Abstract
Background
The very-low-voltage (VLV) mode in electrosurgery can stably and deeply energize tissues even if the local electrical resistance changes with energization. Therefore, in electrosurgical hemostasis, the VLV mode is more reliable than other coagulation modes. In clinical practice, the appropriate use of combined saline drip and blood suction under the VLV mode can further enhance coagulation ability. However, the detailed mechanism is not known. The current study aimed to evaluate the association between electrosurgical activation time (ET) and hemostatic tissue effect (HTE) under the VLV mode. Further, the effect of saline drip and suction on power consumption and HTE was validated.
Methods
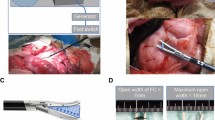
Twelve female pigs weighing 35 kg were included in the experiment. A liver hemorrhage model was established via an open abdominal procedure, and hemostasis in the hemorrhagic lesion was attempted using the VLV mode under different conditions (ET: 3, 6, 9, and 12 s, with/without saline drip and/or continuous suction). Electrical data (such as voltage, current, and resistance) during coagulation were extracted. Then, the vertical/horizontal extent of HTE was assessed, and the hemostasis outcome (successful or failed) was recorded.
Results
The vertical/horizontal HTE, power consumption, and integrated current value were positively correlated with the ET. The coagulation depth deepened with saline drip (p < 0.01). However, it was not affected by continuous suction (p = 0.20). The HTE area increased with saline drip (p < 0.01) and decreased with suction (p < 0.01). The power consumption and integrated current increased with saline drip (p < 0.01) and decreased with suction (p < 0.01). The success rate of hemostasis decreased with saline drip alone (31of 48 trials [success rate = 64.5%] in the saline drip group and 44/48 trials (success rate = 91.7%) in the control group). However, it improved with continuous suction (46/48 trials [success rate = 95.8%]).
Conclusion
The electrosurgical activation time was positively correlated with hemostatic tissue effect. Saline drip increased heat transfer efficiency but decreased the success rate of hemostasis. Therefore, the use of continuous suction in addition to saline drip increased hemostatic efficiency.




Similar content being viewed by others
References
Watanabe Y, Fuchshuber P, Homma T et al (2020) An unmodulated very-low-voltage electrosurgical technology creates predictable and ultimate tissue coagulation: from experimental data to clinical use. Surg Innov 27:492–498
Christensen MC, Dziewior F, Kempel A et al (2012) Increased chest tube drainage is independently associated with adverse outcome after cardiac surgery. J Cardiothorac Vasc Anesth 26:46–51
Smilowitz NR, Oberweis BS, Nukala S et al (2016) Association between anemia, bleeding, and transfusion with long-term mortality following noncardiac surgery. Am J Med 129:315-323.e312
Stokes ME, Ye X, Shah M et al (2011) Impact of bleeding-related complications and/or blood product transfusions on hospital costs in inpatient surgical patients. BMC Health Serv Res 11:135
Wu WC, Smith TS, Henderson WG et al (2010) Operative blood loss, blood transfusion, and 30-day mortality in older patients after major noncardiac surgery. Ann Surg 252:11–17
Shah A, Palmer AJR, Klein AA (2020) Strategies to minimize intraoperative blood loss during major surgery. Br J Surg 107:e26–e38
Overbey DM, Townsend NT, Chapman BC et al (2015) Surgical energy-based device injuries and fatalities reported to the food and drug administration. J Am Coll Surg 221:197-205.e191
Weiser TG, Haynes AB, Molina G et al (2016) Size and distribution of the global volume of surgery in 2012. Bull World Health Organ 94:201–209f
Watanabe Y, Kurashima Y, Madani A et al (2016) Surgeons have knowledge gaps in the safe use of energy devices: a multicenter cross-sectional study. Surg Endosc 30:588–592
Feldman L, Fuchshuber P, Jones D (2012) The SAGES manual on the fundamental use of surgical energy (FUSE)
Hirokawa F, Hayashi M, Miyamoto Y et al (2011) A novel method using the VIO soft-coagulation system for liver resection. Surgery 149:438–444
Ishiko T, Beppu T, Chikamoto A et al (2010) The comparison of efficacy in 3 different types of pre-coagulation method for endoscopic liver resection of hepatocellular carcinoma. J Microw Surg 28:47–51
Matsuoka A, Tate S, Nishikimi K et al (2018) Efficacy of soft coagulation in retroperitoneal lymphadenectomy for ovarian cancer. Gynecol Oncol 149:430–431
Hongo F, Kawauchi A, Ueda T et al (2015) Laparoscopic off-clamp partial nephrectomy using soft coagulation. Int J Urol 22:731–734
Miyazawa M, Aikawa M, Okada K et al (2018) Laparoscopic liver resection using a monopolar soft-coagulation device to provide maximum intraoperative bleeding control for the treatment of hepatocellular carcinoma. Surg Endosc 32:2157–2158
