR: Interquartile range. Each of these parameters was measured using a Likert scale (1= strongly disagree, 4= neutral, 7= strongly agree). Item was defined as favorable when rated over or equal to 5 with an inter-quartile range (IQR) overlapping 4, and very favorable when rated over or equal to 5 with an inter-quartile range (IQR) excluding 4 (neutral).
Table 4. NASA Task Load Index modified median item score per group Scores are expressed as median (IQR). Each item had a scale score from 1 (very low) to 20 (very high), except for the item “performance” where 1 is for “perfect” and 20 for “failure”.
Supplementary file1 (DOCX 1479 KB)
Fig. 1 Simulation Realism Survey form
Fig. 2 Content Validity Survey form
Fig. 3 NASA Task Load Index Modified form
Fig. 4 Bowel cleansing protocol
Supplementary file2 (MP4 63454 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rohr, A., Perrenot, C., Pitta, A. et al. Reperfused human cadaver as a new simulation model for colonoscopy: a pilot study. Surg Endosc 37, 3224–3232 (2023). https://doi.org/10.1007/s00464-022-09763-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09763-0