Okamoto K, Koyama I, Toshimitsu Y et al (2012) Liver resection using a soft-coagulation system without the Pringle maneuver. Hepatogastroenterology 59:875–877
Uchiyama A, Miyoshi K, Nakamura K (2011) VIO soft-coagulation system for major pulmonary resections: results in 68 patients with primary lung cancer. Gen Thorac Cardiovasc Surg 59:175–178
Tang RSY, Lau JYW (2019) Monopolar hemostatic forceps with soft coagulation: earning a place in the endoscopic hemostasis repertoire for peptic ulcer bleeding. Gastrointest Endosc 89:803–805
Takahashi Y, Saito A, Sakuma Y et al (2021) Treatment of air leakage using the VIO soft coagulation system: a mouse pulmonary air leak model. Surg Today. https://doi.org/10.1007/s00595-021-02251-3
Akita H, Takahashi H, Gotoh K et al (2015) Closure method for thick pancreas stump after distal pancreatectomy: soft coagulation and polyglycolic acid felt with fibrin glue. Langenbecks Arch Surg 400:843–848
Ikegami T, Maeda T, Kayashima H et al (2011) Soft coagulation, polyglycolic acid felt, and fibrin glue for prevention of pancreatic fistula after distal pancreatectomy. Surg Today 41:1224–1227
Furuta S, Ebizuka M, Kawabata S et al (2015) Effect of instillation of physiological saline in SOFT coagulation. Iryou kikigaku (The Japanese journal of medical instrumentation) 85:10–13
Katsuyama S, Miyazaki Y, Kobayashi S et al (2020) Novel, infection-free, advanced hemostatic material: physical properties and preclinical efficacy. Minim Invasive Ther Allied Technol 29:283–292
Hamada T, Nanashima A, Yano K et al (2017) Significance of a soft-coagulation system with monopolar electrode for hepatectomy: a retrospective two-institution study by propensity analysis. Int J Surg 45:149–155
Feldman LS, Fuchshuber P, Jones DB et al (2012) Surgeons don’t know what they don’t know about the safe use of energy in surgery. Surg Endosc 26:2735–2739
Madani A, Watanabe Y, Vassiliou MC et al (2014) Impact of a hands-on component on learning in the Fundamental Use of Surgical Energy™ (FUSE) curriculum: a randomized-controlled trial in surgical trainees. Surg Endosc 28:2772–2782
Fuchshuber P, Schwaitzberg S, Jones D et al (2018) The SAGES Fundamental Use of Surgical Energy program (FUSE): history, development, and purpose. Surg Endosc 32:2583–2602
Deguchi H, Tomoyasu M, Shigeeda W et al (2019) Usefulness of a suction ball coagulation probe for hemostasis in complete VATS lobectomy for patients with non-small cell lung cancer. Surg Today 49:580–586
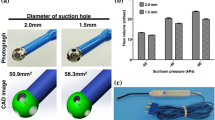
Takahashi H, Haraguchi N, Nishimura J et al (2018) A novel suction/coagulation integrated probe for achieving better hemostasis: development and clinical use. Surg Today 48:649–655
Acknowledgements
This research project benefited from the support and time of many individuals. We gratefully acknowledge the work of past and present members of our laboratory, S. Katsuyama, M. Kikkawa, K. Tanaka, and Y. Tsugita. This work was presented at the 30th Annual Congress of the EAES, Krakow, Poland, held on July 5–8, 2022.
Funding
This study did not receive specific funding.
Author information
Authors and Affiliations
Contributions
KN conceived the study. KN and YU designed the study. YU, KO, KA, and NB conducted data collection. YU wrote the initial draft of the manuscript. KO edited the supplementary movies. KN contributed to data interpretation and critical revision of the manuscript for important intellectual content. MH, KY, TS, KT, TM, TT, YK, HE, and YD contributed to data collection and interpretation and critical review of the manuscript. All authors have read and approved the final version of the manuscript and have agreed to the accountability of all aspects of the study, thereby ensuring that any queries related to the accuracy or integrity of any part of the work are answerable.
Corresponding author
Ethics declarations
Conflict of interest
Yuki Ushimaru, Kazuki Odagiri, Kazunori Akeo, Namiko Ban, Makoto Hosaka, Kotaro Yamashita, Takuro Saito, Koji Tanaka, Kazuyoshi Yamamoto, Tomoki Makino, Tsuyoshi Takahashi, Yukinori Kurokawa, Hidetoshi Eguchi, Yuichiro Doki, and Kiyokazu Nakajima have no conflicts of interest or financial ties to declare.
Statement of ethics
All procedures in this study were performed in accordance with the ethical standards of the responsible committee on institutional animal experimentation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 107137 KB)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ushimaru, Y., Odagiri, K., Akeo, K. et al. Efficacy of electrocoagulation hemostasis: a study on the optimal usage of the very-low-voltage mode. Surg Endosc 36, 8592–8599 (2022). https://doi.org/10.1007/s00464-022-09492-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09492-4